LAO Contact
February 13, 2024
The 2024‑25 Budget
Department of Developmental Services
Summary
The Department of Developmental Services (DDS) coordinates a wide variety of services for about 400,000 Californians with intellectual or developmental disabilities or similar conditions. In this brief, we provide background on DDS before describing and assessing the Governor’s 2024‑25 budget proposals for the department. The Governor’s budget proposes a new Master Plan for Developmental Services, as well as budget solutions, including a proposal to delay by one year the implementation of the final phase of service provider rate reform (with the next rate increase occurring July 1, 2025, rather than July 1, 2024).
Recognizing that the state has in recent years undertaken a wide variety of policy initiatives related to DDS, we also address ongoing oversight and implementation issues. In particular, we provide background and issues for legislative consideration on the following three issues: (1) funding directed in statute to direct care staff compensation increases, (2) service provider quality incentive payments, and (3) service disparities and the Coordinated Family Support Services pilot.
Background
Lanterman Act Lays Foundation for “Statutory Entitlement.” California’s Lanterman Developmental Disabilities Services Act (Lanterman Act) originally was passed in 1969 and substantially revised in 1977. It amounts to a statutory entitlement to services and supports for individuals ages three and older who have a qualifying developmental disability. Qualifying disabilities include autism; epilepsy; cerebral palsy; intellectual disabilities; and other conditions closely related to intellectual disabilities that require similar treatment, such as a traumatic brain injury. To qualify, an individual must have a disability that is substantial, expected to continue indefinitely, and which began before the age of 18. There are no income‑related eligibility criteria. As of December 2023, DDS serves about 360,000 Lanterman‑eligible individuals and another 8,000 children ages zero through four who are provisionally eligible.
California Early Intervention Services Act Ensures Services for Eligible Infants and Toddlers. DDS also provides services via its Early Start program to any infant or toddler under the age of three with a qualifying developmental delay or who are at risk of developmental disability. There are no income‑related eligibility criteria. As of December 2023, DDS serves about 56,000 infants and toddlers in the Early Start program.
Regional Centers Coordinate and Pay for Individuals’ Services. DDS contracts with 21 nonprofit regional centers, which coordinate and pay for the direct services provided to “consumers” (the term used in statute). Services are delivered by a large network of private for‑profit and nonprofit providers. In addition to state General Fund and some smaller funding sources, these services are purchased in part through federal funding obtained through the Medicaid Home‑ and Community‑Based Services (HCBS) waiver. The HCBS waiver provides Medicaid funding for eligible individuals to receive services and supports in their home and community‑based settings, rather than in institutions.
State Recently Began Implementing a Major Overhaul of Service Provider Rates. For decades, the state paid DDS direct care staff (sometimes referred to as direct service professionals) according to a rate structure deemed by the Legislature to be outdated and overly complicated. In an attempt to modernize and rationalize this structure, the Legislature passed legislation to authorize DDS to commission a study of service provider costs to guide the development of a new rate structure. This study—commonly referred to as “the rate study”—was published in January 2020. The 2021‑22 budget initiated a five‑year plan to phase in that study’s rate models. The 2022‑23 budget accelerated this phase in to become a four‑year plan, with full implementation of the new rate system scheduled for July 1, 2024. Budget‑related legislation to implement the accelerated phase‑in plan requires providers to use a specified percentage of rate increases to raise the wages, salaries, or benefits of direct care staff.
Once Fully Implemented, Rate Reform Must Include New Quality Incentive Structure. Following full implementation of the new rate system, statute requires that 10 percent of each service provider rate be reserved for a “quality incentive payment.” These payments are to be tied to performance metrics specific to each category of provider. These metrics and associated standards are to be determined by a workgroup of stakeholders led by DDS. (Prior to the full implementation of the quality incentive payment as 10 percent of the total rate, the state began providing some smaller quality incentive payments on top of providers’ baseline rates in 2022‑23.)
Proposals
Overview
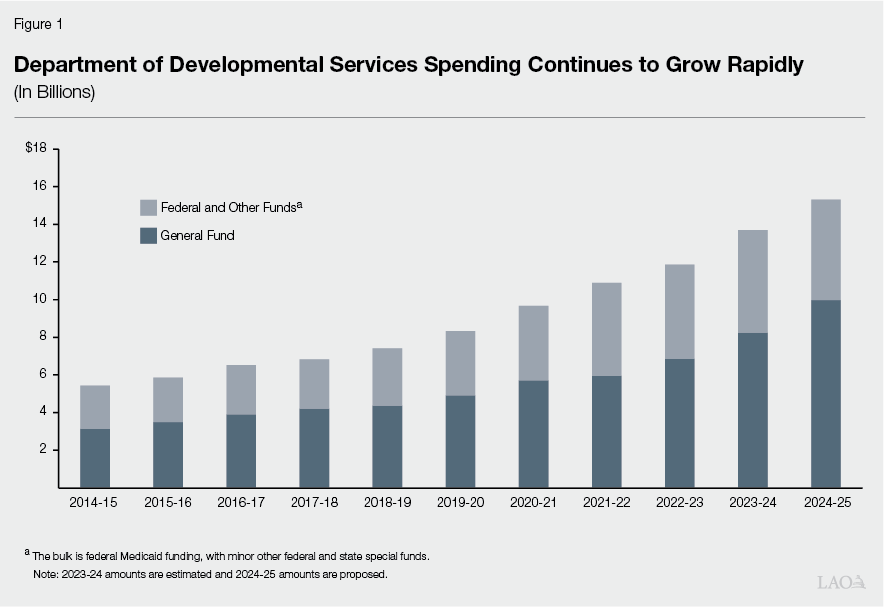
Proposed Budget Reflects Significant Growth. The Governor’s budget proposal includes $15.3 billion total funds in 2024‑25, up $1.6 billion (12 percent) over the revised 2023‑24 level ($13.7 billion). Of the proposed 2024‑25 total, $10 billion is from the General Fund, up $1.7 billion (21 percent) over the revised 2023‑24 level ($8.2 billion General Fund). This significant year‑over‑year growth in overall DDS spending follows the spending growth trend over the past ten years, as shown in Figure 1. The average annual growth rate in total funds over the past ten years is about 11 percent. Primary drivers of the year‑over‑year General Fund growth include rising caseload and increased utilization of services. The administration’s caseload projection is consistent both with our office’s projection and with longstanding trends. (The relatively higher growth rate in General Fund costs in 2024‑25 is due to the expiration of pandemic‑era federal funds.)
Delay Full Implementation of Service Provider Rate Reform
Background
Rate Reform Intended to Increase Rates for Service Providers. The rate study initiated in 2016 was undertaken, in part, because the historical rate structure did not result in funding levels for service providers that kept pace with system growth or supported an adequate supply of providers. (A series of rate freezes and rate reductions—beginning in the early 2000s as budget solutions—meant that the rates had not kept up with rising costs over time.) The funding first allocated in 2021‑22 was intended to raise funding levels for service providers by increasing service provider rates. These rates fund the wide variety of services and supports that service providers deliver to DDS consumers, including residential services, day programs, employment support, independent and supported living, and personal assistance.
Service Provider Rate Reform Implementation Time Line Has Changed in Recent Years. The original plan for service provider rate reform established a five‑year implementation time line starting in 2021‑22. Under this plan, the final rate adjustment would occur in 2025‑26. The original time line included the following steps:
- Year 1 (2021‑22). Service provider rates increase beginning April 1, 2022. Rate increases equal one‑quarter of the difference between a provider’s current rate and what the fully funded rate model (as of 2021‑22) would be according to the rate study.
- Year 2 (2022‑23). The previous year’s rate increase is annualized and DDS implements the first stage of the quality incentive program.
- Year 3 (2023‑24). The cumulative total of this rate increase and the previous increase equals one‑half of the difference between the provider’s rate as of March 30, 2022 (before the first rate increase took effect) and the fully funded rate model. Additional funding is provided for the quality incentive program.
- Year 4 (2024‑25). Rates will sustain the previous years’ changes.
- Year 5 (2025‑26). Rate models will be fully funded beginning July 1, 2025 as follows: A service provider’s base rate will equal 90 percent of its rate model, while up to 10 percent of its rate model will be available as incentive payments if the provider achieves its performance and outcomes targets.
The 2022‑23 budget accelerated the implementation time line from five to four years by eliminating the step planned for Year 4 under the original time line. The accelerated time line included the following steps:
- Year 1 (2021‑22) to Year 3 (2023‑24). Same as original plan.
- Year 4 (2024‑25). Rate models will be fully funded beginning July 1, 2024 as follows: A service provider’s base rate will equal 90 percent of its rate model, while up to 10 percent of its rate model will be available as quality incentive payments if the provider achieves specified performance and outcome targets.
Rate Reform Acceleration Responded to Concerns About Workforce Shortages. The state adopted this acceleration in response to stakeholder concerns about a workforce shortage of direct care staff. Stakeholders proposed the acceleration because providers faced challenges filling vacancies for direct care staff positions. Stakeholders stated that the accelerated time line would facilitate hiring of direct care staff.
Proposal
The Governor’s budget proposes to delay the final stage of service provider rate reform implementation by one year to 2025‑26. Under the proposal, rate models would be fully funded as of July 1, 2025, rather than July 1, 2024. The proposal provides $612.5 million in General Fund savings in 2024‑25. The reduction in General Fund spending would also reduce federal reimbursements by $408 million, resulting in a total reduction of about $1 billion from planned spending in 2024‑25.
In addition to delaying the final rate increase, the proposal would also affect the implementation of quality incentive payments. Under the proposal, quality incentive payments would comprise 10 percent of the fully funded rate model beginning in 2025‑26, rather than in 2024‑25 (as under current law). In lieu of calculating quality incentive payments as 10 percent of the rate model in 2024‑25, the Governor’s budget proposes $137.5 million total funds as separate funding for a quality incentive program. This proposed amount is equal to the estimated amount of funding spent on quality incentives in the current fiscal year.
Assessment
Proposal Would Help Address the State Budget Problem… The $612.5 million decrease in General Fund spending for rate reform implementation would help the state address its budget deficit in 2024‑25. (There are proposed budget solutions across many other programs as well. Our recent publication, The 2024‑25 Budget: Overview of the Governor’s Budget, provides more information on the state’s budget problem and the overall package of proposed budget solutions.) The delay would mean the rate model implementation would remain roughly half‑way implemented in 2024‑25.
…But Could Delay Addressing Direct Care Staff Workforce Shortages. We have heard concerns from stakeholders that the challenges faced by providers in hiring an adequate number of direct care staff, which helped initiate rate reform acceleration in 2022‑23, have not yet been fully overcome. Providers indicate that a continuing shortage of direct care staff could delay service provision to DDS consumers, as providers might have to decline referrals from regional centers due to lack of available staff. Consumers might therefore need to wait longer before a provider can begin to serve them. Additionally, a continuing shortage of direct care staff could disrupt service continuity for those consumers who are successfully referred to a provider due to staff scheduling challenges. We note that DDS has recently adopted workforce initiatives that could improve workforce stability in the longer run, such as bilingual pay differentials and Direct Service Professionals University (a training and certification program tied to wage differentials for direct care staff). However, as these efforts are still in the early stages of implementation or not yet fully implemented, they are unlikely to address providers’ immediate workforce needs in 2024‑25.
Issues for Legislative Consideration
Consider Whether Alternative Approaches Are Warranted. While the proposal would help address the state budget problem, it involves trade‑offs. Specifically, some DDS consumers may not receive services as quickly as could be possible were the full rate reform implemented in 2024‑25. Rejecting the administration’s proposal, however, requires dollar‑for‑dollar reductions in other areas of the budget. Alternatively, the Legislature could consider a scaled‑back budget solution that allows some level of funding for the final phase of rate reform in 2024‑25 while reducing the adverse impacts associated with the proposed solution. For example, such a scaled‑back approach could target select service provider codes where the workforce shortages are most acute. This approach would require collaboration with the administration and stakeholders. Additionally, it would still require alternative budget solutions in other areas of the budget (although of a lesser dollar amount than would be required if the administration’s proposal were rejected completely). We note that delaying the final phase of rate reform is only a one‑year budget solution. That is, the ongoing costs of the final phase of rate reform are reflected in the administration’s multiyear estimates beginning in 2025‑26 (when the state continues to face budget deficits).
Master Plan for Developmental Services
Proposal
The Governor’s budget proposes DDS develop a Master Plan for Developmental Services by the end of calendar year 2024. The stated goal of the plan is broadly to improve the experience of individuals and families receiving developmental services. The plan would outline goals to make developmental services more person‑centered, equity‑focused, and data‑driven. To inform the development of the plan, DDS intends to reconstitute the Developmental Services (DS) Task Force (originally created in 2014 to inform the transition of DDS consumers from institutional settings to home‑ and community‑based settings). The California Health and Human Services Agency identified the Master Plan for Developmental Services as one of its 2024‑25 program priorities. There is no new funding associated with this proposal.
Assessment and Issues for Legislative Consideration
In Concept, Proposal Appears Consistent With Existing Priorities… DDS is developing and has initiated various efforts intended to address quality, equity, outcomes, and accountability. These efforts include, among others, service provider quality incentive payments, implicit bias training at regional centers, efforts to expand consumers’ access to social recreation services, and standardized assessments for respite services. While these efforts have not yet been evaluated for efficacy or efficiency, they are meant to improve the experience of individuals and families receiving developmental services. As such, the proposed Master Plan therefore appears consistent with the department’s existing efforts and stated priorities.
…But Details Provided to Date Are Scarce. At the time this analysis was prepared, the administration had not yet released substantive details of its proposal for the Master Plan for Developmental Services. Particularly given the current fiscal climate, understanding the potential scope and outcomes of this proposal is important. Depending on the specifics of the plan, it could create fiscal pressure on the Legislature to take certain budget and policy actions in coming years. Accordingly, throughout this section, we raise key questions for the administration in order for the Legislature to fully consider the merits of the proposal.
State Has Recent Experience With Master Planning Process. The concept of a master plan has a recent precedent in the state, as California developed a Master Plan for Aging throughout 2019 and 2020. The Governor issued an executive order in June 2019 calling for the Master Plan for Aging in response to anticipated demographic shifts in the state’s aging population. In response, the Legislature enacted legislation (Chapter 742 of 2019 [SB 228, Jackson]) establishing the parameters and reporting requirements of the plan. The development of the Master Plan for Aging involved significant stakeholder and public engagement as well as cross‑agency collaboration. The final plan, released in 2021, identifies 5 goals and 23 strategies with a targeted implementation date of 2030. Six standing stakeholder committees inform the ongoing implementation of the plan.
The Master Planning Process Has Potential Value. While the Master Plan for Aging is still in the early stages of implementation and evaluation, it nonetheless sheds light on the possibilities for developing a master plan. A master plan can serve to focus and coordinate state efforts in a broad policy area that cuts across multiple state entities, initiated by a process of setting priority goals and developing an implementation plan to achieve the goals. For example, the Master Plan for Aging’s five main goals address housing, health, community integration, caregiving, and economic security. The administration has taken various actions to start implementing the Master Plan for Aging, such as investing funds to construct or rehabilitate senior housing facilities through the California Department of Social Services’ Community Care Expansion Program, as well as expanding food benefit eligibility for older adults as part of Food4All.
Legislature Has Opportunity to Inform the Vision for the Master Plan for Developmental Services. At the time this analysis was prepared, the administration has not clearly articulated a definitive vision for the Master Plan for Developmental Services. This presents an opportunity for the Legislature to help establish the vision for both the development of the Master Plan and the plan’s scope in the context of developmental services more broadly. Should the Legislature wish to proceed with the concept of a Master Plan for Developmental Services, we recommend that the Legislature consider introducing legislation, similar to that introduced for the Master Plan for Aging to ensure that the vision for the Master Plan for Developmental Services reflects legislative priorities. Questions to ask the administration could include: Why is DDS proposing to create a Master Plan now? Is a Master Plan the most appropriate vehicle to achieve the department’s goals? Which types of developmental services would the Master Plan affect? How would the department ensure that any programs resulting from the Master Plan are inclusive of the diverse array of individuals served in the developmental services system? How would the Master Plan expand upon the department’s existing initiatives to address quality, equity, outcomes, and accountability?
While DDS indicated that it intends to collaborate with other state departments and programs on the Master Plan for Developmental Services, it has not yet released any details on its vision for this type of collaboration. Individuals with intellectual and developmental disabilities often receive services outside of DDS, including those overseen by the California Department of Education, the Department of Rehabilitation, the Department of Health Care Services, and the Department of Social Services. We recommend that the Legislature ask DDS to provide more information about its plans for collaboration across state agencies. Questions to ask the administration could include: Which state agencies and departments would be involved in the development and implementation of the Master Plan? How would DDS ensure successful and efficient interagency coordination? Would DDS seek to create a Cabinet Work Group, similar to the group created for the Master Plan for Aging?
More Details Needed on Stakeholder Engagement. While the department stated that it plans to convene a workgroup of stakeholders to inform the development of the Master Plan, it has not released details on the stakeholder engagement process. Chapter 742—concerning the Master Plan for Aging—specified requirements for the solicitation of stakeholder input. The Legislature could consider codifying a similar requirement for the Master Plan for Developmental Services.
Relatedly, stakeholders have voiced the importance of giving a diverse representation of consumers the opportunity to meaningfully engage in the development of the Master Plan. We recommend the Legislature ask DDS to provide more information about its intended outreach to stakeholders and the role that stakeholders would play in developing the Master Plan. Questions to ask the administration could include: Does the department plan to solicit participation from consumers that historically have lower levels of service provision/purchase of service expenditures? How would DDS make the stakeholder process accessible in multiple languages? How would DDS encourage participation of family members that represent a wide range of consumer ages, from Early Start to elderly consumers? How would DDS educate laypeople about the developmental services system so that they are sufficiently empowered to provide meaningful feedback? Would meetings be structured to allow stakeholders sufficient time to voice their concerns and suggestions?
Legislature Will Likely Need to Give Fiscal Considerations a Key Focus. In the context of likely budget deficits through 2027‑28, understanding the potential fiscal impacts of the proposed Master Plan would be critical. To understand these potential impacts, the Legislature could ask the administration how it proposes to estimate the implementation costs of the Master Plan and fund any costs above current baselines. The Legislature may want to consider the potential future cost pressures of the administration’s proposal as it evaluates the proposal and weighs it against other legislative funding priorities.
Proposal Does Not Address Ongoing Legislative Oversight of Plan Implementation. At the time this analysis was prepared, DDS has not indicated whether the Legislature would have any role in overseeing the ongoing implementation of the Master Plan once it is developed. We note that Chapter 742 required the Department of Aging to submit annual reports to the Legislature on the implementation of the Master Plan for Aging. The Legislature could consider codifying a similar requirement for the Master Plan for Developmental Services. The information from such reporting could assist the Legislature in exercising ongoing oversight through its appropriations authority and review of administration spending plans. The Legislature could also ask DDS to elaborate on its plan to track ongoing implementation. Questions could include: How would DDS plan to define success and track progress under the Master Plan? How would DDS plan to record and analyze data under the Master Plan? What role would stakeholders play in Master Plan implementation? How would the department ensure its goals are sufficiently specific to be tied to measurable outcomes? How would the department ensure financial transparency in its ongoing implementation tracking and reporting?
Delay Preschool Inclusion Grants
Proposal Is in Addition to Previous Two‑Year Delay. The 2022‑23 budget package included $10 million General Fund of ongoing funding for grants to enable preschool programs to include more children with exceptional needs. The Governor proposes delaying the implementation of this program until 2026‑27. In last year’s analysis, we raised several issues with the design of these grants; all of these concerns still apply. Given that the Governor’s budget projects multiyear deficits (in addition to the current budget problem), the Legislature may wish to consider eliminating this program (which has not yet been implemented).
DDS Oversight Issues
In recent years, the DDS system has undergone some significant changes that warrant continued legislative oversight. Below, we highlight three areas of particular interest for the Legislature. For each, we provide background and updates on the implementation of recent initiatives. We also raise issues for legislative consideration.
Direct Care Staff Compensation Increases
Background
Rate Reform Acceleration Intended to Benefit Direct Care Staff. When the 2022‑23 budget accelerated the phase in of service provider rate reform implementation, the associated trailer legislation required providers to use a specified percentage of the upcoming rate increases to raise the wages, salaries, or benefits of direct care staff starting on January 1, 2023 (Chapter 49 of 2022 [SB 188, Committee on Budget]). The percentage of the rate adjustment that must be allocated to the direct care staff varies by service code. The phase‑in plan also requires providers who receive a rate increase to maintain documentation demonstrating compliance with this requirement.
Issues
Compliance With Compensation Increases for Direct Care Staff. While DDS issued guidance to remind providers about the compliance requirement, the department indicated that it has not yet initiated any provider audits. This is in part because expenditures for 2022‑23 are not yet finalized. DDS stated that providers’ compliance with this requirement is a potential candidate for future audits. Given the significant amount of funding provided for rate reform implementation to date, these types of audits could help ensure that any funding allocated to rate reform implementation aligns with legislative intent. The Legislature could therefore ask DDS when it plans to conduct this type of audit and request a briefing on the findings once complete. The Legislature could also ask DDS to elaborate on how it coordinates with regional centers on this issue.
Service Provider Rate Reform: Quality Incentives
Background
Quality Incentives Will Ultimately Comprise 10 Percent of Provider Rates. Once service provider rate reform is fully implemented, statute requires that 10 percent of each service provider rate is reserved for a quality incentive payment. These quality incentive payments will be tied to performance metrics specific to each category of service provider. By tying payments to performance, the department aims to improve consumer outcomes. DDS convened a Quality Incentive Program Stakeholder Workgroup to help develop the methodology for quality incentive payments. (We provided additional background on and assessment of the status of the development of the quality incentive program in a previous analysis.)
Department Has Initiated Provider Directory. The department has started the process to create a statewide database containing contact details for all service providers authorized to serve DDS consumers. Prior to this, the department did not maintain comprehensive contact details for providers. The department indicated that the directory will help facilitate the quality incentive process by providing access to current and complete provider data. As of December 2023, the department is engaging with regional centers and service provider focus groups, as well as a contractor, to support provider directory rollout and training.
Issues
Infrastructure Needed to Support Quality Incentive Program Still Under Development. Although the administration views the provider directory as a valuable and necessary starting point for quality incentives, we have heard concerns from stakeholders that two other components of the infrastructure needed to fully implement quality incentive payments by 2025‑26 is lagging.
First, DDS needs to define the quality measures that providers must satisfy in order to earn the final 10 percent of the fully implemented rate model. Stakeholders have expressed concerns with the slow pace of progress in reaching consensus on quality measures and the need for more urgency within the department. Although the department indicated that it expects to receive support from regional centers and provider associations in communicating its quality measures before they take effect, limited time now remains before the quality measures must be finalized and published.
Second, the department requires an information technology (IT) system that will enable all 21 regional centers to consistently track whether providers have satisfied the quality criteria to earn the final 10 percent of the rate model. DDS has initiated a project with the California Department of Technology that would modernize case management and financial recordkeeping throughout the state. Once fully operational, this project would allow DDS and regional centers to leverage outcome measurements when calculating rates. At the time this analysis was prepared, whether this project would be completed in time for DDS to implement quality incentive payments is unclear.
In light of these potential challenges, the Legislature could ask DDS to provide more information at budget hearings about the anticipated time line for finalizing quality measures and upgrading the department’s IT systems as both of these components would be required to implement the measures.
Service Disparities and Coordinated Family Support Services
Background
Longstanding Interest in Spending Disparities Among Racial/Ethnic Groups. Starting in 2011‑12, state law requires all regional centers to periodically publish data on the amount spent on services for consumers disaggregated by the race/ethnicity of these consumers. These data consistently have shown large disparities in the average amounts spent among these groups. In particular, spending for Hispanic/Latino consumers is about half that for white consumers on average. (We raised concerns about spending disparities in a previous analysis, which provides additional context on this topic.)
Coordinated Family Support Pilot Intended to Help Identify and Address Disparities. DDS reports that adult Hispanic/Latino consumers are more likely than white consumers to live at home and thus consume fewer residential services. While this could be one contributing factor to lower spending levels for Hispanic/Latino consumers, the circumstances of living at home could mask service needs that are not being met. In response to this spending disparity, DDS created a pilot program for Coordinated Family Support targeted at the population of consumers 18 years and older who choose to live in their family homes. Services provided through the Coordinated Family Support pilot are intended to be tailored to each family’s unique needs and to respect the language and culture of each family. The department utilized funding for HCBS under the American Rescue Plan Act (ARPA) to help fund the pilot. The expenditure deadline for all HCBS ARPA activities is December 31, 2024.
Department Stated Intent to Collect Data on Pilot. The department stated in 2023 that regional center service coordinators are responsible for distributing an experience questionnaire to consumers and families receiving Coordinated Family Support. Service coordinators must then submit questionnaire responses to the department. Additionally, the department stated that regional centers must submit quarterly reports on pilot implementation.
Issues
Evaluation Would Reveal Outcomes From the Pilot and Provide Opportunities for Legislative Oversight. Once the pilot concludes, a program evaluation would be warranted to assess whether the pilot sheds light on the service disparities for Hispanic/Latino consumers and potential opportunities to reduce them. The department has not yet announced an end date for the pilot. For now, the department indicates that it is still implementing the pilot and approving service providers to provide Coordinated Family Support services. To assess whether additional General Fund spending on these services—or other policy actions—could be warranted in future budgets, we recommend that the Legislature ask DDS to provide more details on its plan to evaluate the pilot. Based on the evaluation, the Legislature could consider whether the pilot merits continuation and any potential modifications to improve efficacy. Questions the evaluation could include are: Did the pilot identify gaps in consumers’ service needs? Did participants consume more services as a result? Do the department’s findings suggest that spending disparities are driven by barriers consumers have faced in the developmental services system? Were there a sufficient number of providers approved to provide Coordinated Family Supports?
