February 12, 2015
The 2015-16 Budget:
Analysis of the Health Budget
Overview of Health Budget. The Governor’s budget proposes $21 billion from the General Fund for health programs—a 5 percent increase above 2014–15 estimated expenditures. For the most part, the year–over–year changes reflect implementation of previously enacted policy changes as well as changes in caseload, utilization of services, and costs as opposed to new policy proposals. The Governor’s budget proposal for health programs reflects significant fiscal uncertainty in a number of programmatic areas related to federal actions. For example, the President’s recent executive action on immigration would have a highly uncertain fiscal impact on health programs.
Programmatic and Spending Trends Since 2007–08. Our review of trends in the major health programs since 2007–08 (the last budget developed before the most recent recession) finds that total spending is up by 94 percent. By far the largest factor accounting for this growth in total spending is the increase in federal funding of $37.2 billion, in part reflecting the enhanced federal share of costs for the Medi–Cal expansion population under the federal Patient Protection and Affordable Care Act (ACA), also known as federal health care reform. While funding for some program reductions made during recessionary times has been fully or partially restored, other program reductions remain today. In addition, the Legislature has made some health program augmentations since 2007–08, mainly related to ACA implementation.
Proposed Restructuring of Managed Care Organization (MCO) Tax. A letter from the federal Centers for Medicare and Medicaid Services indicates that taxes structured like California’s existing MCO tax are inconsistent with federal Medicaid law and regulations, thereby putting over $1 billion in federal funding to the state at risk in future years if the tax were extended in its current form. The Governor proposes a new MCO tax structure intended to comply with federal requirements while funding two objectives: (1) restoring service hours previously reduced in the In–Home Supportive Services Program and (2) maintaining the General Fund offset from the current impermissible tax. We find the Governor’s proposed MCO tax would likely meet federal requirements, but note that in doing so, the proposal would in part resemble an actual tax on commercial health coverage (in addition to being a typical Medi–Cal financing scheme to leverage federal funding), with broader economic and social implications. While we recommend the Legislature adopt core features of the Governor’s proposal by August 2015, we find that permanent authorization of the proposal in its current form is not warranted.
Federal Funding for Children’s Health Insurance Program (CHIP) Uncertain. The amount of federal CHIP funding available in 2015–16 is uncertain, pending actions by Congress to appropriate additional funds for CHIP beyond September 30, 2015. Further, the longer–term future of CHIP remains uncertain as the federal government weighs the potential for transitioning children currently covered by CHIP into other sources of health coverage, such as subsidized coverage through Covered California. We recommend the Legislature begin weighing various options for children’s coverage should CHIP be discontinued.
Additional Capacity in Department of State Hospitals May Be Unnecessary. The Governor’s budget includes several proposals—including a $35.5 million capital outlay project—to expand treatment capacity for incompetent to stand trial patients in state hospitals. We find that the proposed increase in capacity may be unnecessary given recent policy changes and the department’s existing capacity. We recommend the Legislature not approve funding for the proposed capacity and request additional information from the department justifying the need for it in light of these concerns. To the extent the Legislature finds additional capacity to be necessary, we recommend the Legislature prioritize the most cost–effective options for providing services. We recommend that the Legislature reject the proposed capital outlay project due to its high cost.
Department of Public Health Licensing and Certification (L&C). Recent incidents of inconsistent and inadequate oversight, monitoring, and enforcement of L&C standards for health facilities have gained the attention of the media and the Legislature. In response, the Governor’s budget plan includes four proposals to take steps to improve the quality of the L&C Program and increase L&C staffing. We find the Governor’s approach of adding more resources to the L&C Program makes sense in order to address the backlog of L&C workload and complaint investigations. However, a key report from the administration is overdue, and without the report, the Legislature is not in a position to determine whether the Governor’s proposals are the most cost–effective approach to addressing workload backlog issues.
California’s major health programs provide a variety of health benefits to its citizens. These benefits include purchasing health care services, such as primary care, for qualified low–income individuals, families, and seniors and persons with disabilities (SPDs). The state also administers programs to prevent the spread of communicable diseases, prepare for and respond to public health emergencies, regulate health facilities, and achieve other health–related goals.
The health services programs are administered at the state level by the Department of Health Care Services (DHCS), Department of Public Health (DPH), Department of State Hospitals (DSH), the California Health Benefit Exchange (known as Covered California or the Exchange), and other California Health and Human Services Agency (CHHSA) departments. The actual delivery of many of the health care services provided through state programs often takes place at the local level and is carried out by local government entities, such as counties, and private entities, such as commercial managed care plans. (Funding for these types of services delivered at the local level is known as “local assistance,” whereas funding for state employees to administer health programs at the state level and/or provide services is known as “state operations.”)
Overview of Health Budget Proposal. The Governor’s budget proposes $21 billion from the General Fund for health programs. This is an increase of $992 million—or 5 percent—above the revised estimated 2014–15 spending level, as shown in Figure 1.
Figure 1
Major Health Programs and Departments—Budget Summary
General Fund (Dollars in Millions)a
|
|
2013–14 Actual
|
2014–15 Estimated
|
2015–16 Proposed
|
Change From 2014–15
|
|
Amount
|
Percent
|
|
Medi–Cal—Local Assistance
|
$16,488
|
$17,843
|
$18,610
|
$767
|
4.3%
|
|
Department of State Hospitals
|
1,463
|
1,563
|
1,576
|
13
|
0.8
|
|
Department of Public Health
|
115
|
120
|
124
|
4
|
3.3
|
|
Other Department of Health Care Services programs
|
60
|
169
|
268
|
99
|
58.6
|
|
High–cost medicationsb
|
—
|
100
|
200
|
100
|
100.0
|
|
Emergency Medical Services Authority
|
7
|
8
|
8
|
—
|
—
|
|
All other health programs (including state support)c
|
166
|
159
|
168
|
9
|
5.7
|
|
Totals
|
$18,299
|
$19,962
|
$20,954
|
$992
|
5.0%
|
Summary of Major Budget Proposals and Changes. The year–over–year increase of $992 million General Fund over the estimated 2014–15 spending level is largely comprised of increased expenditures in three areas. (We discuss each of these increases in more detail later in this report.)
- Medi–Cal Local Assistance. The net year–over–year increase in Medi–Cal local assistance of $767 million General Fund is due to several factors—including caseload adjustments, changes in benefits and utilization, and technical adjustments.
- High–Cost Drugs. The budget plan provides $100 million General Fund in 2014–15 and $200 million in 2015–16 to pay for new drugs used to treat Hepatitis C. These funds are not allocated to specific departments or programs, but are reserved for the state’s costs in treating some individuals infected with Hepatitis C—including inmates in state prisons, patients in state hospitals, and Medi–Cal and AIDS Drug Assistance Program beneficiaries.
- Backfill Reduced Federal Funds for Certain DHCS Family Health Programs. In response to an anticipated reduction in federal funds (used to support certain state–only programs) resulting from the expiration of the state’s current Section 1115 Medicaid waiver in October 2015, the budget plan proposes to increase General Fund support for the California Children’s Services program by $59 million and the Genetically Handicapped Persons Program by $51 million.
Budgetary Uncertainty Due to Federal Actions. The Governor’s budget proposal for health programs reflects significant fiscal uncertainty relating to federal actions in a number of programmatic areas. We describe the major uncertainties in Figure 2 and discuss them in greater detail later in this report.
Figure 2
Health Programs Budgetary Uncertainty Related to Federal Actions
|
Issue
|
Budgetary Uncertainty
|
|
Presidential executive action on immigration
|
If the President’s executive action is implemented, some undocumented immigrants may newly qualify for state health programs, including full–scope Medi–Cal. The potential cost increase to the state’s health services programs is highly uncertain.
|
|
Renewal of Medi–Cal managed care organization (MCO) tax
|
The state currently imposes a 3.9 percent tax on Medi–Cal MCOs’ gross receipts. This tax is used to leverage federal Medicaid funding. Recent federal guidance indicates that California’s tax on MCOs is inconsistent with federal Medicaid regulations and advised California—by no later than the end of this legislative session—to make changes to bring its tax structure into compliance. The budget assumes a General Fund offset from the tax of $803 million in 2014–15 and $1.1 billion in 2015–16. The budget would address this uncertainty by proposing a replacement tax that would comply with federal law.
|
|
Medi–Cal Section 1115 waiver renewal
|
California’s current Medi–Cal Section 1115 waiver, “Bridge to Reform,” expires in October 2015. The Department of Health Care Services will seek a five–year renewal of the waiver to continue to support implementation of the Patient Protection and Affordable Care Act (ACA), also known as federal health care reform, and other programmatic goals. The budget assumes continuation of some of the funding available in the current waiver. However, the federal Centers for Medicare and Medicaid Services has indicated that some funding, such as federal fund support for certain state–only health programs, is unlikely to continue.
|
|
Federal reauthorization of Children’s Health Insurance Program (CHIP) funding
|
Currently, federal funding for CHIP is only appropriated through federal fiscal year (FFY) 2015 which ends September 30, 2015, but ACA authorizes a higher level of CHIP federal funding beginning in FFY 2016. Congress must appropriate additional funds to continue CHIP and provide this higher level of funding. The budget assumes federal funding for CHIP will continue at the current level in 2015–16.
|
Members of the Legislature have expressed interest in the issue of the level of the state’s spending on health programs today compared to pre–recession levels (the 2007–08 state budget was the last budget developed before the recent recession). As with all areas of the budget, significant General Fund budget reductions were made in the health area to help balance the budget during the recessionary years. This section is intended to provide information to the Legislature to be able to make a meaningful comparison between (1) the state’s spending and programmatic service/benefit levels in health programs in the 2007–08 budget and (2) the level of spending and programmatic service/benefit levels for such programs proposed in the 2015–16 Governor’s Budget. We discuss caseload trends, changes in how programs are funded, changes in eligibility and service/benefit levels, and other drivers, such as federal policy changes—all of which help explain the difference between 2007–08 and 2015–16.
California’s state–federal Medicaid program, known as Medi–Cal, is a major source of health coverage for millions of Californians, and is by far the largest state–administered health program in terms of annual caseload and expenditures. Medi–Cal has undergone a major programmatic transformation as a result of the Patient Protection and Affordable Care Act (ACA), that has resulted in a major influx of new federal funding to provide health coverage to a newly eligible Medi–Cal population. There has also been some expansion of Medi–Cal health benefits under ACA. Throughout this section, as we discuss these various changes to Medi–Cal, we assume some basic familiarity with the program’s financing and delivery. To obtain this background information, see the “Medi–Cal” section of this report.
As shown in Figure 3, when all funding sources flowing through the state budget are considered (including federal funds), total spending in health programs has grown by 94 percent between 2007–08 and the Governor’s 2015–16 budget proposal. In real (inflation–adjusted) terms, total spending in health programs has grown by 75 percent from 2007–08 to 2015–16. Total spending was adjusted for inflation using the gross domestic product price index. This adjusts for economywide inflation, providing an indication of how the amount of state and federal resources devoted to spending in health programs has changed from 2007–08 to 2015–16 in real dollars. This adjustment does not account for many other factors specific to health spending, such as the population served, benefit design, technological changes, and the growth in health care prices above overall price inflation.
Figure 3
Health State Budget: Pre–Recession Versus 2015–16 Proposal
(Dollars in Billions)
|
Fund Source
|
2007–08 Actual
|
2015–16 Proposed
|
Change From 2007–08 to 2015–16
|
|
Amount
|
Percent
|
|
General Fund
|
$17.4
|
$21.0
|
$3.6
|
21%
|
|
Federal fundsa
|
20.2
|
57.4
|
37.2
|
184
|
|
Realignment revenues
|
2.8
|
3.5
|
0.7
|
25
|
|
Other special funds
|
6.9
|
10.0
|
3.1
|
45
|
|
Totals (All Funds)
|
$47.3
|
$91.9
|
$44.6
|
94%
|
By far the largest factor accounting for the growth in total spending between 2007–08 and 2015–16 is the increase in federal funding of $37.2 billion, in large part reflecting the enhanced federal share of costs for the Medi–Cal expansion population under ACA. We note that embedded in the total spending increase over this period are some other changes in how health programs are funded. For example, in 2011–12 and 2013–14, costs for certain health programs were realigned to the counties resulting in lower General Fund costs for the state. The Legislature also implemented a tax on managed care organizations (MCOs) that: (1) increases Medi–Cal managed care rates by an amount that offsets the tax paid by MCOs and (2) funds state health programs.
The growth in total spending for health programs between 2007–08 and 2015–16 was largely driven by the implementation of ACA, which was enacted in 2010. However, prior to that time, the Legislature enacted a number of significant spending reductions in the health area in response to declining state revenues brought about by the recession. We briefly turn to a discussion of them now, before focusing our attention on how ACA has transformed the state’s health programs.
Here we provide a high–level overview of major reductions that have been the focus of recent legislative budget hearings. Most of these reductions were made in 2008–09 and 2009–10—in response to the recession and the state’s budget problem—and some remain in effect.
Reduced Some Payments to Medi–Cal Providers. The Legislature and Governor took some significant actions regarding provider rates during a February 2008 special legislative session held to address the state’s fiscal crisis. Legislation enacted at that time, Chapter 3, Statutes of 2008 (ABX3 5, Committee on Budget), reduced most Medi–Cal provider rates by 10 percent as of July 1, 2008, for an estimated savings of $291 million. Some Medi–Cal provider groups challenged the legality of these rate reductions in court, and on August 18, 2008, a federal judge issued an injunction blocking enforcement of these rate reductions for certain types of services provided on or after that date. The state later prevailed in court. While funding for some of the rate reductions was fully or partially restored for certain types of providers, most rate reductions remain in effect.
Eliminated Some Optional Medi–Cal Benefits. The February 2009 budget package eliminated certain optional benefits for adults effective July 2009 for savings of $122 million General Fund. The bulk of the savings came from the elimination of adult dental services, which were later partially restored at an estimated annual cost of $85 million General Fund. However, savings continue from the elimination of incontinence creams and washes, acupuncture, and other services.
Reduced Public Health Spending. In 2008–09, through a combination of legislative actions ($43 million General Fund) and Governor’s veto ($16 million General Fund) a total of $59 million General Fund was cut from various public health programs. In 2009–10, the budget further reduced General Fund spending on public health programs by a total of $154.2 million General Fund ($80.4 million General Fund from Governor’s veto). The major public health programs affected by this reduction were: (1) HIV/AIDS programs; (2) Maternal, Child and Adolescent Health program; (3) domestic violence shelters; and (4) immunization local assistance. Most of these reductions remain in effect although the 2014–15 budget restores $7 million General Fund for the Black Infant Health Program and HIV demonstration projects.
In 2010, the ACA became law. This is far–reaching legislation intended to provide increased access to health care. In part, the ACA is designed to create a health coverage purchasing continuum that makes it easier for persons to access, purchase, and maintain coverage. As individuals’ incomes rise and fall; as they become employed, change employers, or become unemployed; and as they age, they are to have access to different sources of coverage along the continuum. Since the passage of ACA, the Legislature has dedicated significant time and resources towards its implementation.
Establishment of a Health Benefit Exchange. Chapter 655, Statutes of 2010 (AB 1602, J. Perez), and Chapter 659, Statutes of 2010 (SB 900, Alquist and Steinberg), established the California Health Benefit Exchange, known as Covered California, along with a governing board. Through Covered California, individuals and employees of small businesses (50 employees or less) that choose to offer coverage through Covered California are able to enroll in subsidized and unsubsidized health coverage. Covered California provides federally funded tax subsidies to keep the cost of health coverage affordable for eligible individuals. Coverage offered through Covered California must include a minimum set of benefits, known as the “essential health benefits.”
The ACA implementation has had many different fiscal effects—some major and some minor—associated with implementing various provisions of state and federal law related to ACA. Here we describe the major effects.
Major Investments With Federal Support to Prepare for Implementation. In November 2010, the state secured a five–year agreement with the federal government to receive significant funding and support for the state’s preparations to implement the ACA. This agreement is known as the Bridge to Reform Section 1115 waiver. (In general, Section 1115 waivers allow states to operate demonstration projects that further the goals of the Medicaid program.) By demonstrating that changes under the waiver would be budget–neutral to the federal government, the state has drawn down over $10 billion in additional federal funding over the five–year span of the waiver. Among the major uses of these funds were (1) early initiatives—overseen by counties—to provide coverage to populations that would become newly eligible for Medi–Cal under the ACA, (2) incentive payments for public hospitals to improve and ready their health systems for these incoming enrollees, and (3) offsets to state spending for certain state–only health programs. The waiver was also the main vehicle for obtaining federal approval to shift various Medi–Cal populations into the managed care system, which we describe below. The Bridge to Reform waiver expires in November 2015, and the state is currently preparing to submit its proposal for a new waiver.
Expanded Eligibility and Enrollment. Under the ACA, beginning January 1, 2014, California expanded Medi–Cal eligibility to include over 1 million adults with incomes up to 138 percent of the federal poverty level (FPL). This is known as the optional expansion. For three years the federal government will pay 100 percent of the costs of health care services provided to the newly eligible population. Beginning January 1, 2017, the federal share of costs associated with the expansion will be decreased over a three–year period until the state pays for 10 percent of the expansion and the federal government pays the remaining 90 percent. The estimated cost in 2015–16 for providing Medi–Cal services to the roughly 2 million persons who will enroll in the program under the optional expansion is $14.3 billion (all federal funds except for $7.5 million General Fund).
Several factors—such as enrollment simplification, publicity, and outreach—will increase Medi–Cal enrollment among individuals who were previously eligible, but unenrolled—often referred to as the mandatory expansion. Generally, the state will continue to be responsible for 50 percent of the costs of providing services to mandatory expansion enrollees. The estimated cost in 2015–16 for providing Medi–Cal services to the roughly 1 million persons who will enroll in the program under the mandatory expansion are $2 billion total funds ($961 million General Fund). See the “Medi–Cal” section of this report for more information on this ACA–related caseload.
Made It Easier to Enroll and Remain Covered. The ACA and recent state legislation contain several provisions that are expected to simplify Medi–Cal eligibility and streamline the enrollment and redetermination processes, including:
- ACA Simplified Methodology Used to Determine Financial Eligibility. The ACA generally simplified the standards used to determine financial eligibility for most beneficiaries—excluding certain populations, such as SPDs. The two major changes to the methodology include requiring the use of Modified Adjusted Gross Income (MAGI) to calculate income and not requiring asset tests.
- Use of Electronic Data to Verify Eligibility. Pursuant to the ACA, many pieces of information needed to determine an applicant’s eligibility are required to be verified electronically by accessing existing state and federal databases. Consumers are only to be asked to provide physical verification of eligibility if reasonably compatible electronic verification is not available.
- “No Wrong Door” Approach for Applications. The state adopted a no wrong door approach for Medi–Cal applications. This allows applicants to apply: online through Covered California’s website, by calling either Covered California’s service center or county Medi–Cal eligibility offices, in person at county Medi–Cal eligibility offices, or through the mail.
- Other Streamlined Enrollment Processes. The state has also taken advantage of other options under the ACA to streamline the enrollment process, including hospital presumptive eligibility and express lane enrollment. Both are streamlined processes that allow certain individuals to enroll in Medi–Cal without completing a full application.
- Simplified Annual Redeterminations. The ACA and state legislation created a new annual redetermination process that reduces the amount of information that must be provided by beneficiaries and, instead, relies on available electronic data.
The combined effect of all of the changes described above to simplify Medi–Cal eligibility and streamline the enrollment and redetermination processes is to make it easier for Medi–Cal enrollees to obtain and maintain coverage. This has likely increased enrollment and associated spending in the program.
Since 2007–08, managed care has overtaken and surpassed fee–for–service (FFS) as the primary Medi–Cal service delivery system. While managed care has covered the majority of Medi–Cal enrollees for over a decade, until recently, the majority of General Fund spending was in FFS. This was because the most expensive populations and services—such as SPDs and long–term services and supports (LTSS)—remained in FFS.
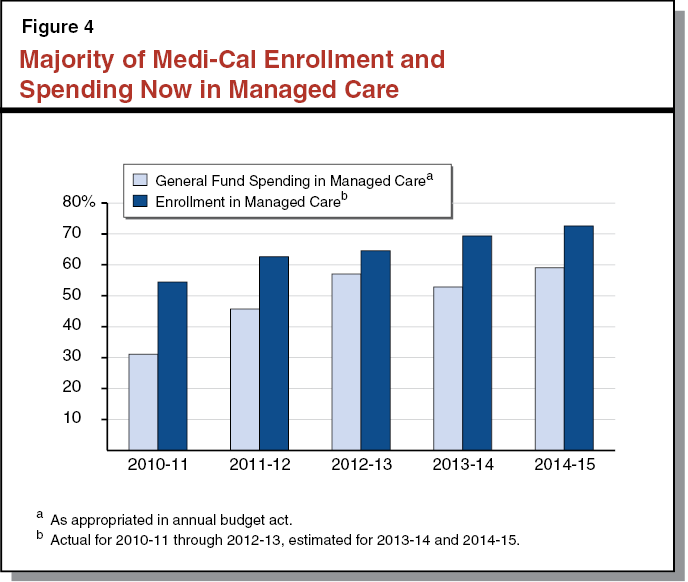
As Figure 4 shows, the bulk of both General Fund spending and enrollment has shifted from FFS to managed care. This is the result of a series of policies to move various groups of beneficiaries and services from FFS and managed care, often (but not always) via mandatory enrollment. From the state’s perspective, the major goals of these transitions have been to (1) improve care quality, efficiency, and access for the affected populations; and (2) provide budgetary predictability via capitated rate–setting. Below, we highlight the most significant Medi–Cal managed care transitions from the past five years.
Shift of Medi–Cal–Only SPDs to Managed Care. The first major transition occurred from June 1, 2011 through May 2012, when the state shifted 240,000 Medi–Cal–only SPDs (that is, SPDs who do not also receive coverage under Medicare) from FFS to Medi–Cal managed care in 16 counties.
Rural Expansion. From September to November 2013, the state expanded Medi–Cal managed care into 28 counties where managed care did not previously exist—generally rural counties. This first wave of the rural managed care expansion covered over 400,000 enrollees from the families and children population. In December 2014, the state began to shift 20,000 Medi–Cal–only SPDs in 19 of these rural counties into managed care.
Coordinated Care Initiative (CCI). The 2012–13 budget package authorized CCI as an eight–county demonstration project consisting of three main components: (1) integrating Medi–Cal and Medicare benefits for SPDs who are enrolled in both programs—known as “dual eligibles”—under the same managed care plans, (2) requiring mandatory enrollment of dual eligibles into managed care for their Medi–Cal benefits (dual eligibles are passively enrolled into these plans for Medicare benefits, meaning they will be enrolled unless they actively opt out), and (3) making LTSS available exclusively through managed care. Up to 426,000 dual eligibles are eligible for passive enrollment into the Medi–Cal–Medicare portion of the demonstration. Enrollment for CCI began in April 2014 and will continue through January 2016.
As described earlier, the Legislature eliminated certain Medi–Cal benefits during the economic downturn. However, the Legislature also has taken action since 2007–08 to add new benefits to the Medi–Cal program, particularly in the area of behavioral health. In many cases, the Legislature expanded these benefits as part of the state’s broader implementation of the ACA.
Alignment of Essential Health Benefits With Medi–Cal Benefits. Some non–specialty mental health and substance use disorder Medi–Cal benefits were enhanced to make them comparable to the essential health benefits provided by plans offered through Covered California. Aligning Medi–Cal benefits with the essential health benefits helps ensure that low–income persons moving back and forth between Medi–Cal and health coverage offered through Covered California will continue to receive comparable benefits as they move between sources of coverage. As of January 1, 2014, Medi–Cal managed care plans provide these non–specialty mental health and substance use disorder services to eligible Medi–Cal enrollees. (Specialty mental health services are provided through county mental health plans and other substance use disorder services are provided through Drug Medi–Cal [DMC]). The budget includes $276 million General Fund in 2015–16 to provide these services.
Behavioral Health Treatment (BHT). As of September 15, 2014, Medi–Cal managed care plans are required to provide medically necessary BHT services to eligible children and adolescents up to age 21 with Autism Spectrum Disorder (ASD). The budget includes $151 million General Fund in 2015–16 for the provision of BHT services. This benefit and its associated costs are discussed further in the “Medi–Cal” section of this report.
DMC Waiver Changes. The DHCS is currently seeking a DMC Organized Delivery System Waiver from the Centers for Medicare and Medicaid Services (CMS). This waiver seeks to demonstrate that organized substance use disorder care improves outcomes for DMC beneficiaries. Counties that opt–in to the waiver would provide a continuum of care to DMC beneficiaries and would provide additional benefits that are not available currently, such as residential treatment services. We note that the state is currently awaiting approval from CMS prior to implementing these changes. The budget includes $19.6 million General Fund to provide residential treatment services under this waiver in 2015–16. No other General Fund costs associated with the waiver are assumed in the budget.
Beginning mostly in 2012–13, the Legislature enacted legislation to eliminate three state departments and shift programmatic and administrative responsibility for several programs between departments. Generally, programs that provide health care services, such as treatment for illnesses, have been shifted from other departments to DHCS. The policy rationale for making some of these shifts is to allow DHCS to better integrate the physical health care provided by Medi–Cal with the care provided by other programs and identify administrative efficiencies by placing the state–level administration of programs that purchase health care services all within the same department. In addition, the policy rationale for shifting the DMC benefit and specialty mental health services (both Medi–Cal benefits formerly administered by other departments) to DHCS is to allow DCHS to better integrate substance use programs and specialty mental health care with the physical health care provided through Medi–Cal. Overall, the effect is to consolidate programs within fewer departments. The net overall fiscal effect of the department eliminations and program shifts is largely budget neutral. The major departmental eliminations and programmatic shifts were:
- Managed Risk Medical Insurance Board (MRMIB). The MRMIB was eliminated effective July 1, 2014. In 2012–13 and 2013–14, enrollees in California’s federal Children’s Health Insurance Program (CHIP), known as the Healthy Families Program (HFP), were shifted from HFP into Medi–Cal. Effective July 1, 2014, MRMIB was eliminated and programmatic and administrative responsibility for the remaining three programs administered by MRMIB (Major Risk Medical Insurance Program, Access for Infants and Mothers, and County Health Initiative Matching Fund Program) were shifted from MRMIB to DHCS.
- Department of Alcohol and Drug Programs (DADP). The DADP was eliminated effective July 1, 2013. State–level oversight of the DMC program was shifted from DADP to DHCS effective July 1, 2012. The DADP’s other programmatic and administrative responsibilities were transferred to other departments effective July 1, 2013.
- Department of Mental Health (DMH). The DMH was eliminated effective July 1, 2012. The DSH was created to administer the state hospitals, in–prison programs, and the conditional release program. State–level oversight for the bulk of community mental health programs, such as Medi–Cal specialty mental health services and Proposition 63 activities, was shifted from DMH to DHCS during 2011–12. Programmatic and administrative responsibility for the remaining DMH programs were transferred to various departments.
- Direct Health Care Service Programs Shifted From DPH to DHCS. Effective July 1, 2012, the budget plan transferred the following programs from DPH to DHCS: (1) Every Woman Counts, (2) Family Planning Access and Treatment, and (3) the Prostate Cancer Treatment Program. All of these programs provide direct health care services, similar to direct health care provided through other programs administered by DHCS.
The implementation of ACA has been the primary driver behind the expansion of health programs in California between 2007–08 and 2015–16. In particular, the Medi–Cal program, by far California’s largest health program in terms of enrollment and funding, has been subjected to a major programmatic transformation under ACA. Accordingly, our summary of the main takeaways from our analysis of programmatic and spending trends in the major health services programs since 2007–08 is focused on Medi–Cal as follows:
- Spending Up Significantly, Funding Mix Changed. While total spending has gone up by about 94 percent, there have been changes in how programs have been funded. Specifically, the amount of federal funds, as a percent of total health spending, has increased from 43 percent in 2007–08 to 62 percent in 2015–16. This is mainly due to increases in federal funding for Medi–Cal provided under ACA.
- Caseload Up. Caseload in the state’s Medi–Cal program has increased from 6.6 million in 2007–08 to 12.2 million in 2015–16. Major factors contributing to this increase in caseload include: (1) the shift of over 750,000 from the state’s CHIP, formerly known as HFP, to Medi–Cal; (2) the enrollment of an estimated 2 million newly eligible persons under the optional expansion; (3) the enrollment of an estimated 1 million previously eligible persons under the mandatory expansion, and; (4) the simplification of Medi–Cal eligibility determination criteria and the streamlining of enrollment and eligibility redetermination processes.
- Some Reductions Continue, but There Have Also Been Augmentations. There were a number of programmatic reductions made during the recessionary period. While funding for some of these reductions has been fully or partially restored, several of the reductions continue today. For example, certain optional benefits and provider rate reductions have not been restored. On the other hand, mainly as part of ACA implementation, there have been a number of program augmentations since 2007–08. Generally, these augmentations, such as adding new Medi–Cal managed care benefits, have been intended to align state program benefits, enrollment systems, and eligibility requirements in order to create a continuum of health care services for persons obtaining health insurance through public health care services programs such as Medi–Cal and Covered California.
In California, the federal–state Medicaid program is administered by DHCS as the California Medical Assistance Program (Medi–Cal). Medi–Cal is by far the largest state–administered health services program in terms of annual caseload and expenditures. As a joint federal–state program, federal funds are available to the state for the provision of health care services for most low–income persons. Until recently, Medi–Cal eligibility was mainly restricted to low–income families with children, SPDs, and pregnant women. As part of the ACA, beginning January 1, 2014, the state expanded Medi–Cal eligibility to include additional low–income populations—primarily childless adults who did not previously qualify for the program.
Financing. The costs of the Medicaid program are generally shared between states and the federal government based on a set formula. The federal government’s contribution toward reimbursement for Medicaid expenditures is known as federal financial participation (FFP). The percentage of Medicaid costs paid by the federal government is known as the federal medical assistance percentage (FMAP).
For most families and children, SPDs, and pregnant women, California generally receives a 50 percent FMAP—meaning the federal government pays one–half of Medi–Cal costs for these populations. However, a subset of children with higher incomes qualify for Medi–Cal as part of the state’s CHIP. Currently, the federal government pays 65 percent of the costs for children enrolled in CHIP and the state pays 35 percent. Finally, under the ACA, the federal government will pay 100 percent of the costs of providing health care services to the newly eligible Medi–Cal population from 2014 through 2016; the federal matching rate will phase down to 90 percent by 2020 and thereafter.
Delivery Systems. There are two main Medi–Cal systems for the delivery of medical services: FFS and managed care. In a FFS system, a health care provider receives an individual payment from DHCS for each medical service delivered to a beneficiary. Beneficiaries in Medi–Cal FFS generally may obtain services from any provider who has agreed to accept Medi–Cal FFS payments. In managed care, DHCS contracts with managed care plans, also known as health maintenance organizations, to provide health care coverage for Medi–Cal beneficiaries. Managed care enrollees may obtain services from providers who accept payments from the managed care plan, also known as a plan’s “provider network.” The plans are reimbursed on a “capitated” basis with a predetermined amount per person, per month regardless of the number of services an individual receives. Medi–Cal managed care plans provide enrollees with most Medi–Cal covered health care services—including hospital, physician, and pharmacy services—and are responsible for ensuring enrollees are able to access covered health services in a timely manner. (In some counties, Medi–Cal managed care plans also provide LTSS, including institutional care in skilled nursing facilities [SNFs], and home– and community–based services.) The number and type of managed care plans available vary by county, depending on the model of managed care implemented in each county. Counties can generally be grouped into four main models of managed care:
- County Organized Health System (COHS). In the 22 COHS counties, there is one managed care plan available to beneficiaries that is run by the county.
- Two–Plan. In the 14 Two–Plan counties, there are two managed care plans available to beneficiaries. One plan is run by the county and the second plan is run by a commercial health plan.
- Geographic Managed Care (GMC). In GMC counties, there are several commercial health plans available to beneficiaries. There are two GMC counties—San Diego and Sacramento.
- Regional. Finally, in the Regional model, there are two commercial health plans available to beneficiaries across 18 counties.
Imperial and San Benito Counties have managed care plans that do not fit into one of these four models. In Imperial County, there are two commercial health plans available to beneficiaries and in San Benito, there is one commercial health plan available to beneficiaries.
According to the Medi–Cal Eligibility Data System (MEDS), there were over 11 million people enrolled in Medi–Cal as of September 2014. This count includes 2 million enrollees—mostly childless adults—who became newly eligible for Medi–Cal under the optional expansion. A substantial number of families and children who were previously eligible—known as the mandatory expansion—are also assumed to have enrolled as a result of eligibility simplification, enhanced outreach, and other provisions and effects of the ACA. The Governor’s budget assumes that following the large influx of enrollees in 2014–15, ACA–related caseload levels will stabilize during 2015–16. The budget also assumes modest underlying growth for baseline enrollment within the families and children and SPD populations. Below, we briefly review the administration’s methodology for forecasting Medi–Cal caseload to provide background and context for our assessment of these projections.
Base Forecast. The DHCS builds its total caseload estimate for Medi–Cal by separately estimating, then combining, two distinct forecasts. The first forecast is known as the base. The base relies on historical trends from actual enrollment data in MEDS. (For the Governor’s January budget proposal, the base reflects MEDS data that is current through August 2014.) The department studies movements in caseload from past periods, then applies statistical techniques to extrapolate future trends from these patterns. The base represents DHCS’ view of the underlying trend—that is, how caseload would evolve absent major shifts (such as the HFP transition) and policy changes in the program.
Policy Change Forecast. The second type of forecast estimates the effect of the aforementioned shifts and policy changes. These policy changes generally consist of new proposals in the Governor’s budget, or enacted policies that DHCS determines are too new or complex to be reliably reflected in the base, mainly due to insufficient historical enrollment data. In particular, policies with long and complicated implementation schedules—or wide–ranging effects that may take years to stabilize—are likely to be estimated through DHCS’s policy change forecast, at least over several budget cycles. When DHCS analysts forecast policy changes, they typically do not use the formal statistical techniques that characterize the base. Instead, each policy change estimate relies on the analyst’s assumptions, judgment, and information obtained outside of formal statistical modeling.
Administration Continues to Project ACA Caseload Mainly Through Policy Change Forecast. The Governor’s budget contains no new policy proposals that are assumed to affect Medi–Cal caseload. Instead, all major policy changes that impact the caseload estimate outside of the base are associated with ongoing provisions and effects of the ACA. There were eight months of post–ACA enrollment data (January through August 2014) available to DHCS at the time of the budget’s preparation. The DHCS indicated that despite additional data, ACA–related enrollment trends have not stabilized enough to be fully incorporated into statistical modeling for the base.
Figure 5 displays a decade of observed and estimated caseload for each major category of enrollment in Medi–Cal, beginning with (1) historical caseload through 2012–13, followed by (2) the administration’s revised estimate for caseload in 2013–14, and (3) the budget’s projections for 2014–15 and 2015–16. The families and children caseload grew at 4 percent annually between 2006–07 and 2010–11 (the onset of the Great Recession through the sluggish phase of the recovery), while SPD enrollment grew at about 2 percent annually over the same period. The further uptick in families and children through 2013–14 reflects the shift of HFP to Medi–Cal. Between January and November 2013, this transition added over 750,000 children to Medi–Cal’s caseload. (Later, we show that absent the HFP transition, the underlying trend for families and children caseload actually flattened in 2012–13.) Later, we take a closer look at these underlying trends prior to ACA implementation, and how they compare to the administration’s outlook for 2014–15 and 2015–16.
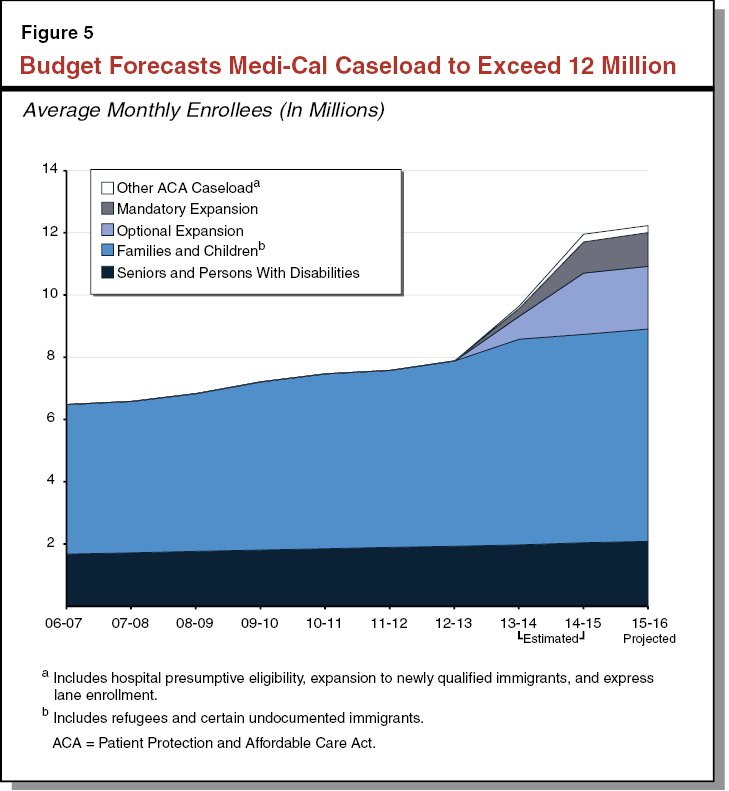
The Governor’s budget assumes total annual Medi–Cal caseload of 12.2 million for 2015–16. This is a 2 percent increase over the revised caseload estimate of 12 million for 2014–15. As noted earlier, the administration continues to isolate the ACA’s effect through its policy change forecast. Below, we break out the Governor’s caseload projections by the portion associated with ACA–related policies, and the remaining portion that is mainly captured in DHCS’s base forecast.
ACA Caseload. The budget assumes that compared to 2013–14—which reflected the first six months of implementation for ACA–related expansions—the combined annual caseload from the optional and mandatory expansions will have tripled in 2014–15. Following this steep climb, the budget assumes that in 2015–16, the optional and mandatory expansions will remain flat at 2 million and 1 million enrollees, respectively. The budget estimates that combined caseload from other ACA–related policies, such as express lane enrollment and hospital presumptive eligibility, will be 250,000 in 2014–15 and 220,000 in 2015–16.
Non–ACA Caseload. The administration projects that annual Medi–Cal caseload in the base forecast—absent the effects of the ACA—will be 8.8 million in 2014–15 and 8.9 million in 2015–16—a 2 percent year–over–year increase. Between the two years, the budget also implies that the underlying trend for both SPDs and families and children is 2 percent growth.
Senior Trend Raises Questions. Figure 6 displays historical annual growth rates for Medi–Cal’s senior caseload (enrollees aged 65 and older), followed by the administration’s estimated growth trend from 2013–14 onward. The DHCS projects the senior caseload to increase 5.7 percent in 2014–15, yet only 2.3 percent in 2015–16. According to the department, MEDS data through August shows senior enrollment being considerably higher than was assumed under the 2014–15 Budget Act. The department also indicated that the estimated spike in 2014–15 may reflect the delay in Medi–Cal redeterminations that occurred from January through June 2014 and the modified renewal process that occurred from July through December 2014. (Under the modified process, counties maintained eligibility for all enrollees who submitted a completed renewal form, regardless of whether these enrollees actually continued to meet eligibility criteria.) These policies may have led to more seniors staying enrolled in Medi–Cal than would have otherwise been the case.
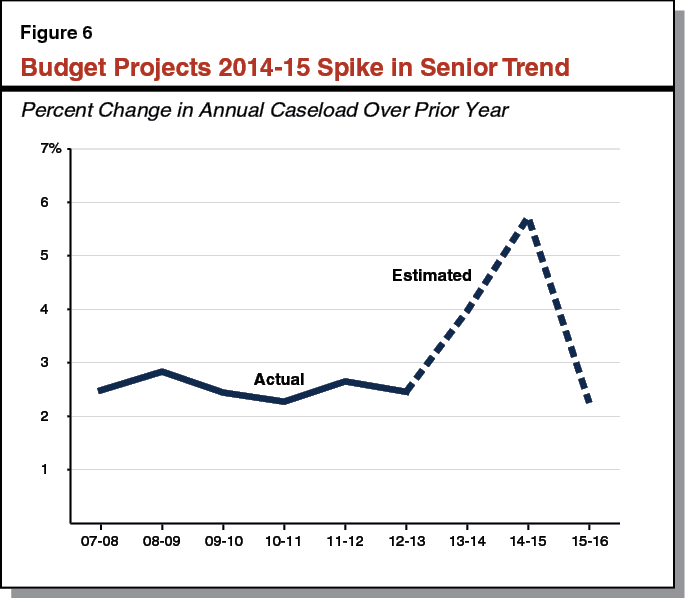
The spike has a material impact on spending in 2014–15. Most seniors enrolled in Medi–Cal are dually eligible for Medi–Cal and Medicare. For 2014–15, the budget’s updated estimate of the number of dual eligibles enrolled in the Medicare prescription drug benefit is higher by 5 percent, leading to a $95 million increase in General Fund spending compared to the 2014–15 Budget Act. (The state makes monthly payments to the federal government for providing Medicare prescription drug coverage to dual eligibles.)
In terms of underlying trends, seniors represent the fastest–growing segment of Medi–Cal caseload, due to the state’s large cohort of baby boomers passing age 65. Over the two–year period, DHCS’s implied annual growth rate for seniors is 4 percent, which is more in line with our expectations. As suggested by the department, the delay in redeterminations, modified renewal process, or other temporary factors could explain the 2014–15 spike as a one–time anomaly. However, without more current data on enrollment, we cannot rule out the other possibility that the spike could signal an upward shift in the underlying trend for seniors, due to demographic changes or other fundamental factors.
Assumes Underlying Growth for Families and Children, Despite Improving Economy. Excluding the caseload associated with the ACA, the budget implies 1 percent growth in base caseload for families and children in 2014–15, rising to 2 percent growth in 2015–16. However, Figure 7 shows that prior to the ACA, Medi–Cal enrollment among families and children moved countercyclical to the economy. (This means that families enrollment tends to go up during an economic downturn and go down during an economic expansion.) We note that caseload for California Work Opportunity and Responsibility to Kids (CalWORKS)—a means–tested program that overlaps with Medi–Cal in terms of the families enrolled—has declined steadily since 2011–12. (For more information on the CalWORKS budget, see our report The 2015–16 Budget: Analysis of the Human Services Budget.)
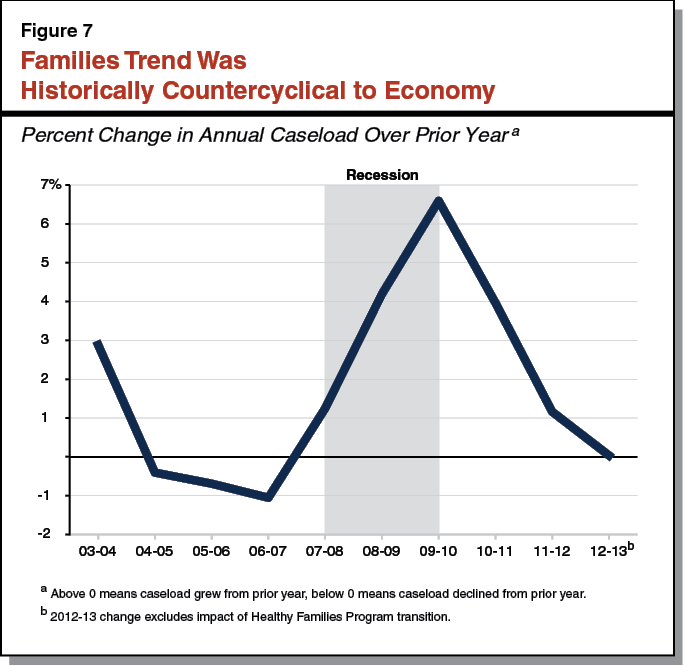
As stated in our November report The 2015–16 Budget: California’s Fiscal Outlook, we expect the underlying trend for Medi–Cal’s families caseload (absent ACA impacts) to transition to a slight decline as the economy expands. Historically, there has usually been some lag between the onset of an economic recovery and a turning point in the families caseload for Medi–Cal. However, the economy is well into the sixth year of the current expansion. All else equal, we would have expected the underlying trend for families to be declining—particularly since the trend showed signs of leveling off just prior to the beginning of ACA–related enrollment.
Budget staff at DHCS indicated that they, too, expect the families trend to slow and reverse if the economy continues to strengthen. Nonetheless, their approach is to maintain a modest growth rate in the base model for the families caseload until the MEDS data shows clear signs of a downward trend. If an obvious turning point occurs, they will adjust their base model. This “wait–and–see” approach is a conservative approach driven in part by the administration’s desire to avoid a deficiency in the program. For example, projecting a 1 percent decline rather than a 2 percent increase for the underlying trend would translate into 200,000 fewer enrollees in the families category, or about $240 million less in General Fund appropriations for 2015–16 (assuming a 50 percent federal matching rate). However, as described later, interpreting the underlying trend in the current data is very difficult given the ACA–related mandatory expansion.
ACA Caseload Estimates Subject to Uncertainty. The ACA–related caseload increase that occurred in 2014–15 was much larger than expected. While some data are available regarding ACA–related caseload, the ACA is a major policy change, and additional months of data are necessary to further clarify these enrollment trends. As noted earlier, according to MEDS data, there were over 2 million people enrolled through the optional expansion as of September 2014. This is higher than initial estimates of the total population eligible for the optional expansion. Therefore, we find the administration’s assumption that the optional expansion population will remain relatively flat at just over 2 million in 2015–16 to be reasonable. However, we find the mandatory expansion estimates to be more uncertain, as it is no longer possible to parse out this population in MEDS data. We discuss this in more detail immediately below.
Unpacking the Mandatory Expansion Estimate. Families and children newly enrolled in Medi–Cal as of January 1, 2014 were enrolled through the simplified eligibility criteria required by ACA (referred to as “MAGI standards”). In developing the caseload estimate that was adopted in the June 2014 budget, DHCS identified previously eligible families and children in the MEDS data as being part of the mandatory expansion population on the basis of being enrolled in Medi–Cal through MAGI standards. The department used its policy change forecast to project enrollment growth for these mandatory expansion families and children. Families and children who were enrolled prior to 2014 and had not yet gone through a redetermination, could be identified in the MEDS data as having been enrolled through pre–ACA eligibility criteria. These pre–ACA families and children remained in the base forecast, where DHCS applied its modest growth trend. However, as of January 1, 2014, most families and children who undergo a Medi–Cal eligibility renewal will be eligible under the post–ACA MAGI standards. This means it is no longer possible to distinguish families and children who enrolled post–ACA with those who were enrolled before the ACA. Thus, in the 2015–16 budget, DHCS was forced to incorporate all families and children, including those enrolled under MAGI standards, into the base data.
To account for this change, the DHCS states that for the 2015–16 budget proposal, 65 percent of the caseload estimate for the mandatory expansion is now reflected in the base. However, the budget still forecasts the total caseload estimate for the mandatory expansion using its policy change forecast. This has key implications.
- Underlying Trend for Families and Children May Be Decreasing. The underlying trend for families and children caseload could well be decreasing as the economy gains traction. Even if so, it may be impossible to tell as Medi–Cal coverage for more individuals is renewed through MAGI standards, blurring the distinction between first–time and renewing applicants. The DHCS’s default assumption for base families caseload is modest growth, and it appears that the department will maintain this trend as long as the ACA continues to add more enrollees to the base and obscures any signs of an underlying turning point.
- Mandatory Expansion Designation May No Longer Be Appropriate. The “mandatory” designation may have made sense at the early stages of ACA–driven enrollment. However, the label now seems arbitrary, as both pre–ACA and post–ACA families and children are enrolled through MAGI standards. The logic behind independently projecting the mandatory expansion in the policy change forecast is hard to follow and may be increasingly removed from reality.
We withhold recommendation on the administration’s caseload estimates at this time. We have outlined a number of issues that prevent us from getting a clear reading of the underlying trend for major categories of enrollment. While uncertainty is inherent in all caseload estimates—and not by itself a reason to withhold recommendation—normally we would have had a sense of the trend’s overall direction to comment on whether the administration’s assumptions seemed reasonable. Part of this was due to our ability to draw from sources of enrollment data outside the budget estimate. As described below, this supplementary information is no longer available to us.
Our overall advice for the Legislature is to wait for the May Revision, which will incorporate MEDS data through February 2015. By then, a number of issues complicating the 2014 data—such as the effect of the redetermination delay and modified renewal process—should be significantly (though not entirely) mitigated. Meanwhile, we have recommendations on how the Legislature can improve the state of available caseload information leading up to the May Revision.
Require Administration to Resume Monthly Caseload Reports. Prior to 2014, DHCS released monthly reports on Medi–Cal caseload levels and trends. Although these reports came with certain caveats, they were useful for keeping abreast of the overall direction of statewide Medi–Cal enrollment. In March 2014, DHCS stated that “[a]mid the initial stages of implementing the [ACA], current Medi–Cal enrollment information is volatile and initial datasets may provide misleading information.” The department went on to announce the temporary suspension of its monthly caseload reports. Since that time, the department has also indicated that it is working through its internal procedures to comply with federal health data privacy rules and ensure that any data released is sufficiently aggregated.
Nearly a year later, DHCS has not resumed any regular reporting on actual caseload. In lieu of these updates, the only publicly available documents on total and categorized Medi–Cal enrollment are the Governor’s biannual budget estimates. In this analysis, we are limited to citing preliminary MEDS data from September 2014. We obtained this data near the end of October by submitting a special request to DHCS.
Caseload data is fundamental to estimating the financing and delivery costs of health and human service programs. (We note that the Department of Social Services posts monthly caseload updates for CalWORKS on its website.) We recognize there was indeed ACA–related volatility when DHCS made its initial decision to halt monthly reporting, due to the first open enrollment and the ensuing backlog of Medi–Cal applications. However, with much of the backlog now resolved, the Legislature continues to operate in a five–month information vacuum with respect to caseload. We recommend the Legislature require DHCS to report at budget hearings on options for releasing statewide monthly enrollment data, aggregated at the level of families and children, SPDs, and childless adults.
Ask Administration About Future Treatment of Mandatory Expansion. It is clear that the ACA, through enrollment simplification and outreach, has led to greater Medi–Cal uptake among those previously eligible. However, continuing attempts to parse out this segment from the overall caseload estimate seem abstract and potentially misleading, as more data accumulate and any definable distinction between mandatory and nonmandatory caseload fades. The DHCS indicated that the May Revision will likely continue to project the mandatory expansion as part of its policy change forecast. We recommend that the department report at budget hearings about this forecasting decision and how it interacts with the projection for the underlying trend in families and children caseload.
In Addition to ACA, Begin Refocusing on Underlying Trends. While the ACA has had an important and sudden impact on total Medi–Cal enrollment, in this analysis we have also raised the issue of underlying enrollment trends for the Legislature’s consideration. We recommend the Legislature explore this issue during budget hearings. For example, we suggest the Legislature ask the administration to describe its outlook for the economy’s effect on the families caseload. We agree that budgeting for some downside risk is prudent. Outside of budgeting, however, there are policy reasons to be interested in caseload’s future trajectory, such as access and capacity within the program. Finally, we recommend the Legislature require the department to report on sustained increases in costlier Medi–Cal populations that are not driven by the ACA, such as the underlying trend for seniors.
BHT Services Added as a Medi–Cal Benefit After 2014–15 Budget Act Enacted. Chapter 40, Statutes of 2014 (SB 870, Committee on Budget and Fiscal Review), the health trailer legislation for the 2014–15 Budget Act, requires DHCS to add BHT services, such as Applied Behavioral Analysis (ABA), as a covered Medi–Cal benefit to the extent required by federal law. Subsequent to the enactment of the 2014–15 Budget Act, the federal government issued guidance indicating that BHT should be a covered Medicaid benefit for eligible children and adolescents with ASD. In response to the guidance, DHCS is in the process of obtaining federal approval for the provision of BHT services to Medi–Cal beneficiaries under age 21 with ASD. In the interim, as of September 15, 2014, Medi–Cal managed care plans are required to provide medically necessary ABA services for eligible children and adolescents with ASD.
Budget Includes Preliminary Cost Estimates for BHT. The Governor’s budget includes $89 million General Fund in 2014–15 that was not included in the 2014–15 Budget Act and $151 million General Fund in 2015–16 for the provision of BHT services to eligible children with ASD. The DHCS is still in the process of reviewing data on cost and utilization of BHT services; therefore, the estimated costs of BHT services included in the Governor’s budget are preliminary. The DHCS expects to provide updated estimates for the cost of BHT services at the time of the May Revision.
Some Medi–Cal Enrollees Currently Receive BHT Services Through Department of Developmental Services (DDS). There are about 7,500 children and adolescents enrolled in Medi–Cal who receive BHT services through DDS. With the addition of BHT services as a Medi–Cal benefit, as new children enroll in Medi–Cal and existing enrollees are provided BHT services, they will receive them through Medi–Cal and not through DDS. This is consistent with the policy that DDS is the payer of last resort for services it provides to developmentally disabled individuals. Additionally, DHCS expects those children and adolescents currently receiving BHT services through DDS to transition to receiving BHT services through Medi–Cal managed care during 2015–16. The current cost associated with providing BHT services through DDS is roughly $70 million General Fund annually and is included in the Governor’s budget for DDS. There is no funding in the Medi–Cal budget to reflect the anticipated transition of costs from DDS to Medi–Cal for BHT as children and adolescents transition to receiving BHT services through Medi–Cal.
Implementation of BHT Benefit in Early Stages. While Medi–Cal–enrolled children and adolescents with ASD have been able to access BHT services since September, DHCS is in the early stages of implementing the BHT benefit. The number of children and adolescents receiving services is slowly ramping up. At the time of this analysis, 420 children and adolescents are receiving BHT services through Medi–Cal managed care plans and an additional 1,200 are in the process of being screened and evaluated for eligibility for BHT services. There are likely several thousand additional children and adolescents who will access BHT services through Medi–Cal. This is in addition to the 7,500 Medi–Cal enrolled children and adolescents receiving BHT services through DDS.
LAO Assessment. Based on the rate of the ongoing phase–in of BHT services and our review of the preliminary data used to estimate the cost of BHT services in the Governor’s budget, we expect that the estimated costs to provide BHT services (excluding costs in the DDS budget) in 2014–15 and 2015–16 are likely to be lower at the time of the May Revision than the current estimate of $89 million General Fund in 2014–15 and $151 million General Fund in 2015–16. We will review the administration’s updated estimates in May and provide the Legislature with our recommendations if we find adjustments to the Governor’s estimates are warranted.
The MCO tax is an important source of funding for the state’s Medi–Cal costs. The administration estimates that revenues from this tax will offset General Fund spending for Medi–Cal local assistance by $800 million in 2014–15 and $1.1 billion in 2015–16. Under existing law, the tax expires on July 1, 2016. In July 2014, CMS issued a letter to states indicating that taxes structured like California’s MCO tax are inconsistent with federal Medicaid law and regulations. The CMS’s letter advises California to bring its MCO tax structure into compliance by no later than August 30, 2016. If the state were to extend the tax beyond this deadline without addressing CMS’s concerns, it could risk losing over $1 billion in federal Medicaid funds annually.
The MCO tax is an important part of the Governor’s budget plan because (1) it provides significant General Fund relief for the Medi–Cal budget and (2) the Governor proposes to use some of the funding for additional purposes in the In–Home Supportive Services (IHSS) Program. In this analysis, we provide a framework for the Legislature to understand the potential effects of the Governor’s proposal and recommend how the Legislature should respond to it.
Health Care–Related Taxes Are Defined in Federal Law. Federal Medicaid law defines a health care–related tax as a licensing fee, assessment, or other mandatory payment that is related to the provision of or payment for health care services or items. In many cases, states collect these payments from health care providers to help finance the nonfederal share of their Medicaid expenditures.
Federal Requirements for Health–Care Related Taxes. Health care–related taxes must meet three major requirements to be deemed permissible under federal Medicaid law. Figure 8 outlines these requirements. Federal law also defines 19 classes of health care providers for the purposes of applying the broad–based requirement. These classes include hospitals, SNFs, and MCOs. Therefore, to satisfy the broad–based requirement, a state that levies a health care–related tax on some MCOs must levy the same tax on all MCOs under its jurisdiction—unless the state obtains a federal waiver, which we describe shortly.
Figure 8
Three Requirements for Health Care–Related Taxes
|
Broad–Based. The tax is broad–based if it is imposed on all providers within a specified class of providers.
|
|
Uniform. The tax is uniform if it is applied at the same rate for all payers of the tax.
|
|
No Hold Harmless. The state may not provide a direct or indirect guarantee that providers receive their tax payment back (or be “held harmless” from the tax).
|
States Can Receive Waivers of Broad–Based and Uniform Requirements. Federal Medicaid rules permit some health care–related taxes that do not meet the strict definitions of “broad–based” and “uniform.” (Federal law does not allow for any waivers of the no–hold–harmless requirement.) Thus, some permissible taxes may exempt certain providers and/or vary the tax rate across providers. To ensure such a tax is treated as permissible, a state must formally request CMS to waive the broad–based and uniform requirements. Within this waiver request, the state must demonstrate that its tax structure is generally redistributive. In practice, this means the state has to provide certain calculations to show that the tax—like a strictly broad–based and uniform tax—would tend to transfer revenue from non–Medicaid to Medicaid providers. Therefore, if the state attempted to exempt all non–Medicaid providers from the tax, the tax would likely fail to be generally redistributive and be denied a waiver from CMS.
A waiver of broad–based and uniform requirements for health care–related taxes—if approved—is effective the first day of the quarter the waiver is received from CMS. (For example, a waiver received at the end of September would be retroactively effective to the beginning of July.) California has secured waivers for two of its largest permissible health–care related taxes: the hospital quality assurance fee and the SNF quality assurance fee. Both fees exempt certain facilities and vary their rates based on the size or type of facilities.
Requirements Can Create “Losers” Among Taxed Providers. Because health care–related taxes must be broad–based or generally redistributive, they must include providers that do not participate much (or at all) in Medicaid. These providers are unlikely to receive sufficient Medicaid payments to fully offset the amount of tax they owe.
Impermissible Taxes Result in Loss of Federal Medicaid Reimbursement. States must report their quarterly Medicaid expenditures to CMS to document the amounts that qualify for federal reimbursement. If CMS finds that a state has received revenues from impermissible health care–related taxes, then CMS will deduct these revenues from the state’s allowable Medicaid expenditures. In effect, this reduces the amount of FFP that the state would otherwise be entitled to receive.
California’s Current MCO Tax. Chapter 33, Statutes of 2013 (SB 78, Committee on Budget and Fiscal Review), imposes a sales tax on the “sellers” of Medi–Cal managed care plans—for the privilege of selling Medi–Cal health care services at retail—until July 1, 2016. (The terms “managed care plan” and “MCO” are often used interchangeably. In our view, this usage conflates the basis for the tax with the actual entity that pays the tax. For purposes of this analysis, we define managed care plan as a particular health coverage product, and MCO as the licensed carrier offering this product. For more information on how we classify MCOs and managed care plans throughout this analysis, see the nearby box.)
Chapter 33 establishes the MCO tax as 3.9 percent—equal to the sales and use tax rate—of the total operating revenue an MCO receives through its Medi–Cal managed care plan. The state Board of Equalization (BOE) collects the tax from MCOs in quarterly installments and deposits the proceeds into a special fund. At a high level, the tax can be thought of as drawing down enough FFP to hold MCOs harmless and offset other General Fund costs. The actual process, however, works somewhat in the opposite direction. Below, we provide more information about the process.
Throughout this analysis, we use the term “MCO” to refer to a health coverage carrier whose licensure and activities are governed under the Knox–Keene Health Care Service Plan Act of 1975. These carriers contract to provide or arrange for all medically necessary covered services for their enrollees, in return for fixed monthly prepayments. (This approach is sometimes referred to as the “promise to provide care.”) With the exception of Gold Coast Health Plan in Ventura County, all MCOs are licensed and regulated by the Department of Managed Health Care (DMHC) for at least some of their products. The MCOs are commonly known for operating health maintenance organizations (HMOs), although some also operate preferred provider organizations (PPOs) that are regulated by DMHC. In contrast, other PPOs and indemnity health insurance companies contract to cover a specific dollar loss or percentage of loss related to their policyholders’ medical expenditures. (This approach is sometimes referred to the “promise to pay.”) This type of health insurance is regulated by the California Department of Insurance (CDI). Over 21 million Californians, or more than half of the state’s population, are enrolled in DMHC–regulated MCO products. By comparison, around 2 million Californians have health insurance regulated by CDI.
A single MCO may contract with a variety of payers to provide health coverage. These may include (1) individuals who purchase coverage for themselves or their families, (2) businesses and public agencies that purchase coverage for their employees, and (3) government programs like Medi–Cal and Medicare that outsource care delivery for their beneficiaries. By “managed care plan,” we mean an MCO’s contract to provide services to a particular payer within a particular health coverage product. For example, in our nomenclature, Anthem Blue Cross is an MCO, while Anthem’s HMO contract with the Department of Health Care Services to enroll and provide care for Medi–Cal beneficiaries is the MCO’s “Medi–Cal managed care plan.”
As shown in Figure 9, the state initially pays its share of Medi–Cal capitation rates—which include the built–in cost of the MCO tax—from the General Fund. These payments draw down federal funds at the relevant matching rate. Meanwhile, BOE collects the tax based on MCOs’ projected Medi–Cal revenues, which include the federal and state shares. (The BOE reconciles these collections with MCOs’ actual Medi–Cal revenues in the following tax year.) Thus, as MCOs make tax payments to BOE, they are simultaneously made whole through higher Medi–Cal payments that incorporate the cost of the tax. Finally, DHCS withdraws most of the tax proceeds from the special fund as quarterly reimbursement for (1) the state’s share of capitation increases for the cost of the tax, and (2) other General Fund costs in the Medi–Cal program.
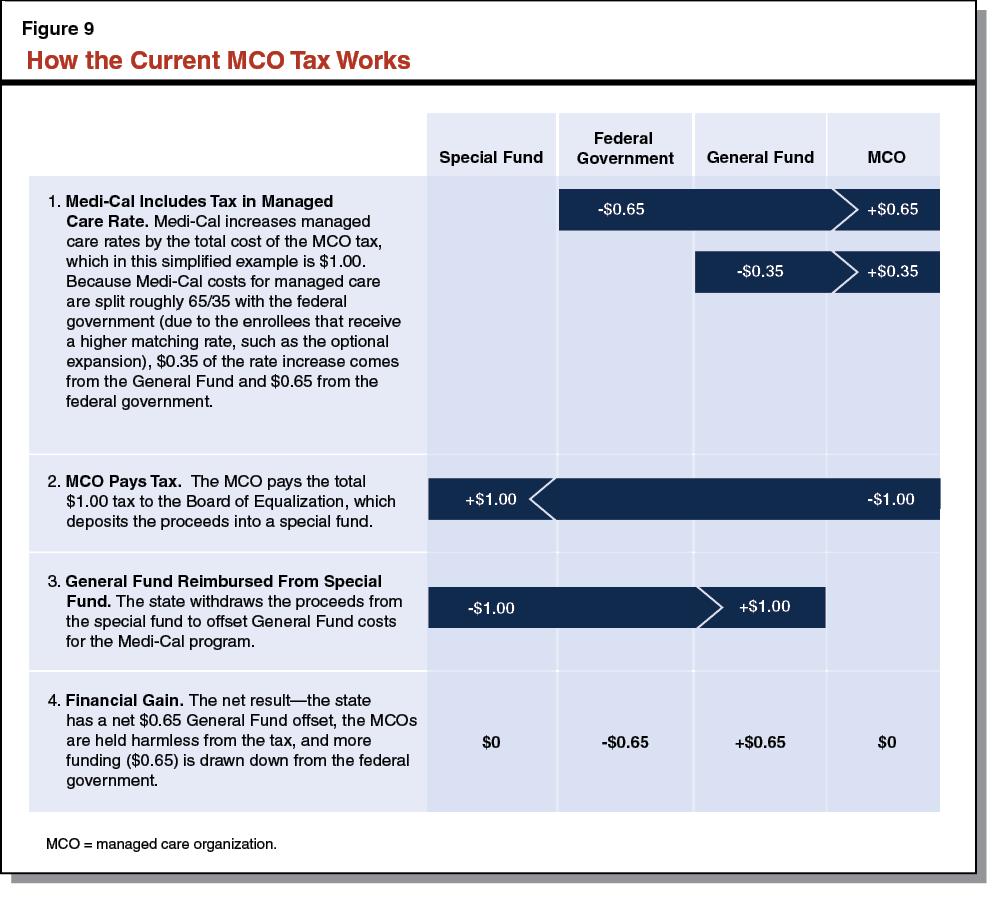
Figure 10 shows the administration’s revised estimates for the flow of funds in 2014–15. The combined amount of General Fund and federal funds for capitation increases—$1.4 billion—is equal to the amount of MCO tax revenue collected. (The federal funds amount is higher than the General Fund amount due to the enhanced matching rate for certain populations and services, such as the optional expansion.) The difference between the General Fund’s contribution to and reimbursement for capitation increases is due to the timing lag between BOE’s collection of the tax and DHCS’s request for funding adjustments.
Figure 10
Funding Flow of Current MCO Tax in 2014–15
|
Inflows/(Outflows), (In Millions)
|
Special Fund
|
General Fund
|
Federal Funds
|
|
Capitation increases for Medi–Cal managed care
|
—
|
($510.8)
|
($922.0)
|
|
MCO tax revenue collection
|
$1,433.3
|
—
|
—
|
|
Reimbursement of General Fund for capitation increasesa
|
(466.0)
|
466.0
|
—
|
|
Reimbursement of General Fund for other Medi–Cal costsa
|
(802.8)
|
802.8
|
—
|
Current MCO Tax Likely Impermissible. In its July 2014 letter, CMS clarified its interpretation of federal requirements governing health care–related taxes. Specifically, CMS indicated that taxes structured like California’s current MCO tax will likely be considered health care–related taxes from the federal perspective, meaning that California’s tax would need to meet the various Medicaid requirements for health care–related taxes (unless an available waiver is obtained). Of the state’s nearly 70 full–service MCOs, over half do not contract with DHCS to provide Medi–Cal managed care plans and therefore do not pay any MCO tax. Clearly, within the provider class of MCOs, the tax is neither broad–based (a fundamental requirement for health care–related taxes) nor generally redistributive (a condition to obtain a waiver from this requirement). Therefore, it is likely impermissible under federal Medicaid rules.
If the tax is extended in its current form past CMS’s deadline for states to reform their tax structures, California would risk the entire amount of FFP attached to the tax. However, because (1) CMS’s deadline is the end of states’ legislative sessions—August 31, 2016 for California—and (2) the current MCO tax sunsets on July 1, 2016, we believe the FFP amounts generated by the tax in 2014–15 and 2015–16 are not at risk, even if the state took no further action to extend or modify the tax. The administration estimates this FFP to be $922 million in 2014–15 and $1.2 billion in 2015–16.
IHSS Legal Settlement Agreement. In 2013, the administration agreed to a settlement with plaintiffs who had brought two class–action lawsuits against the state related to previously enacted IHSS budget reductions. The terms of the IHSS settlement agreement led to the implementation of the 7 percent reduction in IHSS hours in 2014–15. The settlement agreement’s terms also require the administration to pursue CMS approval for an “assessment”—with the resulting revenue used to provide the nonfederal share of funding needed to restore service hours from the current 7 percent reduction. The terms of the IHSS settlement agreement—recently amended by both parties—further specify that the administration must submit the assessment (if approved by the Legislature) for CMS approval no later than April 1, 2015. If this deadline is missed, the parties to the settlement agreement will discuss next steps, which ultimately could result in going back to the court for a resolution and court–ordered remedies.
The Governor proposes to restructure the MCO tax to conform to federal Medicaid requirements as clarified by the recent CMS guidance. The administration will pursue a tax structure that meets the criteria for a broad–based and uniform waiver—including a generally redistributive structure—as well as the no–hold–harmless requirement. The Governor proposes that the new structure, in addition to being federally permissible, be designed to raise enough revenue to fund two objectives. Below, we list these objectives in descending order of funding priority, as specified in the administration’s draft language.
- Fund 7 Percent Restoration in IHSS. The first objective is to fund the nonfederal share of payments needed to restore IHSS hours that were eliminated as a result of the current 7 percent reduction. The nonfederal cost for restoring the hours is estimated to be $216 million in 2015–16.
- Maintain Current General Fund Offset in Medi–Cal. The second objective is to maintain the General Fund offset from the current tax. This offset is estimated to be $1.1 billion in 2015–16.
Next, we discuss key features of the Governor’s proposed MCO tax structure.
Impose Tax on Most MCOs. To establish a generally redistributive structure, the Governor proposes to impose the new tax on most MCOs, defined as full–service health plans regulated by the Department of Managed Health Care (DMHC) or DHCS. (For a more detailed description of the types of entities covered by the proposed tax, see the box on page 25.) As described below, the Governor proposes to exclude Medicare managed care plans from the restructured tax base (as allowed under federal rules), which effectively exempts MCOs that only offer these types of products. The proposal would also exempt specialized MCOs that offer only limited services such as vision and dental coverage, and health insurance products regulated by the California Department of Insurance. Finally, the proposal would exempt several full–service MCOs that provide cross–border coverage to enrollees in Mexico. This last exemption requires a CMS–approved waiver of the broad–based requirement. After accounting for these specific and effective exemptions, 39 MCOs would be subject to the restructured tax, compared to 27 that are subject to the current tax.
Unit Tax on Quarterly Member Months. Unlike the current MCO tax, which is based on a percentage of MCOs’ gross revenue from Medi–Cal, the proposed tax is a unit tax based on each MCO’s quarterly member months of enrollment. (A “member month” is defined as one member being enrolled for one month in an MCO. For example, a family of five enrolled for a full quarter generates 15 member months.) Each MCO’s tax base will include all its member months for the quarter except those enrolled in (1) Medicare managed care plans and (2) plans that subcontract with other MCOs that bear ultimate responsibility for the enrollees.
Tiered Structure Based on Enrollment Size. Under the proposal, the tax per member month will neither vary by payer or product line—such as Medi–Cal versus commercial coverage—nor across different types of MCOs, such as for–profit versus nonprofit. However, the proposal calls for a tiered structure in which the unit tax per additional member month rises, then falls with increasing MCO enrollment. The draft language specifies the tax tiers and per unit amounts for 2015–16, which are shown in Figure 11. For example, an MCO with 1 million taxable member months during a particular quarter in 2015–16 would pay $3.50 per unit for the first 125,000 member months, $25.25 per unit for the next 150,000 member months, and $13.75 per unit for the remaining 725,000 member months, resulting in a total payment of $14.2 million for that quarter. This tiered structure requires a CMS–approved waiver of the uniform requirement.
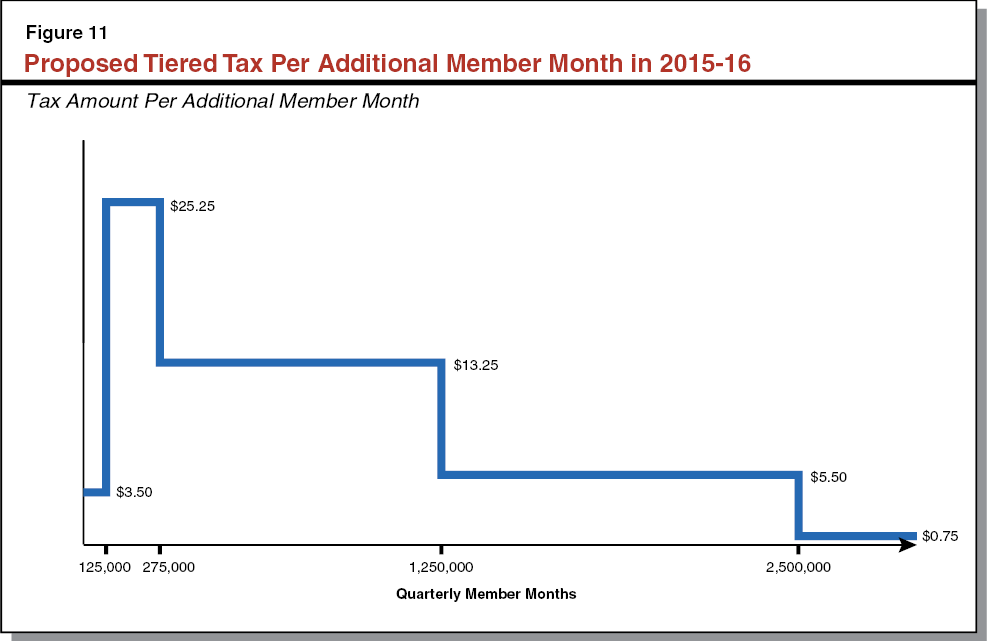
Figure 12 shows the distribution of MCOs in terms of taxable member months per quarter under the proposal. The average quarterly tax base for MCOs that participate extensively in Medi–Cal managed care is around 1 million member months. One intent of the tiered structure is to place a disproportionate share of the tax’s burden on these MCOs, since much of their tax payment can (1) draw down FFP and (2) be fully reimbursed to the MCOs through Medi–Cal capitation increases, as described immediately below.
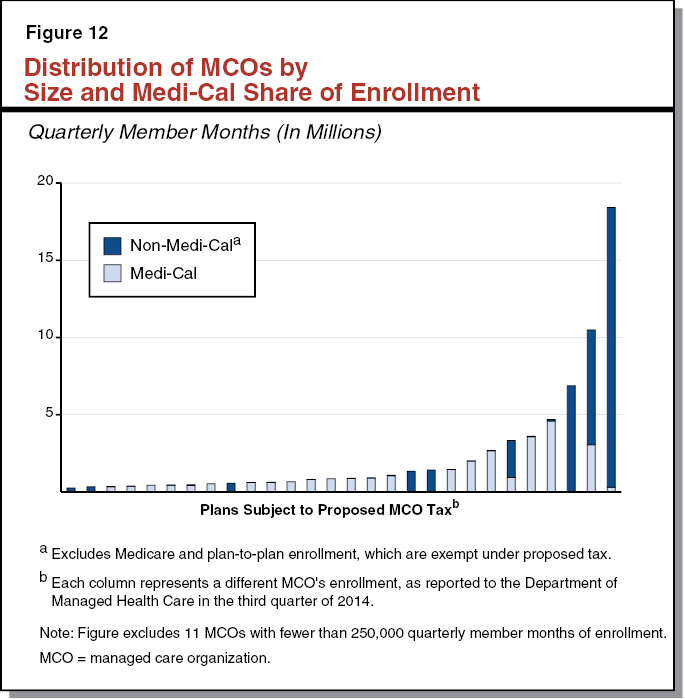
Continue Reimbursing MCOs for Medi–Cal Portion of Tax. . . Normally, under the no–hold–harmless provision, Medicaid payments cannot be directly related to the amount of health care–related taxes owed by providers. However, federal rules also require that qualified actuaries certify Medicaid managed care payments as being “actuarially sound” before these payments may receive FFP. In practice, this involves the actuaries’ assessment that the rates reflect MCOs’ reasonable costs of doing business in Medicaid—including state–mandated taxes and assessments. Under the Governor’s proposal, for each member month enrolled in Medi–Cal managed care, the state would continue to build the cost of the per–unit tax into the MCO’s capitation payment. The DHCS indicated that this policy is permitted by CMS in recognition that Medi–Cal managed care rates must be certified as actuarially sound. However, DHCS reiterated that federal rules bar the state from holding MCOs harmless for the tax on member months outside of Medi–Cal managed care, such as those enrolled in commercial coverage.
. . .And Generally Minimize Impact on MCOs. The draft language states the intent that the tax structure—to the extent possible while meeting federal requirements and the tax’s dual objectives—minimizes the aggregate financial impact on MCOs subject to the tax. Besides concentrating the tax burden on midsized MCOs that can leverage FFP and recover their tax payments through Medi–Cal managed care, the tiered tax would also serve to lessen the proportionate impact on small and large MCOs. This is because the smallest MCOs (fewer than 125,000 quarterly member months) would face a uniform tax of only $3.50 per unit, while the largest MCOs (more than 5 million quarterly member months) would face a low average tax per unit, as over half their enrollment would be taxed at just $0.75 per unit.
Tax Administered by DHCS and DMHC, With Periodic Adjustments. Because the restructured tax would no longer be connected to the sales tax, it would be formally administered by DHCS instead of BOE. The draft language would authorize DHCS to adjust the tax as necessary to raise sufficient revenue to fund the two main objectives, and require the department to report these changes during the annual budget process. The language also states that DHCS will consult with DMHC in developing the tax tiers for future years, and authorizes DHCS to delegate much of the tax’s administration to DMHC, including the actual collection of the tax. (The administration suggested DMHC may be best suited for this role, since DMHC already obtains enrollment data from MCOs and collects annual assessments based on this enrollment.)
Permanent and Swift Authorization. The administration seeks to permanently authorize the proposed tax, effective July 1, 2015. (Therefore, the draft language would render the current MCO tax inoperative a year earlier than the existing sunset.) The administration submitted a letter along with its draft legislation stating that it “will work with the Legislature to pass the enclosed legislation as early as possible in the legislative session.” In urging the Legislature to swiftly adopt the proposal, the administration cites the settlement agreement related to the 7 percent reduction in IHSS—specifically, the deadline under the agreement for the state to submit an assessment to CMS by April 1, 2015.
In the discussion that follows, we draw contrasts between the Governor’s proposal and the state’s other health care–related taxes. We use these contrasts to point out that the proposal would likely have fiscal and economic impacts that extend beyond the total revenue raised and used for budgetary purposes. While we did not undertake a rigorous study of these impacts, we are able to comment on their general direction and rough order of magnitude. With these impacts and other features of the tax in mind, we assess the Governor’s proposed use for the revenues. We also examine issues surrounding the ongoing goals and administration of the tax beyond 2015–16, and the Governor’s push for the Legislature to promptly and permanently authorize the tax.
Proposal Likely to Meet Federal Approval. . . We believe the Governor’s proposal is likely consistent with a federally permissible health care–related tax. Using the 2015–16 tax tiers specified in the draft language, we performed a rough version of the calculation prescribed under federal regulations for a broad–based and uniform waiver. We caution that our informal calculation is not a substitute for DHCS’s official demonstration to CMS of the tax’s permissibility. However, it does suggest to us that the structure appears generally redistributive in 2015–16. We also believe the proposal satisfies the no–hold–harmless provision. As mentioned earlier, the state is actuarially required to incorporate the cost of the tax into payments for Medi–Cal managed care. There is no indication that the proposal would further compensate MCOs for the rest of their tax liability.
. . . And in Doing So Necessarily Creates Losers. The current MCO tax is economically neutral to all 27 MCOs paying the tax—that is, there are no net winners or losers among these current taxpayers. The Governor’s proposal to restructure the tax results in no winners—and some clear losers—among the 39 MCOs that would be affected by the proposal. Figure 13 contrasts the funding flows between the current versus proposed tax for 2015–16.
Figure 13
Comparison of Current and Proposed MCO Tax in 2015–16
Inflows/(Outflows), (In Millions)
|
Current MCO Tax
|
|
State Funding Flow
|
Special Fund
|
General Fund
|
Federal Funds
|
|
Capitation increases for Medi–Cal managed care
|
—
|
($705.7)
|
($1,203.4)
|
|
MCO tax revenue collection
|
$1,909.1
|
—
|
—
|
|
Reimbursement of General Fund for capitation increasesa
|
(657.0)
|
657.0
|
—
|
|
Reimbursement of General Fund for other Medi–Cal costsa
|
(1,133.1)
|
1,133.1
|
—
|
|
Financial Impact to MCOs
|
Gain / (Loss)
|
|
|
|
Capitation increases for Medi–Cal managed care
|
$1,909.1
|
|
|
|
MCO tax revenue collection
|
(1,909.1)
|
|
|
|
Net Impact to MCOs
|
$0
|
|
|
|
Proposed MCO Tax
|
|
State Funding Flow
|
Special Fund
|
General Fund
|
Federal Funds
|
|
Capitation increases for Medi–Cal managed care
|
—
|
($371.7)
|
($691.2)
|
|
MCO tax revenue collection
|
$1,720.9
|
—
|
—
|
|
IHSS restoration
|
(215.6)
|
—
|
267.5
|
|
Reimbursement of General Fund for capitation increases
|
(371.7)
|
371.7
|
—
|
|
Reimbursement of General Fund for other Medi–Cal costs
|
(1,133.1)
|
1,133.1
|
—
|
|
Financial Impact to MCOs
|
Gain / (Loss)
|
|
|
|
Capitation increases for Medi–Cal managed care
|
$1,062.9
|
|
|
|
MCO tax revenue collection
|
(1,720.9)
|
|
|
|
Net Impact to MCOs
|
($658.0)
|
|
|
If the current MCO tax were kept in place for 2015–16, MCOs would pay and receive back $1.9 billion in revenue. Therefore, they would owe nothing in terms of effective tax liability. In contrast, the administration estimates the proposed tax would raise $1.7 billion of gross revenue in 2015–16, with MCOs receiving back $1.1 billion of their tax payment through Medi–Cal capitation increases. Thus, under the proposal, the dollar value of the effective tax liability (after subtracting Medi–Cal repayments via capitation increases) across MCOs would be $658 million.
The administration projects this effective tax liability to equal half a percent of the MCOs’ combined gross operating revenues. This includes revenue from all lines of MCO business, including Medicare (which would be exempted from the tax) and Medi–Cal (for which MCOs would be made whole). However, Figure 12 suggests there are several midsized MCOs that (1) would bear the full brunt of the highest tax tier, (2) have little to no Medi–Cal enrollment to reduce their effective tax liability via capitation increases, and (3) do not have much enrollment beyond the first million member months to lower their average tax rate. The administration estimates that the effective tax rate for these types of MCOs could be as high as 4 percent.
Proposal Is No Longer Solely a Medi–Cal Financing Scheme. . . For the reasons above, the Governor’s proposal is unlike other health care–related taxes imposed by the state. The hospital and SNF quality assurance fees mainly create winners among the taxed providers. The hospital fee finances the nonfederal share of supplemental Medi–Cal payments to hospitals. While not every single hospital subject to the fee may receive a net benefit from these payouts, the industry as a whole is estimated to be $2 billion better off from having the fee in place (after subtracting the fee’s General Fund offset for children’s coverage). A similar situation applies to SNFs, which receive annual Medi–Cal rate increases that are partially financed by their fee payments.
Ultimately, the point of these arrangements is to shift the cost of providing mutual benefits—rate increases for providers and General Fund offset for the state—entirely to the federal government. In contrast, the Governor’s MCO tax proposal would leverage only $691 million in federal funds to support $1.3 billion of the state’s benefit and priorities. The remaining $658 million would be initially borne as a net cost by 14 MCOs.
. . .But in Part Resembles an Actual Tax on Commercial Coverage. . . Under the proposal, the MCOs’ effective tax liability of $658 million would come only from the tax they pay on commercial member months. The state cannot reimburse MCOs for these non–Medi–Cal payments due to the no–hold–harmless provision. Therefore, the proposal’s main economic effect on MCOs would resemble that of an actual per–unit tax on commercial health coverage. As discussed earlier, the administration characterizes the effective tax rate on MCOs as a percentage of their gross revenue from all payers. However, because the effective tax liability would only increase with each additional member month of commercial coverage, the more relevant number for MCOs—economically speaking—is the tax as a percentage of commercial revenue. While we did not have revenue data broken out by lines of business for specific MCOs, our rough estimate for the effective tax rate as a percentage of aggregate commercial revenue is 1 percent.
. . .Partly Passed on to Purchasers of This Coverage. . . In many cases, businesses that are legally required to pay taxes on certain products pass them on to customers through increased prices for those products. We believe that in the long term, purchasers and enrollees of commercial MCO coverage would likely bear much of the burden of the proposed MCO tax through higher premiums. That being said, the overall impact on premiums across the commercial market may be less than 1 percent. This is because the entire $658 million in tax burden may not be passed on by MCOs, due to market forces and other factors.
. . .Including the State. The state pays for a large portion of health coverage costs for its workers, their families, and state retirees. In 2014–15, the estimated General Fund cost for these health benefits was $2.6 billion. Much of this coverage is provided by the three largest MCOs in the state, which would face relatively low tax rates due to their high enrollment levels. If MCOs were to pass the proposed tax on to commercial payers through higher premiums, we think a reasonable order of magnitude for potential increases in General Fund spending on state worker and retiree health benefits is in the low tens of millions of dollars annually.
Governor’s Objectives Are Important. Our point in properly characterizing the Governor’s proposal is twofold. One, the Legislature needs to understand that the proposal is not solely a Medi–Cal financing scheme, but in part resembles an actual tax to be borne by some MCOs and potentially passed on to their purchasers and enrollees. Two, the Legislature should weigh these effects against the purposes the tax would fund. The objectives outlined by the Governor carry important fiscal, policy, and legal ramifications. The MCO tax provides General Fund relief for current Medi–Cal spending. For 2015–16, the tax offsets General Fund spending by 5 percent of what it otherwise would have been. Absent the tax the state would have to find alternative revenue sources or consider General Fund program reductions of a comparable amount. In addition, the state would lack a dedicated non–General Fund funding source for the IHSS restoration, as called for under the legal settlement.
Governor’s Funding Concept Comes With Some Social Cost. . . From a social standpoint, taxes sometimes have undesirable features, such as distorting behavior and placing disparate burdens on otherwise similar taxpayers. In the case of the Governor’s proposal, the MCO tax’s effects may be somewhat muted for most purchasers and recipients of commercial coverage. To the extent that MCOs pass on the tax, the burden would be distributed across the large and diverse commercial market. (Approximately 12 million Californians are enrolled in commercial MCO coverage.) In many cases, the tax could be “hidden” from employers and individuals, due to its slight effect on premiums. In other words, the tax may not lead them to make very different decisions about their health coverage. However, these effects would vary, since the tiered tax would place different burdens on individual MCOs. For example, two MCOs with similar levels of enrollment and revenue—but different shares of Medi–Cal enrollment—would owe substantially different tax.
. . .But Substantial Fiscal Merit. From a fiscal standpoint, the overall concept behind the proposal has strong points. While the state could experience minor increases in health care costs for employees and retirees, these would be dwarfed by the tax’s General Fund offset. The tax base of MCO enrollment should be fairly stable, due to the ACA’s requirement for individuals to have health coverage. Most importantly, the proposal only requires raising $658 million in taxes to generate $1.3 billion for the state’s use, with the remainder being subsidized by the federal government. Weighing the fiscal merits against the social costs, we find, on balance, that the Governor’s approach for a restructured tax is a reasonable one and worthy of the Legislature’s consideration.
However, Ongoing Funding Goals Not Explicit. . . The draft language states that DHCS—on an annual basis—“shall determine the taxing tiers and per enrollee tax amounts for each tier…in order to achieve the goals specified” in the language. While the revenue targets for these goals are clear in 2015–16, the language is mostly silent on how the amounts will be determined in the out–years. To fully fund the 7 percent restoration on an ongoing basis, the tax would have to keep pace with caseload and wage growth in IHSS. With respect to the General Fund offset for Medi–Cal, the language states the intent that the tax “[g]enerate an amount of nonfederal funds for the Medi–Cal program equivalent to the funds generated” by the current MCO tax. Under one interpretation, the administration might calculate the offset that would have been achieved had the current MCO tax—3.9 percent of Medi–Cal managed care revenue—remained in place for each fiscal year. The Legislature should recognize that over time, such a calculation would grow above $1.1 billion, given that Medi–Cal managed care revenues will increase with caseload and health care inflation.
. . .Obscuring How Ongoing Administration Would Work. . . One key limitation of per–unit taxes is that revenue only increases when (1) the number of units being taxed go up or (2) the government raises the amount of tax per unit. If the goal of the proposal is to maintain—dollar for dollar—the amount of offset that the current MCO tax would have achieved, then DHCS would likely have to recalibrate the tax tiers and amounts in future years. This is because the number of units being taxed—MCO member months—would only grow at a modest rate with the general population, and lag behind the inflationary growth in revenue collected under the current MCO tax. Based on our understanding, even minor adjustments to the tax tiers or amounts could require DHCS to submit a new broad–based and uniform waiver to CMS. This constant process of recalibration and resubmissions could become very complicated for DHCS to implement, even with DMHC’s support.
. . .Raising Questions About Permanent Authorization. . . We have concerns about permanently adopting the administration’s language in its current form. As noted above, the language omits any targets or clear benchmarks for how much revenue is to be raised in the future. This, in turn, invites scrutiny as to whether DHCS has sufficient direction and capacity to effectively administer the tax in the long term. The proposal’s lack of clarity about the out–years may reflect the administration’s overriding focus on funding the General Fund offset and IHSS restoration in 2015–16. While these immediate goals are important, they do not obviate the need to carefully consider the tax’s operation from a multiyear perspective.
. . .And Passing the Tax Under Hurried Timeline. The administration’s letter does not suggest a specific date for the Legislature to pass a restructured MCO tax. However, in informal discussions, some administration officials indicated to us the goal of a March enactment. Though the administration projects a sense of urgency, possibly because of the April 1 deadline to submit the assessment to CMS under the IHSS settlement agreement, we are unclear about the practical ramifications of missing this deadline—as explained below.
Missing April Deadline in Settlement Poses Uncertain Legal Risk. . . We acknowledge that there is a legal risk involved in the Legislature failing to enact the Governor’s MCO tax proposal before April. Under this scenario, the terms of the agreement require the administration and plaintiffs to reach a resolution of some kind. If a resolution is not reached, then the plaintiffs (or the administration) could submit the dispute to the district court to fashion “appropriate remedies needed to facilitate the submission of the assessment to CMS for approval.” Under such a situation, it is unclear what specific remedies the district court judge may pursue.
. . .But Seemingly Few Repercussions in Practical Terms. We do not foresee additional General Fund exposure if the assessment—which really means the broad–based and uniform waiver for the restructured MCO tax—is not submitted to CMS by April 1. The state could reach a resolution with plaintiffs by clarifying that the tax need only be passed by August for both (1) the waiver to be submitted on time to CMS, and (2) tax collections to begin on schedule. Again, under federal Medicaid regulations, September is the real deadline for the state to submit a waiver to CMS that is retroactively effective to the start of July. Moreover, under the administration’s own draft language, MCO tax collections would not commence until December 1, 2015 at the earliest. Regardless of when the waiver is approved, the General Fund would pay for at least the first few months of the IHSS restoration, and then be reimbursed in arrears from the MCO tax proceeds. This would be similar in some ways to the process leading to the current hospital quality assurance fee. While the 2013–14 Budget Act adopted the General Fund offset from the fee, the policy bill implementing the fee was enacted in October 2013, and the fee’s broad–based and uniform waiver was submitted to CMS in December 2013.
Pass a Tax With Core Features of Governor’s Proposal… We recommend that the Legislature—no later than the end of August—approve a restructured MCO tax that contains core features of the Governor’s proposal. The structure appears to be federally permissible and would provide important General Fund relief. Though the proposal comes with some social cost it would provide substantial fiscal benefit. To aid multiyear planning and stability, we recommend the Legislature approve a tax structure for at least five years. Failing to replace the current and impermissible MCO tax would not affect the General Fund offset for 2015–16. However, it would leave a funding gap for the nonfederal share of the IHSS restoration, potentially embroiling the state in further legal disputes and adding to General Fund liability.
. . .But First Understand its Impacts. In this analysis, we have provided the Legislature with a framework for understanding the Governor’s proposal. The key takeaway is that the proposal is not solely a mere financing scheme for Medi–Cal. Rather, it partly resembles an actual tax on commercial health coverage, with broader economic and social implications. It appears that the administration may be citing the April 1 date in the IHSS settlement as a reason to pass the restructured tax quickly. While there is technically some legal risk tied to this date, we think this could be defused in a straightforward resolution that lays out the actual milestones of legislative and federal approval—August and September, respectively—necessary for the tax to be operative throughout 2015–16.
Meanwhile, prior to adopting a tax, the Legislature should ask the administration to respond to some important questions. In our view, the most crucial questions revolve around how the tax would operate in the out–years, given the language’s ambiguity about future revenue targets, and the seemingly complex task of rebasing the tax annually while ensuring its permissibility. However, even for 2015–16, the Legislature should be mindful of the tax’s distributional consequences. We pointed out that some midsized MCOs could see effective tax rates as high as 4 percent. To some degree, this is inevitable under a generally redistributive structure that maximizes FFP. Nonetheless, it is worth the Legislature’s time to understand these issues as it moves to enact the tax—especially since many individuals and families may obtain commercial coverage from these MCOs. We also believe the administration needs to be transparent about what its own modeling shows for the potential burden on individual MCOs. While DHCS declined to share their detailed model with us at the time of this analysis, the Legislature should request these data during the budget hearings.
Permanent Authorization Not Warranted in Present Form. Until the administration provides satisfactory answers to the above questions, we advise against permanently adopting the language in its current form. We also recommend the Legislature work with the administration to refine the language in ways that could simplify the tax’s ongoing administration. For example, the Legislature could explore whether it is possible to set revenue targets—and tax tiers and amounts—for five years instead of one. This would give a clearer sense of the future benefit to the General Fund, and would require CMS approval of just one waiver for the five–year period.
The amount of federal CHIP funding available in 2015–16 is uncertain pending actions by Congress to appropriate additional funds for CHIP. Further, the longer–term future of CHIP remains uncertain as the federal government weighs the potential for transitioning children currently covered by CHIP into other sources of health coverage, such as subsidized coverage through Covered California. In this analysis, we discuss the short– and long–term implications for the state’s CHIP depending on future congressional actions.
CHIP Provides Health Insurance to Low–Income Children. The CHIP is a joint federal–state program that provides health coverage to children in low–income families, but with incomes too high to qualify for Medicaid. States have the option to use federal CHIP funds to create a stand–alone CHIP program or to expand their Medicaid programs to include children in families with higher incomes (commonly referred to as Medicaid–expansion CHIP). Recently, California transitioned from providing CHIP coverage through the stand–alone HFP to providing CHIP coverage through Medi–Cal. With this transition, completed in the fall of 2013, Medi–Cal generally provides coverage to children in families with incomes up to 266 percent of the FPL. Some infants in families with incomes up to 322 percent of the FPL may also be eligible for Medi–Cal. (The FPL in 2015 for a family of four is $24,250.)
Federal Matching Rate for CHIP Is Higher Than for Medicaid. . . Currently, the federal government provides a 65 percent federal matching rate for CHIP coverage (roughly a two dollar match for every dollar the state spends). Whereas for other Medi–Cal covered children, California generally receives a 50 percent federal matching rate (a one dollar match for every dollar the state spends).
. . .But CHIP Funding Is Capped. Unlike Medi–Cal, CHIP is not an entitlement program. States receive annual allotments of CHIP funding based on historic CHIP spending. Generally, states receive allotments that are sufficient to cover the federal share of CHIP expenditures for the full year. Allotments correspond to the federal fiscal year (FFY) which runs from October 1 through September 30. If a state does not spend its full annual allotment in the given year, the state may continue to draw down unspent funds in the next year. The DHCS estimates that there will be over 1.1 million children enrolled in Medi–Cal in 2015–16 who receive services funded at the 65 percent matching rate. Throughout this analysis, we refer to this population as the “65/35 Medi–Cal” population. Other children enrolled in Medi–Cal receive services funded at the 50 percent matching rate. Throughout this analysis, we refer to these children as the “50/50 Medi–Cal” population.
Children’s and Parents’ Income Eligibility for Public Health Coverage. Families’ eligibility for public health coverage (Medi–Cal or subsidized coverage through Covered California) can be grouped into three categories, as shown in Figure 14.
- Both Children and Parents Eligible for Medi–Cal. In families with incomes up to 138 percent of the FPL, both children and their parents are eligible for Medi–Cal.
- Children Eligible for Medi–Cal and Parents Eligible for Subsidized Coverage Through Covered California. In families with incomes above 138 percent of the FPL and up to 266 percent of the FPL, children are eligible for Medi–Cal and their parents are eligible for subsidized coverage through Covered California. (We note that some children aged zero through two may be eligible for Medi–Cal in families with incomes up to 322 percent of the FPL.)
- Both Children and Parents Eligible for Subsidized Coverage Through Covered California. In families with incomes above 266 percent of the FPL and up to 400 percent of the FPL, both children and parents are eligible for subsidized coverage through Covered California.
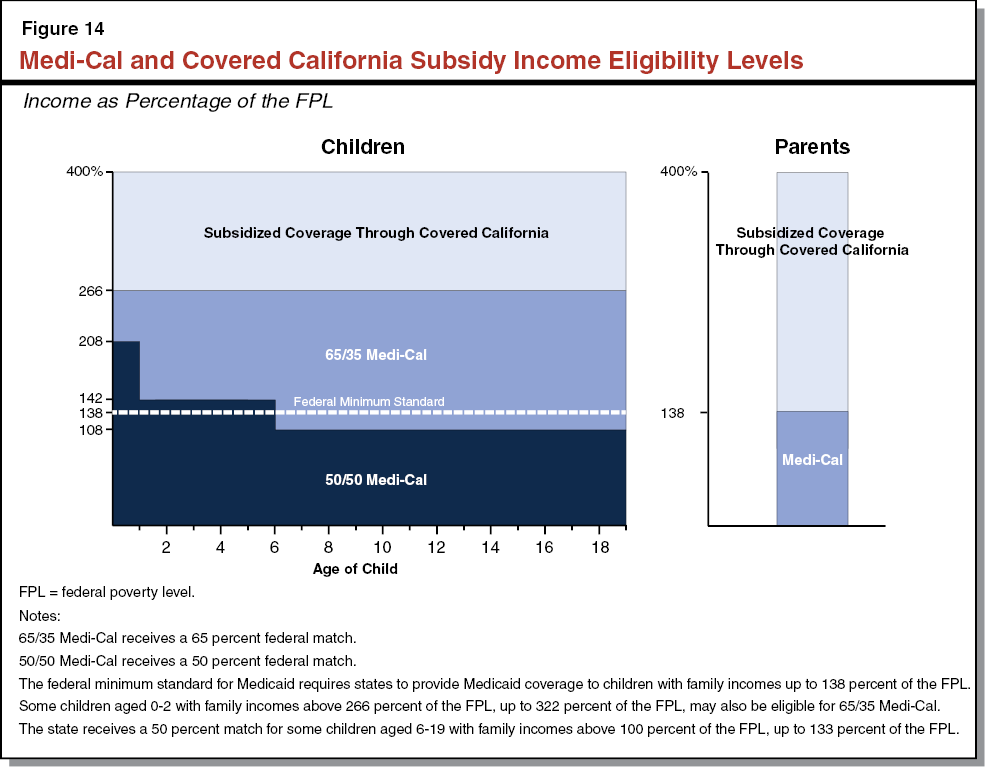
As a result of recent changes associated with ACA, there is uncertainty around whether CHIP will continue to be funded by the federal government. The subsidized health coverage provided under ACA (through Covered California) offers an alternative way to provide health coverage to children currently covered through CHIP (in California, this is the 65/35 Medi–Cal population). However, there are also several issues with transitioning children from CHIP coverage to subsidized health coverage, such as the cost–sharing requirements for families. (We discuss these issues in more detail later in this analysis.) In the short term, the amount of federal funding for CHIP available to California in 2015–16 is uncertain. Over the longer term, it is uncertain whether and for how long Congress will continue to fund CHIP.
ACA Appropriated Federal Funds for CHIP Through FFY 2015. The ACA appropriated federal funding for CHIP through FFY 2015, which ends September 30, 2015. In order for states to receive annual CHIP allotments beyond FFY 2015, Congress must appropriate additional funds for the program. The state can carry over any remaining CHIP funds from the FFY 2015 allotment into FFY 2016. Once these federal funds are exhausted, there will be no additional CHIP funds available to states unless Congress appropriates additional funds.
ACA Authorizes Increased Federal Matching Rate for CHIP Beginning in FFY 2016. Beginning in FFY 2016, ACA authorizes an increased federal matching rate for CHIP through FFY 2019. Under ACA, California’s CHIP federal matching rate would increase from 65 percent to 88 percent during this period. The ability to draw down federal CHIP funds at this higher matching rate is dependent on Congress’s decisions regarding the appropriation of funding for CHIP beyond FFY 2015. The implications of this for California’s budget are discussed in the next section.
ACA Required Part of CHIP Population to Be Covered Through Medicaid. Under ACA, states must provide Medicaid coverage to children up to age 19 with family incomes up to 138 percent of the FPL (which is referred to as the “federal minimum standard”). Previously, children aged 6 to 19 with family incomes between 108 percent and 138 percent of the FPL could be covered through states’ CHIP programs. The federal government currently pays the higher CHIP matching rate (65 percent in California) for this population. States will be required to continue providing Medicaid coverage to this population at the lower Medicaid matching rate (50 percent in California) if CHIP funding runs out.
ACA Maintenance–of–Effort (MOE) Requirements for CHIP and Medicaid. Under an ACA MOE provision, states are required to maintain their March 23, 2010 Medicaid and CHIP eligibility levels for children through September 30, 2019. However, the implications of this MOE may vary between states with stand–alone CHIP programs and states with Medicaid–expansion CHIP programs. According to the federal Medicaid and CHIP Payment and Access Commission (MACPAC), a nonpartisan congressional advisory commission, states with stand–alone CHIP programs would not be required to continue providing coverage to CHIP–eligible children with family incomes above the federal minimum standard if federal CHIP funding runs out. However, states that serve the CHIP–eligible population through their Medicaid programs would be required to continue to cover the entire CHIP population through September 30, 2019 at the lower Medicaid matching rate. The implications of these MOE requirements are uncertain for California because the state transitioned from a stand–alone CHIP program (HFP) to a Medicaid–expansion CHIP program after March 2010. The CMS will need to clarify the implications of the ACA MOE requirements for California if Congress does not appropriate additional CHIP funding through FFY 2019.
Longer–Term Future of CHIP Is Uncertain. The MACPAC has recommended a two–year extension of CHIP funding through FFY 2017. After FFY 2017, MACPAC expects that funding for CHIP will not be continued assuming that children with CHIP coverage can be transitioned into other sources of health coverage, such as subsidized coverage. During the two–year extension, MACPAC expects that the federal government and states can address any issues around transitioning children from CHIP coverage to ACA–subsidized health coverage. Ultimately, it will be Congress’s decision whether to fund CHIP and for how long; but MACPAC’s recommendation provides an indication that even if Congress appropriates some additional funds for CHIP, the program is not likely to continue beyond the next several years. In the next section, we discuss the implications of CHIP funding uncertainty in 2015–16. Later, we discuss the longer–term implications in more detail.
Budget Assumes Federal Funding for CHIP Continues at Current Level. . . The Governor’s budget assumes California will continue to receive a 65 percent federal matching rate for the 65/35 Medi–Cal population for the full year in 2015–16. The DHCS estimates the state will draw down nearly $2.1 billion in federal CHIP funding in 2015–16 (most of which is matched with General Fund).
. . .But Actual Level of Federal Funds Is Uncertain. Given that Congress has not appropriated funds for CHIP beyond FFY 2015, the amount of CHIP funding, if any, allotted to California for FFY 2016 is uncertain. It is certain that California will maintain the 65 percent matching rate for the 65/35 Medi–Cal population from July 1, 2015 through September 30, 2015, because this three–month period overlaps with FFY 2015. The CHIP funding for the rest of 2015–16 is less certain and could have a significant impact on the state’s budget.
Congress’s Decision on CHIP Funding Could Result in Higher or Lower General Fund Costs in Medi–Cal Budget. The decision Congress makes regarding appropriations of CHIP funding beyond FFY 2015 has implications for the state’s General Fund spending in Medi–Cal. There are three basic scenarios regarding congressional action with respect to CHIP funding.
- No New CHIP Funds Are Appropriated. If Congress decided not to appropriate additional funds for CHIP beyond FFY 2015, the state would likely face higher General Fund costs in 2015–16 than are reflected in the Governor’s budget for Medi–Cal. We assume the state would continue to provide Medi–Cal coverage to the full 65/35 Medi–Cal population in 2015–16 even if Congress does not appropriate additional funds for CHIP. This is because it would take time for the state to decide whether to transition this population to subsidized coverage through Covered California and implement the potential transition. Under this scenario, we estimate the Medi–Cal budget would likely increase by as much as $300 million General Fund in 2015–16, depending on the amount of FFY 2015 CHIP funds that the state carries over into FFY 2016.
- CHIP Funds Appropriated Are Insufficient to Fund ACA–Enhanced Federal Matching Rate for Full Year in FFY 2016. The ACA authorizes an increase in federal matching rates for CHIP beginning in FFY 2016. As described earlier, this would increase the federal matching rate for California from 65 percent to 88 percent. However, Congress could hold CHIP funding constant at current levels which are insufficient to fund the increased federal matching rate. If this were the case, General Fund spending for the 65/35 Medi–Cal population in 2015–16 would likely be similar to the level assumed in the Governor’s budget (about $950 million).
- CHIP Funds Appropriated Are Sufficient to Fund ACA–Enhanced Federal Matching Rate for Full Year in FFY 2016. Congress could decide to appropriate additional funds for CHIP and adjust states’ allotments to account for the increased matching rate authorized by ACA. If this were the case, California could draw down federal funds for the 65/35 Medi–Cal population at the 88 percent federal matching rate beginning on October 1, 2015. In this case, General Fund spending in Medi–Cal in 2015–16 would be roughly $450 million lower than assumed in the Governor’s budget.
LAO Assessment. The Governor’s approach to budgeting CHIP funding is reasonable given the uncertainty. Across the range of potential actions Congress may take on CHIP funding, the Governor’s budget assumes a middle–of–the–road scenario; however, as discussed above, federal CHIP funds available to California in 2015–16 may be more or less than assumed in the Governor’s budget. There are also longer–term implications for children’s health coverage given that CHIP may not continue beyond the next several years, even if Congress appropriates funding for CHIP beyond FFY 2015. We discuss this further in the next section.
Beyond the budget impacts of CHIP funding in 2015–16, the longer–term uncertainty regarding the continuation of federal CHIP funding raises questions about how best to provide health coverage for the 65/35 Medi–Cal population in the absence of federal CHIP funding. Even if Congress appropriates additional CHIP funding, it appears possible that CHIP will not continue to be funded beyond the next several years. During the next two FFYs, MACPAC anticipates that states and the federal government will have sufficient time to develop plans to ensure health coverage for low–income children in the absence of federal CHIP funding. There are some key issues for the Legislature to consider if the federal government does not continue to fund CHIP.
Some Younger Children With Family Incomes Above 138 Percent of the FPL Historically Covered by Medi–Cal. We note that there are some younger children with family incomes above 138 percent of the FPL who are not part of the CHIP population (see the 50/50 Medi–Cal population above 138 percent of the FPL in Figure 14). These children have historically received coverage through Medi–Cal and the state receives a 50 percent federal matching rate for these children. Under the ACA MOE requirement, the state must continue covering these children in Medi–Cal at least through September 30, 2019.
Part of CHIP Population Must Remain in Medi–Cal With a Higher State Share if CHIP Is Discontinued. Based on the federal minimum standard for Medicaid coverage, Medi–Cal eligibility must be maintained for all children in families with incomes up to 138 percent of the FPL regardless of whether CHIP funding is continued. Figure 14 shows California’s current federal matching rates by income eligibility level compared to the federal minimum standard. Those children with family incomes below the federal minimum standard for whom California currently receives a 65 percent federal matching rate must be covered in Medi–Cal at a 50 percent federal matching rate if federal CHIP funding runs out.
Remaining CHIP Population Can Continue to Receive Medi–Cal Coverage but State’s Costs Will Increase. If CHIP funding is not continued, the state may continue to provide Medi–Cal coverage to the remaining CHIP population not required to be in Medi–Cal—65/35 Medi–Cal children with family incomes above 138 percent of the FPL. In this case, the state share of spending for this population would increase as the federal matching rate would decrease from 65 percent to 50 percent. The estimated full–year increase in General Fund spending to provide Medi–Cal to the entire 65/35 Medi–Cal population at a 50 percent matching rate is roughly $400 million.
Alternatively, State May Be Able to Transition Remaining CHIP Population Into Covered California Coverage, but Several Issues to Consider. If CHIP funding is not continued, California may be able to transition 65/35 Medi–Cal children in families with incomes above 138 percent of the FPL to ACA–subsidized coverage through Covered California. The state’s ability to transition this population is dependent on the interpretation of the ACA MOE requirement. The state will need to seek clarification from CMS to understand whether CHIP children in families with incomes above 138 percent of the FPL must be covered through Medi–Cal through September 30, 2019 or if these children may be transitioned to subsidized coverage if federal CHIP funding runs out. There are several issues to consider related to the potential transfer of this population to ACA–subsidized coverage. There are three considerations in favor of transferring this population to ACA–subsidized coverage.
- General Fund Savings. Transitioning 65/35 Medi–Cal children with family incomes above 138 percent of the FPL to subsidized coverage through Covered California would result in state General Fund savings—likely in the mid to high hundreds of millions of dollars. There would be no state cost for the subsidized coverage because subsidies are funded with federal funds.
- Alignment of Coverage for Parents and Children. As shown in Figure 14, children in families with incomes above 138 percent of the FPL up to 266 percent of the FPL are eligible for Medi–Cal whereas their parents are eligible for subsidized coverage through Covered California. If 65/35 Medi–Cal children in families with incomes above 138 percent of the FPL were transitioned to ACA–subsidized coverage, both the children and their parents could obtain health coverage through the same source.
- Decrease in Total Premium Payments for Some Families. Certain 65/35 Medi–Cal children with higher family incomes are required to pay monthly premiums for Medi–Cal coverage. Transitioning 65/35 Medi–Cal children with family incomes above 138 percent of the FPL to subsidized coverage through Covered California would reduce total annual premium payments for some of these families. Under ACA, total premium contributions for families that are eligible for ACA–subsidized health coverage are capped based on income level and federal subsidies pay the balance of the premiums. However, Medi–Cal premium payments are not considered when determining a family’s total premium contribution. This is problematic for families where parents obtain ACA–subsidized health coverage through Covered California and children obtain Medi–Cal coverage with a required premium payment. In this case, the families total premium contribution is higher than it would be if both the parents and the children obtained ACA–subsidized health coverage through Covered California.
While there are reasons to consider transitioning 65/35 Medi–Cal children in families with incomes above 138 percent of the FPL to ACA–subsidized coverage, there are also reasons to continue covering this population in Medi–Cal.
- Some Children May Not Be Eligible for Subsidies. Some 65/35 Medi–Cal children with family incomes above 138 percent of the FPL may not be eligible to receive subsidized coverage through Covered California as a result of the so–called “family glitch” in the ACA. Under ACA, individuals with incomes between 100 percent and 400 percent of the FPL qualify for subsidized coverage only if these individuals have no other offers of affordable health coverage. If a parent has an individual offer of employer–sponsored insurance that is determined to be affordable by ACA criteria, then no member of that family may receive subsidized coverage. However, an individual offer of affordable employer–sponsored insurance does not necessarily mean that the parent is offered affordable employer–sponsored insurance for the whole family. In this case, there may be children with family incomes between 138 percent and 400 percent of the FPL who have no offer of affordable health coverage and who cannot access subsidized coverage through Covered California. Therefore, if 65/35 Medi–Cal children with family incomes above 138 percent of the FPL were transitioned to ACA–subsidized coverage through Covered California, some of the children may not be eligible for subsidies.
- Benefits, Cost–Sharing, and Network Adequacy. The benefits, cost–sharing requirements, and network adequacy of Covered California health plans are likely to differ from those of Medi–Cal. Prior to transitioning Medi–Cal–covered children to subsidized coverage through Covered California, it would be important to compare Covered California health plans to Medi–Cal coverage to understand the impact the transition would have on children and families in terms of cost and access to services.
It is possible that some of the issues raised above, such as the family glitch, will be resolved by the federal government prior to CHIP being discontinued. However, these are the major issues that currently need to be weighed when considering how to provide health coverage to the 65/35 Medi–Cal population with family incomes above 138 percent of the FPL if CHIP funding is not continued.
Legislature Should Begin Weighing Various Options for Children’s Coverage if CHIP Is Discontinued. Even if Congress takes action to continue CHIP funding beyond FFY 2015, it seems likely that CHIP will not continue indefinitely. Given both the immediate and longer–term uncertainty associated with CHIP, the Legislature should begin to consider how to best provide health coverage to 65/35 Medi–Cal children in families with incomes above 138 percent of the FPL should CHIP not continue. The issues for consideration discussed above serve as a guide for the Legislature’s evaluation of this issue.
Legislature Should Require DHCS to Provide Updates on CHIP at Budget Hearings. We recommend that DHCS report at budget hearings regarding: (1) the status of CHIP funding beyond FFY 2015 and (2) the implications of the ACA MOE requirements for Medi–Cal.
Background. Currently, Medi–Cal beneficiaries enrolled in managed care plans have the option to change managed care plans once per month. In many other states, Medicaid managed care enrollees are restricted from changing managed care plans during certain periods. The structure of these restrictions varies across states. Some states—such as Florida, New Hampshire, and Indiana—establish a specified window of time each year when Medicaid managed care enrollees may change plans.
Governor’s Proposal. The Governor proposes savings of $1 million General Fund in 2015–16 through the implementation of an annual 90–day managed care open enrollment period. The Governor’s proposal would restrict plan changes for certain Medi–Cal beneficiaries to an annual 90–day period which would align with Covered California’s annual open enrollment period. The Governor’s proposal would generally apply to families and children, and would not apply to SPDs, beneficiaries dually enrolled in full–scope Medicare and Medi–Cal, and the ACA adult expansion population, which consists predominantly of childless adults. Also, this proposal would only affect beneficiaries enrolled in Two–Plan and GMC counties. COHS counties are not included because there is only one Medi–Cal managed care plan operating in these counties. The Medi–Cal beneficiaries affected by this proposal are hereafter referred to as “included Medi–Cal beneficiaries.”
While the Governor’s proposal generally restricts managed care plan changes to the annual open enrollment period for the included Medi–Cal beneficiaries, the proposal would allow for plan changes outside of the open enrollment period under two circumstances.
- Newly Enrolled Medi–Cal Beneficiaries. Included Medi–Cal beneficiaries who are newly enrolled in managed care could change managed care plans once within 90 days after their initial selection of a Medi–Cal managed care plan.
- Good Cause Reasons. Included Medi–Cal beneficiaries could change managed care plans outside of the annual open enrollment period when they have “good cause” reasons for changing plans. The good cause reasons include (1) the enrollee moves out of the Medi–Cal managed care plan’s service area; (2) the enrollee’s Medi–Cal managed care plan does not cover a service the enrollee seeks because of moral or religious objections; (3) the enrollee needs to receive multiple, related services performed at the same time but not all of the services are available within the Medi–Cal managed care plan’s network; and (4) other reasons, including but not limited to, poor quality of care, lack of access to covered services, or lack of access to providers with experience caring for the enrollee’s health care needs.
Governor’s Proposal Has Potential Benefits. The Governor’s proposal has potential benefits for Medi–Cal managed care enrollees.
- Annual Open Enrollment Provides More Consistency Than Other Plan Change Restrictions. An annual open enrollment period establishes a consistent period of time when included Medi–Cal beneficiaries can change plans. The consistency of an annual open enrollment period would likely create administrative efficiencies and allow for better outreach regarding plan selection.
- Less Frequent Plan Changes May Improve Measurement of Medi–Cal Managed Care Accountability. Many measures that are used to hold Medi–Cal managed care plans accountable for the level of care provided to Medi–Cal enrollees capture only those Medi–Cal beneficiaries enrolled in the managed care plan for several months continuously. Restricting managed care plan changes to an annual open enrollment period would likely increase the number of Medi–Cal beneficiaries captured by measures of Medi–Cal managed care plan accountability, thereby allowing DHCS to assess the level of care provided to a larger portion of Medi–Cal managed care enrollees. For example, some Healthcare Effectiveness Data and Information Set (HEDIS) quality measures capture the quality of care provided only to those Medi–Cal beneficiaries enrolled in the same Medi–Cal managed care plan for 12 continuous months. The Consumer Assessment of Health Plan Satisfaction (CAHPS) survey measures managed care plan satisfaction only among those Medi–Cal beneficiaries enrolled in the same health plan for at least five of the six months prior to the survey. Therefore, both HEDIS and CAHPS measures are limited to those Medi–Cal beneficiaries who are consistently enrolled in the same Medi–Cal managed care plan for a period of time.
- Alignment With Covered California Open Enrollment Would Create Consistency. The alignment of annual open enrollment periods in Medi–Cal and Covered California would allow for a consistent period of time each year when consumers could change health plans. This is particularly relevant for families in which parents are eligible to enroll in Covered California health plans and children are eligible to enroll in Medi–Cal managed care. Through outreach from Covered California and Medi–Cal, these families would receive a consistent message about the 90–day period in which it is allowable to change health plans, thereby reducing potential confusion.
Analyst’s Recommendation. While we recognize the Governor’s proposal would limit beneficiaries’ options as to when they could change plans, on balance, we recommend that the Legislature approve the proposal given its potential benefits. Specifically, we find that this proposal would likely create administrative efficiencies resulting in $1 million in General Fund savings in 2015–16 and allow for more consistent outreach to families in which some family members are eligible for Covered California and others are eligible for Medi–Cal. Further, this proposal may result in more robust data that can be used to better hold Medi–Cal managed care plans accountable for the care provided to Medi–Cal beneficiaries.
Background. Chapter 857, Statutes of 2004 (AB 1629, Frommer), enacted a facility–specific rate structure for Medi–Cal reimbursements to SNFs. Under Chapter 857, each SNF receives a per diem rate based on that facility’s annually reported costs. (Each rate year for SNFs spans August 1 through July 31.) However, total Medi–Cal payments to all SNFs are subject to an annual limit. The limit is based on the average per diem rate across all SNFs, weighted by the facilities’ number of Medi–Cal bed days (hereafter the “weighted average rate”). Generally, the SNFs’ weighted average rate for a given rate year is capped at a set percentage above the weighted average rate from the previous rate year. (Hereafter, we refer to this capped percentage increase as the “weighted average rate increase.”) Chapter 857 also imposed the SNF quality assurance fee—a health care–related tax—on SNFs to finance part of the nonfederal share of SNF payments under the facility–specific rate structure. (For more information on health care–related taxes, see the “MCO Tax Modification” section earlier in the Medi–Cal analysis.)
Although Chapter 857 contained a sunset date of July 1, 2008 for both the fee and facility–specific rate structure, the Legislature has since extended both provisions five times, as either one– or two–year extensions. Legislation enacting one of these extensions—Chapter 717, Statutes of 2010 (SB 853, Committee on Budget and Fiscal Review)—also established the Quality and Accountability Supplemental Payment (QASP) program. Under the QASP program, SNFs that meet minimum staffing standards can earn incentive payouts from a pool of supplemental funds. The payouts are awarded based on SNFs’ performance on certain quality measures (including clinical indicators), as well as SNFs’ improvement on these measures relative to the previous year. Under Chapter 717, a portion of each year’s weighted average rate increase was to be set aside to fund the QASP payment pool. Though Chapter 717 authorized the QASP payouts to begin in the 2011–12 rate year, subsequent legislation—including Chapter 631, Statutes of 2012 (AB 1489, Committee on Budget)—delayed these payouts until the 2013–14 rate year.
Chapter 631 extended the fee and facility–specific rate structure through July 31, 2015. In addition, Chapter 631 capped the weighted average rate increase at 3 percent for the 2013–14 and 2014–15 rate years. Finally, Chapter 631 authorized QASP payouts to begin in the 2013–14 rate year, with the first payout taking place in April 2014. The DHCS set aside one–third of the weighted average rate increase for the QASP payment pool. The set–aside amount was $43 million in the 2013–14 rate year, and $90 million in the 2014–15 rate year. In the 2013–14 rate year, about 480 out of 1,000 SNFs earned $43 million in QASP payouts.
Governor’s Proposal. The Governor proposes to extend the fee, facility–specific rate structure, and QASP program for SNFs through July 31, 2020, thereby authorizing a five–year extension. The Governor also proposes to make the following modifications to these provisions.
- Raise Weighted Average Rate Increase. The weighted average rate increase would be capped at 3.62 percent annually throughout the proposed five–year extension.
- Freeze QASP Payment Pool. The set–aside amount for the annual QASP payment pool would no longer be defined as a portion of the weighted average rate increase. Instead, the proposal would fix the set–aside amount at $90 million annually (the size of the QASP payment pool for the 2014–15 rate year) throughout the proposed five–year extension.
LAO Assessment. At the time of this analysis, we do not have any issues to raise with the Governor’s proposal. We will continue to review the proposal and provide the Legislature with an updated analysis if we find changes to the proposal are warranted.
The President’s recent executive actions on immigration include actions that allow certain undocumented immigrants to request deferred action and employment authorization. Deferred action status provides temporary relief from deportation. The President’s executive actions expand the Deferred Action for Childhood Arrivals (DACA) program and create the Deferred Action for Parents of Accountability (DAPA) program (also known as the Deferred Action for Parents of Americans and Lawful Permanent Residents program) as follows:
- Expands DACA Program. Previously, undocumented individuals who were younger than 31 years of age as of June 2012, had entered the United States prior to the age of 16, and had lived in the United States continuously since January 1, 2010, were eligible for DACA. The President’s executive actions expand the population eligible for DACA to include people of any age who entered the United States before the age of 16 and meet the other DACA requirements. The President’s executive actions also extend the period of DACA eligibility and work authorization from two years to three years.
- Creates DAPA Program. The President’s executive actions also create the DAPA program, which allows undocumented immigrants who have lived in the United States continuously since January 1, 2010 and are parents of United States citizens or lawful permanent residents to request deferred action and work authorization for three years.
Lawsuit Challenges President’s Executive Actions on Immigration. A lawsuit was filed recently by officials of 26 states who contend the President’s executive actions violated the United States Constitution as an overreach of executive powers. The suit seeks an order blocking the immigration changes from taking effect. Initial arguments in the suit were heard by a United States district judge on January 15, 2015, where the states asked the judge to block the executive actions until they have been able to challenge the actions in court. At the time of this analysis, the judge had not issued a ruling. Officials from 12 states, including California, and the District of Columbia recently filed an amicus or “friend of the court” brief supporting the President’s executive actions.
Budget Does Not Include Potential Costs Related to President’s Immigration Actions. The Governor’s budget does not include funding for potential costs related to the President’s executive actions on immigration. Under existing law, some undocumented immigrants affected by the President’s executive actions—if such withstand legal challenge—may newly qualify for full–scope Medi–Cal, IHSS, and/or the Cash Assistance Program for Immigrants. The benefits received by undocumented immigrants through these programs are almost entirely funded by the state and would therefore result in additional General Fund costs of an unknown amount. Below, we discuss the multistep process eligible undocumented individuals must complete to receive state–funded benefits, and the uncertainty involved in estimating the number of people completing each step of this process. It is as a result of this multistep process and the associated uncertainty that the General Fund costs to provide state–funded benefits to this population are unknown at this time.
Estimates Not Yet Available for Population Affected by Executive Actions. At the time of this analysis, detailed estimates of the population eligible to apply for DACA or DAPA status under the President’s executive actions were not available. We note that researchers at the University of California, Los Angeles and the University of California, Berkeley have a forthcoming report that will provide estimates of the size of this population as well as demographic characteristics. This report will also provide estimates of the portion of this population that would be eligible for Medi–Cal.
Processing of DACA and DAPA Applications May Take up to a Year, Creating Delay Before Eligible Individuals Could Apply for State–Funded Benefits. The United States Citizenship and Immigration Services (USCIS) expects to begin processing applications for those newly eligible for DACA in late February 2015 and for those eligible for DAPA in late May 2015. Further, the USCIS aims to process all applications for DACA or DAPA status within one year of the receipt of the application. This indicates that it will take up to a year from February 2015 before eligible individuals will be able to enroll in state–funded benefits, meaning that any significant state fiscal impact is unlikely to start prior to the second half of 2015–16.
Uncertainty Regarding Proportion of Eligible Population That Would Take Step to Apply for DACA or DAPA Status. The proportion of undocumented immigrants eligible for DACA or DAPA status under the President’s executive actions who would apply for DACA or DAPA status is highly uncertain, but history suggests that many eligible would not apply. The USCIS reports that approximately 60 percent of the current DACA–eligible population applied for DACA status in the first two years that the program was in effect. There are several reasons that may explain this relatively low rate of applications, including:
- Application Fee May Be Unaffordable for Some. To apply for DACA or DAPA, applicants must pay a $465 application fee. This application fee may not be affordable for individuals with lower incomes. One analysis of those who were eligible for DACA but did not apply found that the application fee was the most common barrier to applying.
- Government Avoidance. Although the President’s executive actions would prevent members of this population from being deported for a period of time, some eligible applicants might still be hesitant to apply for DACA or DAPA. The analysis of those eligible for DACA but who did not apply found that legal concerns and fear of providing personal information to the government were barriers to applying.
Eligible Individuals Would Also Have to Proactively Apply for State–Funded Programs. In addition to applying for DAPA or DACA status, individuals would need to take the additional step of applying for Medi–Cal and other state–funded programs in order to receive benefits from these programs. It is uncertain how many newly eligible individuals with DACA and DAPA status would apply for Medi–Cal and other state–funded programs. However, there are reasons to suggest that enrollment could be low.
- Language and Government Avoidance. Undocumented immigrants face several barriers to enrollment—including limited English proficiency and government avoidance.
- No Individual Mandate. Under current law, only United States citizens and legal residents are subject to the individual mandate to obtain health coverage and associated penalties for failing to obtain coverage. Therefore, undocumented individuals do not face the mandate’s financial consequences for not obtaining coverage, lessening the incentive to apply for Medi–Cal, particularly in cases where an individual is relatively healthy.
Medi–Cal Application Process Requires Verification of DACA or DAPA Status, Potentially Limiting Enrollment. Consistent with the application and verification process that is used for all Medi–Cal applicants, individuals applying for Medi–Cal who attest to having DACA or DAPA status would have information provided in their application verified by county Medi–Cal eligibility offices. Verification is completed using the federal data hub and where necessary through additional follow–up with federal departments, such as USCIS, and the applicant. Applicants receive full–scope Medi–Cal during the application verification process. In cases where, after due diligence, counties are not able to verify an applicant’s DACA or DAPA status, the applicant’s benefits would be reduced to restricted–scope Medi–Cal benefits—provided to all undocumented individuals—which include emergency and pregnancy–related services. This has the potential to limit Medi–Cal enrollment among the population eligible to apply for DACA or DAPA status given the barriers to applying discussed above.
LAO Analysis. Once university researchers release their report on the size and demographic characteristics of the populations affected by the President’s executive actions, the Legislature will have some information necessary to help estimate the potential fiscal effect on state program costs of the President’s executive actions. Based upon the information available at the time this analysis was prepared, it is likely the state would at most only experience partial–year costs in 2015–16 due to the rate at which DAPA and DACA applications are projected to be processed by USCIS.
Budget Includes Additional Funds for High–Cost Drugs. The Governor’s budget includes funding of $100 million General Fund in 2014–15 and $200 million General Fund in 2015–16 to pay for new breakthrough drugs, such as those used to treat Hepatitis C. The budget does not allocate this funding to specific departments. The DHCS, DPH, DSH, and the California Department of Corrections and Rehabilitation (CDCR) are already providing Hepatitis C drugs under their 2014–15 and 2015–16 budget authority. The Governor’s budget includes these additional funds, given the uncertainty around the cost and utilization of these drugs, discussed in more detail below. The individuals who may potentially be treated with the new Hepatitis C drugs include inmates in state prisons, patients in state hospitals, individuals enrolled in Medi–Cal, and individuals enrolled in the AIDS Drug Assistance Program (ADAP).
Cost of Hepatitis C Drugs Is Uncertain. The administration expects the new Hepatitis C drugs to cost approximately $85,000 per treatment regimen, making them extremely costly relative to most other prescription drugs. The state is working to obtain supplemental drug rebates for the new Hepatitis C drugs, which would lower the cost to the state, but at this time, it is unclear whether the state will be able to obtain such rebates.
Medical Guidelines Associated With Hepatitis C Drugs Are Being Revised. The administration expects the current medical guidelines for the recommended treatment of individuals with Hepatitis C to be expanded to include a broader population of individuals with Hepatitis C. This would increase utilization of these drugs relative to what was assumed in Medi–Cal, ADAP, CDCR, and other state program budgets.
Workgroup Will Provide Guidance to State on Which Patients to Treat. The administration plans to convene a workgroup that will address the state’s approach regarding high–cost drug utilization policies and payment structures. The workgroup will inform the state’s guidelines for which individuals enrolled in state programs are eligible for treatment with the new Hepatitis C drugs, and to the extent possible, the state will try to generate a consistent set of treatment guidelines that can be implemented across state programs.
LAO Analysis. We find the Governor’s approach of budgeting an unallocated set–aside to address potential costs for new drugs to treat Hepatitis C to be reasonable. However, we also find that there is considerable uncertainty regarding whether the amount of the proposed set–aside is an appropriate amount. As more information becomes available regarding the cost and projected utilization of the new Hepatitis C drugs, we will provide the Legislature with an analysis of the likely costs for state programs at the time of the May Revision.
The budget plan proposes provisional language to notify the Legislature of the expenditure of these funds as follows:
“Notwithstanding any other provision of law, items of appropriation in this act may be adjusted, as determined by the Director of Finance, to reflect changes to General Fund and Federal Trust Fund expenditures resulting from high cost medications. Adjustments authorized pursuant to this section shall be implemented upon notification to the chairpersons of the committees in each house of the Legislature that consider appropriations and the chairperson of the Joint Legislative Budget Committee.”
We find that this provisional language does not provide for sufficient legislative oversight. Specifically, the language should require notification to the Legislature—30 days prior to distribution of the funds—of the following: (1) the amount of funds being distributed, (2) a description of what the funds will be used for, and (3) the program(s) that will receive the funding.
Analyst’s Recommendation. We withhold recommendation on the amount of funds to be set aside to pay for the new high–cost drugs pending further information regarding the cost and projected utilization of the drugs. We recommend the Legislature add additional requirements to the provisional budget language proposed by the administration in order to ensure legislative oversight of these funds.
The DSH provides inpatient mental health services at five state hospitals (Atascadero, Coalinga, Metropolitan, Napa, and Patton) and at three psychiatric programs located on the grounds of CDCR prisons (Vacaville, Salinas, and Stockton). The department provides treatment to approximately 6,600 patients with a variety of mental health needs. Patients at the state hospitals fall into one of two categories: civil commitments or forensic commitments. Civil commitments are generally referred to the state hospitals for treatment by counties. Forensic commitments are typically committed by the courts and include individuals classified as incompetent to stand trial (IST), not guilty by reason of insanity (NGI), mentally disordered offenders (MDOs), or sexually violent predators. In addition, the three co–located DSH psychiatric programs treat inmates referred by CDCR. Currently, over 90 percent of the patient population is forensic in nature and there has been a steady increase in waitlists for forensic commitments. In contrast, the population of civil commitments has remained relatively stable. As of January 2015, the department had more than 550 patients awaiting placement, including about 370 IST patients.
The Governor’s budget proposes total expenditures of $1.7 billion ($1.6 billion from the General Fund) for DSH operations in 2015–16, which is roughly the same level provided in the 2014–15 budget. The department’s budget includes increased funding for several proposals, including plans to (1) operate 105 more IST beds than were budgeted in 2014–15, (2) modify an existing facility to eventually expand IST treatment capacity by an additional 232 beds, and (3) involuntarily medicate certain NGI patients.
Services for IST Patients. Under state and federal law, all individuals who face criminal charges must be mentally competent to help in their defense. By definition, an individual who is IST lacks the mental competency required to participate in legal proceedings. Individuals who are IST and face a felony charge are eligible for DSH–provided restoration services. At any given time, between 15 percent and 20 percent of the population in DSH facilities is committed as IST. The state spends about $300 million annually to provide treatment for this population—an average of about $230,000 per bed. In recent years, the department has contracted with counties and private providers to provide restoration services for IST patients through the Restoration of Competence (ROC) program. Patients in the ROC program can receive restoration services while in county jail or in a locked community facility, rather than in a DSH facility. Currently, the state spends about $8.2 million annually on the ROC program—about $91,000 per bed per year.
Long Waitlist for IST Treatment. As indicated above, as of January 2015, the department had 380 IST patients waiting to be placed in a DSH facility. Individuals on the waitlist are typically held in county jail until space becomes available in a DSH facility. Such long waitlists are problematic because they could result in increased court costs and higher risk of DSH being found in contempt of court orders to admit patients. This is because DSH is required to admit patients within certain time frames and can be required to appear in court or be held in contempt when it fails to do so. In light of these concerns, the 2014–15 budget provided $28 million for 105 additional IST beds in DSH facilities and $4 million for about 50 additional beds in the ROC program.
The Governor’s budget for 2015–16 includes proposals to expand treatment capacity in DSH for IST patients. Specifically, the budget proposes to activate existing beds at two state hospitals and build the capacity for additional beds at another state hospital.
Activation of Existing Beds. First, the budget proposes $17.3 million in additional General Fund support for the activation of 105 beds for IST patients in 2015–16. This amount includes:
- $8.6 million and 75.1 positions to activate 55 beds at DSH–Atascadero. (The administration proposes to redirect $104,000 in savings in the current year for minor retrofitting of the facility.)
- $8.7 million and 74.6 positions to activate 50 beds at DSH–Coalinga. (The administration proposes to redirect $2.9 million in savings and establish 25 positions in the current year to begin the activation process.) According to the department, these beds would be filled with MDO patients transferred from DSH–Atascadero. The beds made available from this transfer would then be filled with IST patients.
Building Secure Treatment Capacity at Metropolitan. The budget also proposes $1.9 million from the General Fund to develop preliminary plans to increase secure treatment capacity at DSH–Metropolitan, located in Norwalk, by 505 beds. This amount includes (1) 232 new beds and (2) 273 existing beds currently activated but not considered secure capacity because they are not enclosed by secure fencing. The beds would be prioritized for IST patients. The project is estimated to cost $35.5 million in total and would be completed in 2019. The staffing costs for the 232 new beds are estimated to be $48 million annually.
Once the beds provided through the project at Metropolitan were activated, as well as the above beds at DSH–Atascadero and DSH–Coalinga, the department would have a total of 337 additional beds for IST patients at an annual cost of $65 million. (We note that the Governor’s budget also proposes to activate 32 beds for individuals with developmental disabilities deemed IST at Porterville Developmental Center, a facility of the Department of Developmental Services. For more on this proposal, please see our report The 2015–16 Budget: Analysis of the Human Services Budget.)
The administration’s plan to expand DSH capacity raises several concerns. As discussed in more detail below, this is because (1) the plan would result in more IST beds than are currently needed, (2) previously funded capacity in DSH remains unused, (3) the need for the additional requested staff remains unclear, (4) unused ROC program capacity could serve some patients, (5) Proposition 47 will likely reduce the amount of capacity the department needs, and (6) the proposed capacity at DSH–Metropolitan may be unnecessary and unusable.
Proposal Results in More IST Beds Than Currently Needed. In total, the Governor’s budget provides funding for DSH to operate more than 1,900 beds for IST patients in 2015–16, and nearly 2,150 IST beds once the additional capacity at DSH–Metropolitan was activated in 2019. However, DSH currently only has 371 IST patients on the waitlist and about 1,300 IST patients in its facilities. Thus, the budget would provide the department a few hundred more beds in the budget year than is currently needed.
Previously Funded Capacity Remains Unused. In our report The 2015–16 Budget: Improved Budgeting for the Department of State Hospitals, we raise concerns that the DSH population budgeting process lacks sufficient information to assess whether the department is appropriately using its existing resources. For example, the department has historically had a large number of vacant beds—meaning beds for which they receive funding, but are not using. Although the Legislature approved funding in the 2014–15 budget for DSH to activate 242 additional beds, the DSH patient population has only increased by 41 patients (as of January 2015). In other words, the department has utilized less than 20 percent of the new capacity it was funded for in the budget. This raises questions about (1) whether the department is capable of utilizing its budgeted capacity in an effective manner and (2) whether providing funding for additional capacity will actually result in the assumed increase in the number of patients being treated.
Need for Requested Staff Remains Unclear. In our recent report on DSH’s budgeting methodology, we also noted that the staffing ratios used by the department to determine how many treatment staff are required to provide care to a specified number of patients do not account for all of the work performed by such staff. Because of this limitation, DSH typically requests funding for additional treatment staff beyond what the department’s own staffing model ratios require. It is unclear how DSH decides the number of treatment staff it needs beyond the amount required by its staffing ratios. For example, DSH is requesting 149.7 staff to serve 105 patients annually beginning in 2015–16, including 114.9 treatment staff. However, the department’s staffing ratios suggest it would only need 76.1 treatment staff. While the additional 38.8 treatment staff could be of value, the department has not provided sufficient justification for the requested level of staffing. Similarly, the department has not sufficiently justified its need for the nontreatment staff.
Unused ROC Capacity Could Accommodate Some Patients. According to DSH, the ROC program generally provides treatment services more quickly, and at a significantly lower cost, than when such services are provided in DSH facilities. In part, this is because the ROC program generally treats individuals with less serious mental illnesses who can be restored to competence in a shorter time frame. Treatment provided through the ROC program costs 60 percent less than the cost of providing similar treatment in DSH. The department is currently authorized to operate a total of about 90 beds under the ROC program, which includes 50 additional beds funded in the 2014–15 budget. We note, however, that the department has not entered into any contracts to activate the 50 additional ROC beds. Because the average length of stay for an IST patient in the ROC program is shorter than that of a patient treated in a DSH facility, these unused beds could treat a substantial number of patients. Specifically, if DSH activated and filled the 50 unused ROC beds, we estimate that the department would be able to treat about 325 additional IST patients annually. Given that ROC beds are less expensive than those in DSH facilities, the department should prioritize fully utilizing these beds before seeking funds to treat more patients in its facilities.
Proposition47 Will Likely Reduce IST Capacity Needs. As noted above, individuals who are IST and facing a felony charge are eligible for DSH–provided treatment. Such individuals are generally held in jail while awaiting transfer to a DSH facility. In contrast, individuals deemed IST for misdemeanor charges are generally released or referred for treatment in the community, which is provided by counties. Proposition 47, approved by voters in November 2014, reduces the classification of some nonserious and nonviolent property and drug crimes from a felony to a misdemeanor. As discussed below, these changes will likely reduce the number of patients eligible for DSH services.
Some IST patients now in DSH or on the waitlist were referred by the courts because they were determined to be IST for a crime affected by Proposition 47. As a result of reducing the penalties for these crimes from felony to misdemeanor, the measure will cause both the current IST patient population and waitlist to decline. For example, prior to the passage of Proposition 47, an individual may have been determined to be IST for a felony drug possession offense and committed to DSH by the courts. After the passage of Proposition 47, courts may choose to reconsider the order committing the individual to DSH since the patient is no longer facing felony charges. In such circumstances, DSH is no longer required to provide treatment, and the patient can be returned to the county. According to the department, they have already had several of these cases. Proposition 47 will also reduce the number of IST patients referred to DSH in the future. This is because some individuals found to be IST for the crimes affected by the measure will be subject to misdemeanor rather than felony penalties. As a result, the counties will be responsible for providing these individuals with restoration services.
Since the implementation of Proposition 47, the IST patient population and waitlist has declined by 72 patients—about 4 percent in less than three months. It is difficult to determine whether this decline is solely due to Proposition 47. However, the decrease is suggestive of the possible impact the measure could have on the IST population. However, DSH reports that the impacts of Proposition 47 were not taken into account when it developed its budget request. Additionally, DSH has not estimated the number of its current or waitlisted patients that will be affected by Proposition 47 or how the measure will affect the number of referrals it will receive in the future. While it is difficult to assess precisely what the impact of Proposition 47 will be on the IST patient population without such information, it will likely be significant enough to reduce the need for at least some of the additional beds proposed in the Governor’s budget.
Proposed Capacity at DSH–Metropolitan Likely Unnecessary and Unusable. It is uncertain whether the plan to modify DSH–Metropolitan would provide usable capacity for IST patients. This is because there are limits on the type of patients that DSH can place in the facility. The DSH–Metropolitan has an agreement with the City of Norwalk and the Norwalk station of the Los Angeles County Sheriff’s Department to only admit patients who have no history of attempted or successful escape from a locked facility and no charges or convictions for murder or a sex crime. According to the department, it does not anticipate having difficulty finding IST patients who fit those criteria. However, the department does not track the number of patients in its facilities or on its waitlist who are eligible for placement at DSH–Metropolitan. As a result, it is difficult to assess whether the department would be able to fully utilize the additional 232 secure treatment beds proposed for IST patients at DSH–Metropolitan once completed.
In view of the above concerns, we recommend that the Legislature (1) not approve the Governor’s proposal to expand IST capacity at DSH–Atascadero and DSH–Coalinga until the department provides additional justification and (2) reject the proposal to develop preliminary plans to expand secure capacity at DSH–Metropolitan.
Require Department to Provide Additional Justification. We recommend the Legislature require DSH to report at budget hearings this spring on the following:
- Additional Budget Information. We recommend the DSH provide (1) the number of budgeted and filled beds (particularly those authorized in the 2014–15 budget), and any justification for why the number of budgeted beds differs from the number of filled beds; and (2) detailed information about how its request for additional positions to activate the new IST capacity ties to its staffing ratios, along with justification for any staff in excess of those ratios.
- ROC Delays and Potential for ROC Expansion. We recommend the department report on why there has been a delay in activating the additional ROC beds authorized in the 2014–15 budget and on the potential for the ROC program to serve additional IST patients in the future.
- Impacts of Proposition47. We recommend DSH report what changes it has seen in the IST patient population and waitlists since the passage of Proposition 47, as well as estimates on the long–term impacts of the proposition on the IST population (such as by reviewing a sample of IST patient data to determine the proportion of IST patients who were committed for Proposition 47 eligible offenses). To the extent that DSH identifies reductions in the patient population as a result of Proposition 47, the Legislature should require the department to submit updated population budget proposals.
Once the Legislature receives the above information, it can determine how many additional IST beds and related funding—if any at all—are necessary for DSH to address its IST waitlist. To the extent the Legislature believes additional capacity is necessary, we recommend the Legislature prioritize various options for expanding capacity based on their cost–effectiveness. Specifically, we recommend first utilizing existing bed capacity, such as the additional beds authorized in the 2014–15 budget at DSH facilities and through the ROC program. The next most cost–effective option would be to further expand the ROC program, which operates at a much lower cost than state hospitals. After that, the Legislature could consider authorizing additional beds in state hospitals. The most expensive option would be pursuing capital outlay projects to expand capacity beyond what is currently available, such as the proposed DSH–Metropolitan capital outlay project.
Reject Proposal to Expand DSH–Metropolitan Secure Capacity. As discussed earlier, the Governor’s proposal to expand secure treatment at DSH–Metropolitan is estimated to cost $35.5 million to complete, and $48 million to operate annually. Given such costs relative to more cost–effective options for expanding capacity, we recommend that the Legislature reject the proposed expansion at DSH–Metropolitan at this time. As we note above, there is significant uncertainty about the department’s need for the additional capacity, and, even if such a need existed, the department may be unable to utilize the proposed capacity at DSH–Metropolitan.
NGI. The courts may determine that a defendant who has been accused of a crime is NGI in cases where it finds that the defendant was insane at the time the offense was committed. Individuals who are NGI are committed by the court to receive treatment for their mental illness, typically to a DSH facility. Patients committed as NGI can leave DSH if they: (1) have remained in DSH for an amount of time equivalent to the maximum term they would have served for the crime they committed, (2) have been found restored to sanity, or (3) are conditionally released to outpatient treatment. In all cases, the individual must be found to no longer pose a risk to themselves or others. Currently, the department treats about 1,350 NGI patients.
Involuntary Medication. Most individuals committed to DSH as NGI receive medication to treat their mental illness. In cases where NGI patients refuse to take medication, the department has the authority to compel them to do so. The department can exercise this authority when patients are: (1) unaware of their mental health condition, (2) unable to understand the benefits and risks of treatment, (3) unable to understand treatment decisions, or (4) a risk to themselves or others. Historically, the department has exercised this authority administratively for NGI patients. The decision to provide involuntary medication using an administrative process was based on a court ruling that occurred in 2000 in a case referred to as In re Locks. Specifically, the court ruled that because NGI patients are committed to DSH due to the fact that they are insane and a risk to themselves or others, they are presumed to meet the criteria for involuntary medication. As we discuss below, the In re Locks decision was recently overturned.
In contrast, DSH must seek authorization from a trial court to involuntarily medicate IST, MDO, and SVP patients. Court processes for these patients were developed after rulings in several cases found that these patients have a state constitutional right to a court hearing prior to being involuntarily medicated. Under these processes, a DSH panel first hears the case for involuntary medication. If the panel approves the case, it is then heard by a trial court. The cases are also reviewed annually by the court to assess whether continuing to involuntarily medicate the patient is appropriate.
Court Hearing Now Needed to Involuntarily Medicate NGIs. In 2014, the same court that ruled in In re Locks ruled on a separate case known as In re Greenshields. In the In re Greenshields decision, the court invalidated its previous In re Locks ruling and found that NGI patients have the same constitutional right as IST, MDO, and SVP patients to a court hearing before being involuntarily forced to take medication. The department informs us that it does not plan on appealing the ruling, and accordingly, the In re Greenshields ruling is binding. This means that the department must develop an alternative involuntary medication process—involving court review—for NGI patients.
The Governor’s budget proposes $3.2 million from the General Fund and 14.4 positions in 2015–16 for DSH to establish and implement an involuntary medication process for NGI patients that includes trial court review. These positions include clinical staff positions to provide patients with information and testimony in court, as well as legal positions to represent DSH during initial court hearings and annual review hearings. According to the administration, the NGI involuntary medication process will be based on the existing involuntary medication process for other DSH patient types.
While it is reasonable for DSH to establish an involuntary medication process for NGI patients in response to the In re Greenshields decision, the department has not provided adequate justification for the level of resources that is being requested. Specifically, the department’s proposal lacks data justifying the assumed workload increase in 2015–16 and does not account for the reduction in workload that will occur in the future.
Lack of Data Justifying Workload in 2015–16. The department does not know how many of the roughly 1,350 NGI patients statewide currently receive medications involuntarily. In addition, DSH does not know what percentage of NGI patients might refuse their medications under the new process. Thus, it is very difficult to assess the amount of workload and the number of positions required to obtain involuntary medication orders for NGI patients in the near term.
Future Reduction in Workload Not Taken Into Account. The establishment of an involuntary medication process for NGI patients could require significant workload in 2015–16, given the large number of NGI patients statewide and the potential need for a hearing for every patient that refuses medication. However, in future years, the workload associated with involuntary medication will likely decrease for two reasons. First, ongoing medication renewal orders require about 50 percent less staff time than new orders. Thus, we would expect workload associated with the current patient population to decline once all the initial orders for this population are completed. Second, once the workload associated with establishing new orders for the portion of the 1,350 current NGI patients that refuse medication is completed, the department will only need to develop new orders for the portion of the 180 new NGI patients committed to DSH each year that refuse medication. Despite these factors, the administration’s plan does not reflect a reduction in funding or positions in future years.
Given the ruling in In re Greenshields, it is reasonable for the Governor’s budget to propose some funding and staff to address the workload associated with the involuntary medication process for NGI patients. However, the budget proposal does not sufficiently justify the estimated increase in workload in 2015–16. Thus, we recommend that the Legislature direct DSH to provide a revised request for funding and staff for 2015–16 based on an analysis of the number of NGI patients expected to refuse medication. We further recommend that the Legislature only provide funding and staff positions on a one–year, limited–term basis and that it direct the department to submit a proposal for future funding as part of the 2016–17 budget. At that time, the department will have a better estimate of the ongoing workload related to the involuntary medication process.
The Licensing and Certification (L&C) Program, located within DPH’s Center for Health Care Quality, licenses and certifies health care facilities and enforces laws and regulations designed to protect the health and safety of individuals in these facilities. The Governor’s budget proposes $255 million in total funds ($3.8 million General Fund) for support of the L&C Program in 2015–16, which is a net increase of $32 million in total funds (with no change to General Fund support), or 14 percent above estimated 2014–15 expenditures. This year–over–year increase primarily results from the Governor’s four proposals to take steps to improve the quality of the L&C Program and increase L&C staffing. Below, we provide an overview of the L&C Program and then analyze the Governor’s four proposals.
The DPH’s L&C Program is statutorily required to license health care facilities that do business in California. Under a contract and a cooperative agreement with the federal CMS, DPH certifies that facilities accepting Medicare and Medi–Cal payments meet federal requirements. In conducting these licensing and certification activities, the L&C Program develops and enforces state licensure standards, conducts inspections to assure compliance with federal standards, and responds to complaints from the public against providers. The L&C Program also responds to incidents that the facilities self–report, which are known as entity–reported incidents (ERIs). The L&C Program licenses and certifies over 7,500 health care facilities and agencies in California in 30 licensure and certification categories including long–term care facilities such as skilled nursing facilities (SNFs) and intermediate care facilities for the developmentally disabled (ICF–DD). Facilities failing to meet the state or federal standards are subject to fines or other enforcement actions. The L&C Program conducts these activities in 57 counties and contracts with the Health Facilities Inspection Division within the Los Angeles Department of Public Health to perform these activities in Los Angeles County. The DPH L&C staff work out of district offices located in five geographic regions in order to provide oversight of health facilities.
As of December 30, 2014, the most recent date for which L&C staffing information is available, the L&C Program had 1,078 established positions of which 975 were filled, resulting in an overall vacancy rate of 9.8 percent. Of the 1,078 total established positions, 483, or 45 percent, are Health Facility Evaluator Nurses (HFENs). The vacancy rate for HFENs was about 3 percent. As we describe in the next section of this analysis, the total number of L&C staff is driven to a large extent by the number of HFENs needed to complete L&C workload.
L&C Staffing Based Upon Workload Estimating Model. The L&C Program projects the workload associated with all L&C programmatic functions and the corresponding number of positions needed to perform these functions. The projected L&C workload is largely determined by three drivers.
- Facility Count. The number of health facilities to survey or investigate.
- Activity Count. The number of pending and projected activities for L&C staff to perform. This is based on a projection of the number of new and renewal licensing and certification surveys and complaint investigations L&C staff will conduct in a year. The estimate also includes the workload associated with the number of pending complaints the program anticipates will roll over from prior years into 2015–16.
- Standard Average Hours. The average number of hours needed to complete a licensing, certification, or investigative activity. The L&C Program calculates this average number based on the actual average time spent on the activity and facility type in past years.
In illustration, to estimate the annual survey workload, DPH multiplies the standard average hours needed to complete surveys by the number of anticipated surveys in a year. The department then calculates the amount of additional time associated with nonsurvey functions, such as training, and adds this time to estimated total survey hours to arrive at the overall amount of time required by HFENs to complete survey activities in a given year. The number of HFEN positions is used to calculate the number of supervisors and administrative positions needed to support the HFENs who perform the bulk of L&C functions in the field. The L&C Program recently adjusted its workload estimating model to better reflect how long it takes L&C staff to perform certain functions and capture incomplete workload from prior years.
Recent Issues Have Gained Attention. Recent incidents of inconsistent and inadequate oversight, monitoring, and enforcement of L&C standards for health facilities have gained the attention of the media and the Legislature. In 2014, several issues came to light regarding the Los Angeles County Health Facilities Inspection Division. An investigative reporter uncovered evidence that Los Angeles County had an unofficial policy to close certain complaints about long–term care facilities without properly investigating them. The County of Los Angeles Department of Auditor–Controller issued the results of its investigation of the Health Facilities Inspection Division’s performance, concluding that the division had a significant workload backlog and lacked a mechanism to effectively track and manage its workload. In a separate report, DPH found Los Angeles County has significant problems with how to correctly prioritize complaints, which has resulted in delayed investigations of serious allegations.
In response to the problems regarding L&C in Los Angeles County and statewide, the Legislature enacted Chapter 31, Statutes of 2014 (SB 857, Committee on Budget), that included several requirements intended to facilitate legislative oversight of L&C including: (1) quarterly reporting on the status of long–term care facility complaints, investigations, state relicensing and federal recertification surveys, and vacancy rates within L&C; (2) by December 1, 2014, DPH will provide a report assessing the possibilities of using professional position classifications other than HFENs to perform licensing and certification survey or complaint workload; and (3) DPH will hold semiannual meetings for all interested stakeholders to provide feedback on improving the L&C Program.
In October 2014, the California State Auditor released a report that found DPH has not effectively managed investigations of complaints related to long–term health care facilities. One of the State Auditor’s key findings was that as of April 2014, DPH had more than 11,000 open complaints and ERIs—many of which had remained open for an average of nearly a year. The State Auditor made recommendations to DPH to take several actions to protect the health, safety, and well–being of residents in long–term health care facilities including: (1) implementing a formal monitoring process of open complaints and improving the accuracy of tracking their status; (2) establishing time frames for completing facility–related complaint investigations and developing formal policies for timely processing of complaints against individuals; (3) providing district offices with guidance for the consistent and efficient processing of ERIs; and (4) ensuring that district offices have the necessary resources to process complaints promptly. The DPH agreed with many of the State Auditor’s recommendations and stated that it will take steps to implement them.
In response to recent issues of inconsistent and inadequate oversight, monitoring, and enforcement of L&C standards, the Governor’s budget includes two quality improvement proposals: one targeted at improving the efficiency and effectiveness of Los Angeles County’s contract L&C activities and the other targeted at improving L&C Program quality statewide. The Governor’s budget also includes two workload–related proposals: one would provide additional L&C positions to DPH to address workload backlogs; the other would provide additional contract funding to Los Angeles County to pay for additional Health Facilities Inspection Division positions and cover increases in negotiated salary rates. Figure 15 summarizes the Governor’s proposals.
Figure 15
Summary of Governor’s Licensing and Certification Program Proposals
(Dollars in Millions)
|
|
State Positions
|
Funds
|
Fund Source
|
|
Quality Improvement Proposals
|
|
|
|
|
Los Angeles County contract monitoring and quality improvement
|
3
|
$0.4
|
Public Health Licensing and Certification Fund
|
|
Licensing and Certification Program quality improvement projects
|
—
|
2.0
|
Internal Department Quality Improvement Account
|
|
Workload–Related Proposals
|
|
|
|
|
Los Angeles County contract increased funding
|
—a
|
9.5
|
Public Health Licensing and Certification Fund
|
|
Licensing and Certification Program state workload
|
237
|
19.8
|
Public Health Licensing and Certification Fund
|
|
Totals
|
240
|
$31.7
|
|
In the next section of this analysis, we describe each of the Governor’s four proposals separately and provide our analysis and recommendations in conjunction with each proposal. We start with the two proposals addressing quality improvement and then move on to the two proposals regarding salary and staffing. Overall, we find that the Governor’s proposals contain elements that would address the recent quality–related issues and shortcomings identified both in Los Angeles County and at the state level. However, we raise concerns regarding the Governor’s proposals to increase L&C staffing both in Los Angeles County and DPH.
Background. On April 21, 2014, CMS notified DPH that it would withhold $503,000 of DPH’s federal funding allocation until DPH achieves certain benchmarks related to its management of its contract with Los Angeles County to perform L&C activities, including installing a temporary management monitoring team to assist in and oversee the implementation of programmatic and administrative improvements. (Ultimately the CMS withheld $251,000 in federal funds.) To address CMS issues, DPH requests resources for an ongoing, on–site management monitoring team to ensure Los Angeles County improves the quality of its L&C Program. According to DPH, Los Angeles County has formed a new management team to improve its Health Facilities Inspection Division operations, but the new division management staff lack experience in the program and need assistance from staff with knowledge and experience performing and managing L&C workload.
Governor’s Proposal. The budget plan proposes $378,000 in special funds to permanently establish three state positions (these positions have already been administratively established) to perform quality improvement activities to improve Los Angeles County Health Facilities Inspection Division operations as follows.
- Conduct on–site monitoring of Los Angeles County operations in the Health Facilities Inspection Division district offices to improve the division’s efficiency and effectiveness.
- Help staff prioritize workload, implement work plans and tracking logs and identify best practices.
- Conduct on–site training and quality reviews of Los Angeles County surveys and investigations.
LAO Assessment. We find that the Governor’s proposal to improve oversight and monitoring of the Los Angeles County L&C contract has merit. Since the Governor’s request would address quality issues that have been identified by CMS and DPH, it makes sense that the state would act to improve its oversight in this area. In addition to this proposal, we believe there are other options for the state to improve its monitoring of the Los Angeles County L&C contract. We discuss these other options in more detail in our analysis of the Governor’s proposal to increase funding for the Los Angeles County L&C contract later in this analysis.
LAO Recommendation. We recommend approval of the Governor’s proposal to establish 3 positions to perform quality improvement activities to improve Los Angeles County Health Facilities Inspection Division operations and address issues identified by CMS. Such action is necessary to mitigate the risk of further loss of federal funding that supports L&C activities.
Background. In a June 2012 letter, CMS directed DPH to conduct a comprehensive assessment of DPH’s entire survey and certification operations at its headquarters and also at each of the DPH’s district offices and the offices covered by its contract with Los Angeles County. The assessment was to identify concerns, issues, and barriers related to DPH’s difficulty in meeting CMS performance expectations. In response to the CMS letter, DPH contracted for and received an “Initial Assessment and Gap Analysis Report and Remediation Recommendations” report in August 2014. The report contains 21 recommendations to allow for meaningful, measurable improvements in the L&C Program.
Governor’s Proposal. The budget plan proposes $2 million in special funds to implement quality improvement projects recommended in the consultant’s report. According to DPH, many of the quality improvement initiatives recommended in the report will require knowledge, skills, expertise, or capacity that DPH lacks internally. Accordingly, DPH seeks assistance implementing several recommendations made in the consultant’s report including the following examples.
- Standardizing data entry processes and identifying and resolving data quality issues.
- Creating measures to assess performance and provide transparency to internal and external stakeholders.
- Engaging an expert to develop and implement a nurse recruitment strategy, retention strategies to retain qualified and trained staff, and mentoring programs.
LAO Assessment. Many of the recommendations in the consultant’s report have a direct bearing on L&Cs ability to ensure the health and safety of persons in long–term care facilities. Given the need to address the issues identified in the consultant’s report in a timely manner, we believe it makes sense to bring in outside consultants to fill the gaps where DPH does not have sufficient internal expertise.
LAO Recommendation. We recommend approval of this component of the Governor’s proposal. Given the urgent need to address identified quality issues in the L&C Program in order to ensure health and safety of persons in long–term care facilities, we believe adding additional resources in the short term is a sensible approach.
Background. For the past 30 years, CDPH has contracted with Los Angeles County to perform L&C surveys and investigate complaints and ERIs in Los Angeles County. According to DPH, Los Angeles County accounts for 33 percent of licensed and certified health care facilities in California.
In July 2012, DPH and Los Angeles County renewed the contract for a three–year term ending June 30, 2015, with an annual budget of $26.9 million to fund a total of 178 positions. However, according to DPH, due to a salary increase negotiated by Los Angeles County nurses after the contract went into effect, the current budget is sufficient to fund only 151 of the 178 positions and Los Angeles County has held 27 positions vacant in order to stay within its annual budget. In addition, Los Angeles County has experienced difficulties due to attrition, recruitment problems, and delays in hiring and training.
Governor’s Proposal. The budget plan proposes an increase of $9.5 million in special funds to augment the Los Angeles County contract to perform L&C activities in Los Angeles County. Specifically, the proposal would (1) provide $2.6 million to fully fund the salaries for the existing 178 contract positions at current Los Angeles County salary rates, and (2) provide $6.9 million to fund 32 additional positions. This would bring the total Los Angeles County L&C positions to 210.
According to DPH, Los Angeles County would need a total of $43.1 million and 281 positions to complete state licensing and federal certification activities, and investigate aging complaints and ERIs. Of the 281 positions, 23 would be required for clearing open and aged complaints over a four–year period and the remaining 258 positions would complete ongoing mandated workload. Thus, this component of the Governor’s budget proposal would focus on only a portion of the pending workload, allowing Los Angeles County to meet timeliness requirements for the highest priority workload based on CMS guidelines. In discussions with DPH, the department indicates that once Los Angeles County has filled and trained staff for the 32 additional positions funded under this proposal, DPH may request additional resources for Los Angeles County in order to address the county’s ongoing workload backlog.
LAO Analysis. Based upon our analysis of average cost per position in the Los Angeles County Health Facilities Inspection Division, and assuming current staffing ratios, we believe the proposed funding level appropriately accounts for an increase in HFEN salaries and adds 32 positions. However, we note that under Chapter 31, DPH was required to provide a report by December 1, 2014, assessing the possibilities of using professional position classifications other than HFENs to perform L&C survey or complaint workload. At the time this analysis was prepared, the administration had not released the required report. Depending on the results of the report, it may be feasible to have licensed social workers, licensed vocational nurses, or other position classifications perform workload currently performed by HFENs. To the extent these other position classifications are paid lower salaries than HFENs, it would result in lower overall costs to perform the same workload. In the absence of the pending report, we are not in a position to assess whether the Governor’s proposal is the most cost–effective approach to addressing the workload backlog in Los Angeles County (or in the DPH L&C Program as we discuss in the next section of this analysis).
Chapter 31 requires reporting of key L&C measures. In February of 2015, DPH released its second report containing this information for the second quarter of the 2014–15 fiscal year. For example, for SNFs, ICF–DD, congregate living health facilities, and pediatric day health and respite care facilities, the report provided information on: (1) complaints received during the reporting period, (2) complaints completed during the reporting period (regardless of receipt date), (3) the growth or decrease in open complaints by reporting period, and (4) the number of open complaints pending broken out by the reporting period in which they were received. The report also provided significant additional information that is not described here. In this most recent report, the data were reported at a statewide level. However, based upon discussions with DPH, beginning with the report for the third quarter of 2014–15 (due to be released in April 2015), data will be broken out by region, including data on Los Angeles County. This data will allow for better legislative oversight of Los Angeles County to determine whether the county is improving its performance.
The existing three–year Los Angeles County contract is up for renewal July 2015. According to DPH, the existing contract contains broad language that failure to perform workload could result in a withhold of payments. In our view, it makes sense to include clearly specified performance goals in the contract and clearly specified actions, such as withholds of payment, if those performance goals are not attained. Furthermore, given Los Angeles County’s recent performance, we believe it makes sense to renew the contract on a one–year basis. This would allow for an annual review process and give DPH the ability to adjust the performance goals annually until Los Angeles County has fully addressed the outstanding performance issues.
LAO Recommendation. We withhold recommendation on approval of the Governor’s request for $9.5 million to augment the contract with Los Angeles County to fund 32 new positions in 2015–16 and fully fund existing HFEN positions at current Los Angeles County salary levels. At the time this analysis was prepared, the administration had not released a report required under Chapter 31 to assess the possibilities of using professional position classifications other than HFENs to perform licensing and certification survey or complaint work. In the absence of this report, we are unable to fully evaluate whether the administration’s proposal is the most cost–effective approach to addressing L&C workload issues. We recommend that the Legislature encourage the administration to submit this report as soon as possible so that it can be considered in the budget process.
We also recommend the Legislature require the department to incorporate meaningful performance measures and benchmarks into the Los Angeles County contract and impose withholds of funding if the county fails to achieve these measures. We further recommend that the contract, up for renewal in July 2015, be renewed for a one–year period in order to allow for annual adjustments to the performance measures and benchmarks. We believe this approach to structuring the Los Angeles County contract will improve the county’s accountability to the state and incentivize improvements in quality, efficiency and effectiveness.
Background. Based on recent changes to its workload estimating model, the November 2014 estimate indicates the DPH L&C Program requires additional funding authority and staff to complete mandated workload, including completing complaint and ERI investigations that remain open from prior years. The DPH indicates that it is still reviewing and refining its workload estimating model. In particular, the L&C Program is continuing to refine its timekeeping system to improve the program’s ability to accurately capture and assess the surveyor time and staff needed to complete various types of state and federal licensing and certification activities.
Governor’s Proposal. The budget plan proposes an increase of $19.8 million in special funds in 2015–16 ($30.4 million in 2016–17) for 173 permanent positions and 64 two–year, limited–term positions, for a total of 237 positions (123 positions would become effective July 1, 2015, and 114 positions would become effective on April 1, 2016). The DPH estimates that with the additional 237 positions requested, program staff could complete the current pending investigation workload in approximately four years, while also addressing new workload and avoiding any new cases from aging. Of the 237 proposed positions, 144 are for HFENs (42 two–year, limited–term positions and 102 permanent positions).
LAO Analysis. In the previous section of this analysis, we noted the administration had not released an overdue report required under Chapter 31 to assess the possibilities of using professional position classifications other than HFENs to perform L&C survey or complaint work. Because this proposal would establish an additional 144 HFEN positions, this report is critically important to informing an analysis of the proposal. Although information in the overdue report might provide information that would cause us to recommend a reduction in the number of HFEN positions that the Legislature should authorize, it is likely that at least some HFEN positions would still warrant approval. For this reason, we provide some additional information regarding HFEN training for the Legislature to take into account as it weighs the Governor’s proposal.
A new HFEN spends the first four to six months completing prerequisite state training courses and participating in surveys and complaint investigations. General training times are approximately as follows:
- 4 to 9 months prior to working independently on state complaints.
- 4 to 12 months prior to working independently on state licensing surveys.
- 12 to 16 months prior to working independently on federal complaint investigations and to work on federal certification surveys.
Generally, newly hired HFENs must work as part of a team while undergoing training. Furthermore, HFENs must complete state and federal courses and pass CMS’s Surveyor Minimum Qualification Test before the HFEN may work independently on surveys and complaint investigations. Given the amount of time it takes to train a newly hired HFEN before he/she is able to work at full capacity, we think it makes sense to explore other options to complete this workload using other position classifications. Furthermore, we question whether it makes sense to establish two–year, limited–term positions in a position classification where it takes as much as nine months before a new hire can work independently in some areas of L&C.
LAO Recommendation. We withhold recommendation on approval of the request for $19.8 million and 273 positions in 2015–16. At the time this analysis was prepared, the administration had not released a report required under Chapter 31 to assess the possibilities of using professional position classifications other than HFENs to perform L&C survey or complaint work. In the absence of this report, we are unable to fully evaluate whether the administration’s proposal is the most cost–effective approach to addressing L&C workload issues at the state level.
Governor’s Approach of Adding More Resources Makes Sense. . . We believe it makes sense to add significant additional resources to the L&C Program in order to address the backlog of L&C workload and complaint investigations. Even with these additional resources, it will likely take several years before the L&C workload backlog is cleared.
. . .However, Outstanding Report Is Key to Making Informed Decisions. In the absence of a key report, the Legislature is not in a position to determine whether the additional funding for Los Angeles County to address L&C staffing issues and the proposed increase in staffing for state L&C functions is the most cost–effective approach to addressing workload backlog issues.
LAO Publications: To request publications call (916) 445-4656. This report and others, as well as an E-mail subscription service, are available on the LAO's Internet site at www.lao.ca.gov. The LAO is located at 925 L Street, Suite 1000, Sacramento, CA 95814.
Return to LAO Home Page