California’s major human services programs provide a variety of benefits to its citizens. These include income maintenance for the aged, blind, or disabled; cash assistance and welfare–to–work services for low–income families with children; protecting children from abuse and neglect; providing home care workers who assist the aged and disabled in remaining in their own homes; collection of child support from noncustodial parents; and subsidized child care for low–income families.
Human services are administered at the state level by DSS, Department of Developmental Services (DDS), Department of Child Support Services, and other California Health and Human Services Agency (CHHSA) departments. The actual delivery of many services takes place at the local level and is carried out by 58 separate county welfare departments. The major exception is Supplemental Security Income/State Supplementary Payment (SSI/SSP), which is administered mainly by the U.S. Social Services Administration.
Recent Major Changes in Funding for Human Services Programs. As a result of realignment–related legislation in 2011 and 2013, the budget reflects shifts to counties of a significant amount of General Fund costs in human services programs. Specifically, as a result of 2011 legislation, the budget (beginning in 2011–12) reflects shifts to local realignment revenues of about $1.1 billion of General Fund costs in the CalWORKs program and about $1.6 billion in child welfare and adult protective services General Fund costs. As a result of the latter shift, the state’s role with respect to child welfare and adult protective services is largely one of oversight of county administration of these program areas.
Legislation enacted in 2013 shifted additional General Fund costs in the CalWORKs program to local realignment revenues that previously have been used to provide health services to indigent individuals. These realignment revenues have been freed up given that many indigent individuals are newly eligible for coverage in the state–funded Medi–Cal Program. Specifically, the budget shifts $300 million in CalWORKs General Fund costs to these local realignment revenues in 2013–14 and an additional $600 million (for a total of $900 million) in 2014–15. The 2013 legislation additionally provided that the costs of specified ongoing increases to CalWORKs assistance payments will be shifted to revenues from the growth of existing local realignment revenues that otherwise would have supported other social services programs. These recent changes to realignment are discussed in greater detail below in the “CalWORKs” section of this report.
Overview of Human Services Budget Proposal. The Governor’s budget proposes expenditures of about $9.9 billion from the General Fund for human services programs in 2014–15. As shown in Figure 1, this reflects a decrease of $132 million—or 2.5 percent—from revised General Fund expenditures in 2013–14.
Figure 1
Major Human Services Programs and Departments—Budget Summary
General Fund (Dollars in Millions)
|
|
2012–13 Actual
|
2013–14 Estimated
|
2014–15 Proposed
|
Change From 2013–14 to 2014–15
|
|
Amount
|
Percent
|
|
SSI/SSP
|
$2,752.6
|
$2,782.3
|
$2,816.5
|
$34.2
|
1.2%
|
|
Department of Developmental Services
|
2,674.5
|
2,803.1
|
2,934.7
|
131.6
|
4.7
|
|
CalWORKs
|
1,544.5
|
1,206.2a
|
636.9b
|
–569.3
|
–47.2
|
|
In–Home Supportive Services
|
1,705.9
|
1,910.0
|
1,994.1
|
84.1
|
4.4
|
|
County Administration and Automation
|
617.0
|
763.2
|
798.7
|
35.5
|
4.6
|
|
Department of Child Support Services
|
298.9
|
313.0
|
312.9
|
–0.1
|
—
|
|
Department of Rehabilitation
|
55.3
|
57.0
|
57.0
|
—
|
0.1
|
|
Department of Aging
|
31.4
|
32.2
|
32.2
|
—
|
—
|
|
All other social services (including state support)
|
239.3
|
261.7
|
294.7
|
33.0
|
12.6
|
|
Totals
|
$9,919.3
|
$10,128.7
|
$9,877.7
|
–$251.0
|
–2.5%
|
Summary of Major Budget Proposals and Changes. As shown in Figure 1, the budget reflects generally stable or modest growth in General Fund expenditures across most human services programs, with CalWORKs being the major exception. The 47 percent decrease ($569 million) in CalWORKs General Fund expenditures can largely be explained by a year–over–year increase of $600 million in 1991 health realignment revenues that are being redirected to help pay for CalWORKs grant costs, thereby reducing General Fund expenditures by a like amount. The CalWORKs budget also reflects a 5 percent increase in cash grant levels costing $168 million, although this is funded almost entirely from realignment revenues (with $6 million General Fund). The CalWORKs budget also reflects a net increase of $91 million from the General Fund to implement a number of recent policy changes—that result in costs and savings—related to early engagement, family stabilization, and subsidized employment. Finally, the budget proposes a six–county, three–year Parent/Child Engagement Demonstration Pilot in CalWORKs, at a three–year cost totaling $115 million General Fund ($9.9 million in 2014–15). We discuss the grant increase, implementation of recent policy reforms, and the proposed pilot program in detail later.
The 4.4 percent growth ($84 million) in IHSS General Fund expenditures mainly reflects the partial–year cost ($99 million General Fund in 2014–15) of the Governor’s policy proposal to comply with new federal labor regulations. These regulations require, among other things, that IHSS providers be paid overtime for work over 40 hours a week. We provide an analysis of this proposal later.
The 4.6 percent increase ($36 million) in General Fund expenditures in the County Administration and Automation budget line item largely reflects a $30 million increase for CalFresh administration (due to the caseload impact of outreach conducted with the implementation of the federal Patient Protection and Affordable Care Act [ACA]) and a $12 million increase for two human services automation projects.
Varied Growth Through Recession. While caseload grew for most of the state’s human services programs during the recent recession, there was substantial variability among them. (One key exception is the state’s foster care caseload, which has declined since 2001 and through the recession. In part, this reflects the creation of the Kinship Guardian Assistance Payment program in 2000 that facilitates a permanent placement option for relative foster children outside of the foster care system.) For example, over the 2007–08 to 2011–12 period, the CalFresh and CalWORKs caseloads increased by 97 percent and 27 percent, respectively, while the IHSS caseload—less susceptible to economic fluctuations—increased by 8 percent. The SSI/SSP caseload grew modestly during this time period (3.4 percent)—in part reflecting recent grant reductions that in effect reduced the eligible population—and is projected to grow relatively modestly in 2014–15.
We now turn more specifically to caseload trends in the IHSS and CalWORKs programs and the budget’s assumptions regarding caseload for these two programs in 2014–15.
IHSS Caseload Projected to Grow Modestly in 2014–15. The budget projects the average monthly caseload for IHSS to be 453,417 in 2014–15—a 1.3 percent increase over the most recent estimate of the 2013–14 caseload. We discuss the administration’s projection in further detail below in the “IHSS” section of this report. For historical perspective, the IHSS caseload has remained relatively flat throughout the five–year period from 2009–10 through 2013–14, in part reflecting policy changes that constrained caseload growth.
CalWORKs Caseload Continues to Decline. In the midst of the recent recession, the CalWORKs caseload rose substantially and peaked at over 597,000 cases in June 2011. The caseload has been declining since that time due to enacted policy changes and an improving labor market. The budget assumes a CalWORKs caseload of 545,647 cases in 2013–14, a 2.5 percent decline from the previous year. The year–over–year decline in caseload is assumed to accelerate somewhat to 3 percent in 2014–15, resulting in a caseload of 529,376.
The federal Department of Labor recently released new regulations that affect home care workers. A home care worker can be any individual who provides home care services, including certified nursing assistants, home health aides, or personal care aides such as providers for California’s IHSS program. Personal care refers to assistance with activities of daily living—such as bathing, grooming, and bowel and bladder care—provided to a consumer by a home care worker. The new federal labor regulations—effective January 1, 2015—make two significant changes, discussed below, that affect the home care industry. These new federal labor regulations have budgetary implications for both the state’s IHSS program and DDS. In this analysis, we describe the federal labor regulations, explain how these regulations impact IHSS and DDS, describe the Governor’s proposals to comply with the regulations, and provide modifications to the Governor’s IHSS proposal for consideration by the Legislature.
Federal Labor Regulations Require Home Care Workers to Be Paid for Certain Work Activities. The federal labor regulations require home care workers to be paid for certain work activities, effective January 1, 2015. Generally, employers have been exempt from the requirement to pay home care workers for the following work activities that will now require payment.
- Wait Time During Medical Appointments. Time spent waiting for consumers during medical appointments must be paid.
- Travel Time During the Work Day. Time spent traveling during the employee’s regular work hours, such as travel time to shop for food or perform other errands on behalf of the consumer, must be paid. For home care workers employed by a “third–party employer,” travel time between consumers during the workday must also be paid. (A third–party employer is an employer other than the consumer receiving services. In the case of the IHSS program, the state can be understood to be the third–party employer.)
- Mandatory Worker Training. Time spent attending training required by the employer must be paid.
Federal Labor Regulations Require Home Care Workers to Receive Overtime Pay for Working More Than 40 Hours Per Week. Employers of home care workers have been exempt from the requirement to pay overtime at the rate of one–and–a–half times the regular pay rate for all hours worked that exceed 40 in a week. However, effective January 1, 2015, federal labor regulations require home care workers to be paid overtime. Under federal law, the requirement to pay overtime may not be waived by agreement between the employer and employee. Further, an announcement or notice by the employer that no overtime work will be permitted will not infringe on the employee’s right to receive overtime pay for hours that exceed 40 in a workweek. In other words, the employer is required to pay overtime when it is claimed by an employee on his/her timesheet, regardless of whether the overtime is authorized or not.
Narrow Exemptions to Overtime Pay Requirement When Consumer, His/Her Family, or Household Is the Employer. When a worker is employed by a consumer receiving services or the consumer’s family or household, the federal labor regulations provide for narrow exemptions to the requirement to pay overtime. One of these exemptions—known as the “live–in domestic service worker exemption” is available when a worker is employed by—and resides with—the consumer receiving services or the consumer’s family or household. In these cases, the consumer, his/her family, or household may claim the live–in domestic service worker exemption to avoid paying the worker overtime for hours that exceed 40 in a workweek (and would instead pay at least the state–mandated hourly minimum wage for all hours worked). However, this exemption is not available to a third–party employer, such as the state in the existing program model of IHSS. (It may be possible for an IHSS recipient to claim this exemption under a different program model for the delivery of IHSS–like services, which we discuss later in this report.)
The federal labor regulations we describe have significant implications for the state’s IHSS program. Effective January 1, 2015, IHSS providers that deliver personal care and domestic services to IHSS recipients will be compensated for certain work activities, including wait time during medical appointments and travel time during the work day, which are currently not compensated by the IHSS program. Additionally, IHSS providers will be eligible to receive overtime pay for hours worked that exceed 40 in a workweek. Below, we provide background information about the IHSS program that is relevant to understanding the implications of the federal labor regulations.
The IHSS Program Is a Medi–Cal Benefit That Provides Personal Care and Domestic Services. The IHSS recipients are eligible to receive up to 283 hours per month of assistance with tasks such as bathing, dressing, housework, and meal preparation that are delivered by an IHSS provider in the recipient’s home. The recipient has the right to determine when service hours are provided within the month. For nearly all recipients, the IHSS program is delivered as a benefit of the state’s Medicaid health services program (known as Medi–Cal in California) for low–income populations. The IHSS program is therefore subject to federal Medicaid rules. For more background on IHSS, please refer to the “In–Home Supportive Services” section of this report.
Division of Employer Responsibilities in the IHSS Program. Employer responsibilities in the IHSS program are divided among three entities.
- Recipient. The recipient has the right to hire, supervise, and train the IHSS provider and can fire the provider for any reason. Essentially, the recipient has the right to receive care from a provider of his/her choosing—a concept we refer to as “consumer choice.”
- State. The IHSS providers submit their timesheets to a state processing facility and receive payment from the state for the hours they work during each pay period. The state is responsible for paying for certain benefits, including state disability insurance, unemployment insurance, and workers’ compensation insurance.
- Public Authority. The Public Authority at the county level currently negotiates with unions representing IHSS providers to set wages and benefits. The Public Authority also maintains a registry of providers who may be available to work for IHSS recipients who are unable to identify their own provider. (We note that recent legislation provides for the future transfer of collective bargaining responsibilities from the county level to the state level in certain counties.)
Because of this division of IHSS employment responsibilities, it is our understanding that the IHSS recipient, the state, and the Public Authority at the county level are all considered to be joint employers of IHSS providers for the purposes of the new federal labor regulations. The state and the Public Authority are third–party employers because they are entities other than the consumer receiving services. However, because of the financial structure of the IHSS program in which county costs are effectively capped given recently enacted maintenance–of–effort (MOE) requirements, the state would assume all of the nonfederal costs associated with newly paying for overtime and for the work activities newly required to be compensated.
Individuals Must Follow Four Steps Before Being Enrolled as IHSS Providers. Currently, prospective IHSS providers must complete four steps in order to be enrolled as a provider and receive payment from the state, including completion of an application, a criminal background check, a brief IHSS program provider orientation, and completion of an enrollment agreement.
IHSS Providers Receive Wages Negotiated at the County Level. Because the wages of IHSS providers are negotiated at the county level, they vary by county—currently ranging from the state–mandated hourly minimum wage of $8 to $12.20 per hour. Providers currently receive the negotiated wage for all hours worked, regardless of whether they work in excess of 40 hours in a week. Chapter 351, Statutes of 2013 (AB 10, Alejo), increases the state–mandated hourly minimum wage from $8 to $9 effective July 1, 2014—and to $10 effective January 1, 2016. In 2014–15, the minimum wage increase to $9 will affect IHSS providers in 17 counties, where wages are currently less than $9 per hour.
IHSS Providers and Recipients Impacted by Federal Labor Regulations. The DSS, which administers the IHSS program, estimates that 385,425 individuals will work as IHSS providers in 2014–15. About 49,000 providers, or 12.7 percent of the estimated workforce, currently work more than 160 hours per month and will therefore be impacted by the requirement to pay overtime for hours that exceed 40 in a workweek. We note that some providers work for more than one recipient.
The DSS estimates that 453,417 low–income individuals who are aged, blind, or disabled will receive IHSS in 2014–15. About 37,000 recipients, or 8.2 percent of the estimated caseload in 2014–15, are expected to receive more than 160 service hours per month from a single IHSS provider. The IHSS recipients who receive more than 160 service hours per month are generally individuals who are reliant on the IHSS program for significant assistance with activities of daily living.
IHSS Providers Are Often Family Members or Relatives of Recipients. About 70 percent of IHSS recipients (an estimated 317,000 recipients) receive their care from a family member or relative provider. About half of IHSS recipients (an estimated 222,000 recipients) receive their care from a live–in provider, and 84 percent of these live–in providers are family members of the recipient. These family members could be, for example, a parent providing services to a minor child, a spouse providing services to a husband or wife, or an adult child providing services to a parent.
Absent any changes to the IHSS program, the administration estimates the annualized cost to comply with the federal labor regulations to be $620 million ($288 million General Fund). There are three main components of this cost estimate.
- Overtime Costs. Based on the existing workload of IHSS providers statewide, the DSS estimates that the cost of paying overtime would be $402 million ($186 million General Fund) annually. This estimate likely understates the actual cost of paying overtime as some IHSS providers would choose to work additional hours for other recipients in order to receive overtime pay for hours exceeding 40 in a workweek.
- Costs of Newly Compensable Work Activities. The DSS estimates that the cost of paying IHSS providers for wait time during medical appointments and travel time during the work day is $192 million ($89 million General Fund) annually.
- Administrative Activities. The DSS estimates that the cost of administrative activities to implement the new payments is $26 million ($13 million General Fund) annually. These costs would fund such administrative activities as county social worker time to answer questions from IHSS recipients and providers, making provider timesheet changes, and modifying the Case Management, Information, and Payrolling System (CMIPS) II information technology (IT) system used by the IHSS program—in order to handle authorization and payment for the newly compensable work activities and overtime.
The federal labor regulations we describe also have a budgetary impact on the state’s Community Services Program for eligible individuals with developmental disabilities that is administered by DDS. The budgetary impact for the Community Services Program is relatively minor when compared to the impact on the IHSS program. For more background on the Community Services Program, please refer to the “Developmental Services” section of this report.
Community Services Program Provides In–Home Assistance, Among Other Services and Supports. The Community Services Program provides eligible individuals with developmental disabilities with a broad range of services and supports they need to live in the community. The DDS oversees 21 nonprofit organizations known as regional centers (RCs), which purchase services and supports from vendors (generally organizations that hire employees to deliver services) for consumers. In some cases, consumers receive IHSS as a Medi–Cal benefit and receive other in–home services paid for by RCs, either on an ongoing basis or temporarily to provide respite to the primary caregiver.
Consumers and Workers Affected by Federal Labor Regulations. Due to current data limitations, the number of consumers who receive in–home assistance that exceeds 40 hours per week—and the number of workers who provide in–home assistance that exceeds 40 hours per week—is not known by DDS. These consumers who receive more than 40 hours of in–home assistance per week and home care workers who provide this assistance will be affected by the federal labor regulations.
The Governor’s budget responds to the federal labor regulations by (1) funding the cost associated with newly compensable work activities, (2) limiting the cost of overtime in the IHSS program by restricting IHSS providers to no more than 40 hours of work per week, and (3) providing a small rate increase to certain RC vendors in order for vendors to mitigate the fiscal impact of the requirement to pay overtime to their employees. At the time of this analysis, the administration had not yet released budget–related legislation providing further detail on its overtime proposals for IHSS and DDS. We provide details of the Governor’s proposals that were made available to us at the time of this analysis.
The administration estimates the annual ongoing cost of funding the three main components of its IHSS proposal—(1) paying for newly compensable work activities, (2) funding administrative activities to prevent overtime, and (3) maintaining a “Provider Backup System”—is $239 million ($113 million General Fund) annually. In Figure 2, we provide a cost summary of the Governor’s proposal to respond to the federal labor regulations in 2014–15 and 2015–16. (We note that Figure 2 includes the estimated costs of the Governor’s IHSS proposal as corrected by the administration for a technical budgeting error.) We discuss each component of the Governor’s IHSS proposal below.
Figure 2
Cost of Governor’s IHSS Proposal to Respond to Federal Labor Regulations
(In Millions)a
|
|
2014–15
|
|
2015–16
|
|
General Fund
|
Total Funds
|
General Fund
|
Total Funds
|
|
Newly compensable work activities
|
$40
|
$87
|
|
$88
|
$188
|
|
Administration to restrict overtime
|
27
|
53
|
|
10
|
19
|
|
Provider Backup System (including higher wage for backup providers and related costs)b
|
10
|
21
|
|
15
|
32
|
|
Totals
|
$77
|
$161
|
|
$113
|
$239
|
Pay for Newly Compensable Work Activities. The Governor’s budget proposes $87 million ($40 million General Fund) in 2014–15 to comply with the federal labor regulations that require the state to compensate IHSS providers for certain previously exempted work activities beginning January 1, 2015, or, for six months of 2014–15. The department estimates that the full–year cost is $188 million ($88 million General Fund) in 2015–16. The Governor’s budget funds compensation for wait time during medical appointments and travel time during the work day, but not the mandatory provider orientation, as explained below.
- Providers’ Wait Time During IHSS Recipients’ Medical Appointments. The current in–home IHSS assessment conducted by a county social worker assesses a consumer for the amount of time needed to travel to medical appointments, but makes no assessment for the amount of wait time that may be involved. The Governor’s budget assumes that the 85 percent of IHSS recipients who receive medical accompaniment will have their provider wait three hours per month—on average—during appointments. Based on these assumptions, the six–month cost of this work activity is estimated to be $81 million ($37 million General Fund) in 2014–15. However, because the exact amount of time that providers wait at medical appointments is unknown, the actual cost of paying IHSS providers for wait time during recipients’ medical appointments is uncertain.
- Providers’ Travel Time Between IHSS Recipients. The Governor’s budget estimates that 19 percent of IHSS providers serve multiple recipients. It is assumed that these providers who work for multiple recipients will spend one hour per month—on average—traveling between recipients. Based on these assumptions, the six–month cost of this work activity is estimated to be $6 million ($3 million General Fund). Like wait time during medical appointments, there is currently no data collected by the IHSS program on the exact amount of time IHSS providers spend traveling between IHSS recipients during the work day. Therefore, the cost of paying IHSS providers for travel time is uncertain.
- Mandatory Provider Orientation. While the federal labor regulations require IHSS providers to be paid for any mandatory training, the Governor’s budget does not request funding for the cost of paying individuals to attend the mandatory orientation prior to enrollment as an IHSS provider. The DSS has indicated to us that it assumes that the state may not need to pay individuals for participating in the mandatory orientation since it occurs before the individual enrolls as an IHSS provider. Based upon our review of the federal labor regulations, we find this assumption to be reasonable. However, because the mandatory orientation is brief (about one to two hours in most counties) and is only required to be completed once for individuals newly seeking to become IHSS providers, we do not estimate a significant General Fund cost if this activity is ultimately determined to require compensation.
Administrative Costs to Prohibit IHSS Providers From Working Overtime. The Governor’s budget proposes to respond to the federal labor regulations requiring overtime pay for home care workers by establishing an administrative structure that would prohibit IHSS providers from working overtime—at an estimated cost of $53 million ($27 million General Fund) in 2014–15. This restriction would generally require an IHSS recipient who receives more than 40 hours of care per week from a single provider to secure a second provider. To help IHSS providers set their schedules to avoid working overtime, the proposal requires all recipients and providers to complete “workweek agreements” to ensure no provider is scheduled to work more than 40 hours per week. These workweek agreements must be submitted to the county, reviewed by a county social worker, and entered by clerks into CMIPS II. The full–year cost of the administrative activities to restrict overtime is estimated to be $19 million ($10 million General Fund) in 2015–16. These administrative costs are estimated to decrease in 2015–16 primarily because the processing of workweek agreements by county social workers and clerks mostly occurs in the first year of implementation.
In addition to the workweek agreements, as a method to deter providers from working overtime, the proposal provides for suspending IHSS providers who claim more than 40 hours per week on their timesheet on at least two occasions. After the first instance of overtime claimed on a timesheet, the IHSS provider would receive a warning notice that he/she cannot claim more than 40 hours per week on his/her timesheet. After the second instance, the IHSS provider would be suspended from the program for a period of one year.
County social workers and clerks would conduct all administrative activities associated with the overtime restriction, including: (1) mass mailings about the overtime restriction and workweek agreement, (2) answering questions from IHSS providers and recipients about the overtime restriction, (3) reviewing the workweek agreements and entering the agreements into CMIPS II, (4) suspending and reenrolling certain IHSS providers, (5) adding IHSS providers to the Public Authority registry, and (6) coordinating services for the Provider Backup System, described below.
Provider Backup System for Unforeseen Circumstances. The Governor’s budget proposes $69 million ($32 million General Fund) in 2014–15 for the costs associated with establishing a Provider Backup System at the county level. (In Figure 2, we display the estimated costs of the Provider Backup System in 2014–15 and 2015–16 after correcting for a technical budgeting error, discussed below.) This system would supply a backup provider for an unforeseen circumstance in which an IHSS recipient is in need of immediate assistance but his/her regular provider has already worked 40 hours within the week, and other options, such as a second provider or the informal support of a family member or neighbor, are unavailable. In such circumstances, the consumer could call the system to request a backup provider who would be available in a short amount of time to provide assistance. Service hours delivered by a backup provider would be counted toward—and not in addition to—a recipient’s total allotment of monthly IHSS hours. The backup provider would receive a higher wage than the standard rate in the county to compensate him/her for the need to provide services on short notice.
The majority of the costs for the Provider Backup System funds a wage premium for backup providers above the county’s negotiated wage in order to compensate them for providing services on short notice. The estimate assumes that the cost of compensating the backup provider would be—on average—25 percent higher per hour than the estimated statewide average cost per hour of $12.33 in 2014–15. This translates into a wage premium of $3.08, and an average wage of $15.41 per hour for backup providers in 2014–15. (We note the exact amount of the wage premium for backup providers will be specified in forthcoming budget–related legislation.) The administration assumes that IHSS recipients with at least 60 monthly service hours will use the Provider Backup System. Accepting the administration’s assumptions regarding the utilization of the Provider Backup System and the incremental cost increase of about $3 per hour for provider backup services, we find the administration has overestimated the cost associated with paying for authorized service hours delivered by a backup provider by $22 million General Fund in 2014–15 (and by $48 million General Fund in 2015–16). This overestimation is due to a technical budgeting error, the administration acknowledges. In the nearby box, we provide an overview of two small–scale programs in San Francisco and Los Angeles Counties that have some similarities to the proposed Provider Backup System.
A number of Public Authorities at the county level have administered small–scale programs that have some similarities to the proposed Provider Backup System. The In–Home Supportive Services (IHSS) hours provided by these programs are counted toward—and not in addition to—a recipient’s total allotment of monthly service hours. Below, we provide an overview of the programs in San Francisco and Los Angeles Counties that recipients may use when their regular provider is unavailable.
San Francisco’s Public Authority Operates On–Call Program. Consumers in San Francisco who need an IHSS provider on short notice can get assistance from the On–Call Program operated by the Public Authority. The On–Call Program is intended for several unforeseen circumstances: (1) when a consumer suddenly needs a provider but has not yet hired one, (2) when a recipient’s regular provider is not available, and (3) when the consumer is being discharged from a hospital or nursing home without a regular provider in place. The On–Call Program phone line is available Monday through Friday from 8:30 a.m. to 5 p.m. with messages retrieved until 8 p.m. On weekends and holidays, an assigned counselor checks the On–Call line for messages five times throughout the day. The On–Call Program averages about 130 requests per month from consumers seeking assistance. The On–Call counselors dispatch a provider from a select group of providers who are willing to make themselves available on short notice and who receive a higher wage of $16 per hour plus a $5 transportation allowance (compared to the standard wage of $11.75 per hour in San Francisco with no transportation allowance).
Los Angeles’ Public Authority Operates Backup Attendant Program (BUAP). The BUAP began as a pilot program in 2007 with the intent of providing high–need IHSS recipients in Los Angeles County with a backup provider available on short notice for urgent, temporary needs. Today, IHSS recipients who receive 25 hours or more of personal care each month are eligible to access BUAP when their provider and usual substitute provider are not available. The BUAP phone line is available Monday through Friday 8 a.m. to 5 p.m. When a consumer calls, the BUAP operators use a computer database to identify a backup provider who can best meet the consumer’s needs. All backup providers are required to undergo training or a proficiency exam in the provision of paramedical services, such as administering medications, wound care, or tube feeding. Backup providers also receive a higher wage of $12 per hour (compared to the standard wage of $9.65 per hour in Los Angeles County). We note that BUAP is not heavily utilized. In 2013, only 142 IHSS recipients were enrolled in BUAP. The BUAP phone line received 254 calls and provided 1,342 backup service hours for the full year in 2013.
Apart from paying for backup provider wages, the estimated cost for the Provider Backup System in 2014–15 includes $4 million General Fund to make relevant changes to CMIPS II and $250,000 General Fund for paying overtime to some IHSS providers who may claim more than 40 hours per week, despite the overtime restriction, on no more than two occasions.
The Governor’s budget proposes $7.5 million ($4 million General Fund) in 2014–15 to respond to the new federal labor regulations for DDS. These costs would double in 2015–16 to $15 million ($8 million General Fund). This amount funds a 2.25 percent increase in the rates paid to certain RC vendors that provide in–home assistance to individuals with developmental disabilities. The rate increase intends to provide vendors with sufficient funding to mitigate the fiscal impact of the requirement to pay their employees overtime for hours that exceed 40 in a workweek. Vendors may mitigate this fiscal impact by, for example, hiring more employees to deliver in–home services. However, as we noted earlier, the DDS does not have data available on the number of consumers who currently receive in–home assistance that exceeds 40 hours per week nor does it maintain data on the number of workers who provide in–home assistance that exceeds 40 hours per week. While we find it reasonable to assume that vendors will incur increased administrative costs to minimize overtime pay, we are uncertain because of data limitations whether a rate increase in the amount of 2.25 percent is appropriate.
Analyst’s Recommendation. Although we find it reasonable that vendors would incur administrative costs to limit overtime, it is difficult to determine the actual cost to vendors in the absence of data. In order to assess whether a 2.25 percent rate increase for certain vendors is appropriate on an ongoing basis, we recommend DDS report to the Legislature—no later than May 1, 2016—on the results of the rate increase on impacted vendors. The DDS could potentially gather and report relevant information, such as the average number of new employees that were hired by vendors based on organizational size, the average administrative cost of hiring a new employee, and other methods used by vendors to mitigate the fiscal impact of overtime pay for employees who would otherwise work more than 40 hours in a week.
We find the Governor’s proposal to restrict overtime for IHSS providers to be worthy of consideration by the Legislature as a reasonable starting point for addressing the fiscal impact of the federal labor regulations on the IHSS program. The Governor’s proposal complies with the federal labor regulations in a manner that controls costs without reducing authorized service hours for IHSS recipients. Notwithstanding its merits, below we identify fiscal and policy issues that the Governor’s proposal raises. Later, we offer modifications to the Governor’s proposal that the Legislature may wish to consider to mitigate some of these policy concerns.
Below, we raise a number of policy issues with the Governor’s proposal to restrict IHSS providers from working more than 40 hours in a week. Some of these policy issues call into question whether the Governor’s proposal will work as intended to restrict overtime without causing recipients to forgo authorized service hours.
Some IHSS Recipients Will Experience an Erosion of Consumer Choice. As we note, the administration estimates that about 37,000 recipients who receive more than 160 service hours per month from a single provider will be impacted by the overtime restriction. About 49,000 providers currently work more than 160 hours per month and would experience a reduction in income because of the proposed overtime restriction. Under the Governor’s proposal, high–hour recipients would need to hire, supervise, and train an additional provider. Further, recipients who receive less than 160 service hours per month would need to ensure that their providers—who may work for multiple recipients—do not exceed 40 hours in any workweek. For some recipients who receive less than 160 service hours per month, this may involve switching to a provider who can fully accommodate their care without exceeding 40 hours in a workweek or hiring a second provider. The overtime restriction may prove to be an inconvenience for recipients who have an established plan of care with a single preferred provider. For consumers who receive care from a live–in provider, or from a family member or relative, the overtime restriction and potential need to hire a second provider may prove to be undesirable. Finally, for recipients with certain disabilities, such as a developmental disability, we understand anecdotally that some may experience challenges in adjusting to a new provider. The requirement that no single provider work more than 40 hours per week can be understood as an erosion of the existing consumer choice of some IHSS recipients who would no longer be able to receive all of their care from a single provider of their choice.
Uncertain Whether IHSS Providers Will Be Available to Fully Meet Predictable, Regular Care Needs. Because the Provider Backup System is only intended for unforeseen circumstances, an IHSS recipient who predictably and regularly needs more than 40 hours of assistance per week would need to retain at least two providers. It is uncertain if a sufficient number of IHSS providers would be available to meet this new demand for second providers—in some cases, for a small number of weekly hours. Depending on the labor market in a particular geographic area and a county’s negotiated wage—both of which change over time—along with a consumer’s needs and preferences, there may or may not be a sufficient pool of available providers.
We note that the following factors will likely assist consumers in identifying second providers: Public Authorities currently maintain registries of available IHSS providers (some providers on the registries may not be currently working at all), some existing IHSS providers who regularly work less than 40 hours per week may be willing to work additional hours for other recipients, and—in 17 counties where wages are currently set below $9 per hour—the increase in the state–mandated hourly minimum wage to $9 may encourage some individuals to work as IHSS providers. On the other hand, the Governor’s proposed one–year suspension of IHSS providers who claim overtime on two occasions, discussed further below, could somewhat reduce the pool of available providers.
Uncertain Whether the “Right” Backup Provider Will Be Available for Unforeseen Circumstances. For consumers who are in need of a backup provider to provide unforeseen assistance within a workweek, we find that a higher wage for backup providers is a reasonable way to work toward ensuring that a sufficient pool of backup providers is available from which to draw on short notice. However, even with a higher wage, it remains uncertain whether the Provider Backup System will be able to successfully pair all consumers with backup providers who meet consumers’ individualized needs in a manner that maintains their quality of care and preserves their preferences. The consumer may live in a geographically isolated area, may communicate in a language other than English, may have paramedical needs, or other specialized needs during the period in which the unforeseen assistance is required. The system would need to have a sufficient pool of backup providers as well as an effective matching process in order to adequately meet consumers’ individualized needs and preserve consumers’ right to hire a provider of their choosing.
Governor’s Proposal to Restrict Overtime Generally Lacks Flexibility. By restricting all overtime that exceeds 40 hours in a workweek, the Governor’s proposal inherently lacks flexibility. This lack of flexibility could have some significant policy consequences.
- Could Impede Consumers’ Access to Care. In the case of predictable, regular care for high–hour recipients, we are concerned about situations in which a county faces a shortage of available providers and is therefore unable to provide a consumer with a list of possible second providers. Under this scenario, the county would not have the flexibility to authorize overtime for a recipient’s regular provider until a second provider can be identified, and a consumer may be forced to forgo authorized care that exceeds 40 hours in a week in the interim.
- Could Result in Inefficient Response to Some Unforeseen Circumstances. Although the cost per hour of a backup provider is less expensive than the cost per hour of overtime for a regular provider, there may be other factors to consider—such as convenience and a consumer’s preference—when the care needed is unforeseen and requires a provider to exceed 40 hours in a week, but is expected to be limited in duration to just a couple hours. For instance, a recipient could fall and require assistance from the provider to get up, or a doctor’s appointment may last longer than expected. Under the Governor’s proposal, there is no flexibility for a provider to claim overtime for these types of short, unforeseen care needs if he/she has reached—or is approaching—the 40–hour workweek limit. However, such a situation may be an inefficient use of the Provider Backup System, which includes not only the higher wage of the backup provider but associated administrative costs to coordinate services in a short time frame.
- Enforcement of Overtime Restriction Could Lead to Some Unnecessary Disruptions in Care. The Governor’s proposed one–year suspension of IHSS providers who claim overtime on two occasions—without any exceptions—raises concerns in that it may suspend some IHSS providers and unduly cause a disruption in care for individuals receiving care from these providers. For example, if a provider does not receive the warning notice—because of a change of address or for some other justifiable reason—and as a result, claims overtime on two occasions, the provider would be suspended for a period of one year and the recipient would lose his/her regular provider. The provider may also submit two timesheets simultaneously or in close succession—both claiming overtime—before he/she receives the warning notice. Short of appealing the suspension, the provider would have no recourse but to wait for the period of one year to elapse. In cases in which the provider has made an honest mistake, the one–year suspension may be unwarranted and the recipient would likely experience a disruption in care that may cause him/her to rely on the Provider Backup System or to forgo care while a new regular provider can be identified.
After correcting the technical budgeting error, the administration estimates that the Governor’s proposal to restrict overtime for all IHSS providers, including administrative activities to prevent overtime and maintenance of the Provider Backup System, would cost $51 million ($25 million General Fund) annually. This is significantly less than the estimated cost of paying for the overtime—$401 million ($186 million General Fund) annually. Both the cost of the Governor’s proposal and the estimated cost of paying the overtime are subject to some uncertainty. On the one hand, the cost of restricting overtime under the Governor’s proposal is somewhat uncertain because the ongoing administrative costs could be higher than assumed and the ongoing Provider Backup System costs could be higher if utilization exceeds the administration’s assumptions. On the other hand, the cost of paying for overtime would likely be higher than estimated by the administration since providers could change their behavior (such as by working additional hours for other recipients) in order to receive overtime pay.
Despite this uncertainty, the General Fund cost of restricting overtime as proposed by the Governor would still likely be significantly lower than the alternative—paying for overtime for all IHSS providers. We therefore find that on a purely fiscal basis, the Governor’s proposal makes sense. Even if the annual ongoing costs of restricting overtime were significantly higher, the state would still likely save more than $100 million General Fund annually by implementing the Governor’s overtime restriction instead of paying for overtime for IHSS providers. However, as we explained, there are programmatic implications associated with the Governor’s overtime restriction. Below, we suggest potential modifications to the proposal that the Legislature may wish to consider to mitigate, at least to some degree, these concerns.
Because of the policy issues we raise with the Governor’s proposal to restrict overtime, the Legislature may want to consider potential modifications to the Governor’s proposal. In evaluating these modifications, the Legislature would want to weigh any additional costs of implementing the modification against the benefit of mitigating a particular policy concern using the following criteria.
- Costs Incurred for Overtime. What is the annual General Fund cost of overtime associated with the modification? Generally, mitigating an undesirable policy consequence of the overtime restriction—such as requiring a new provider for a high–hour recipient who currently relies on a single live–in provider—would result in additional costs compared to what the Governor is proposing (through the payment of overtime at least for some circumstances). However, the Legislature may wish to incur this cost if the modification mitigates, at least to some degree, an undesirable policy consequence of the Governor’s overtime restriction.
- Consumer Choice. Does the modification preserve or infringe on the existing choice of a recipient to hire a single provider of his/her choosing? Does the modification create added inconvenience for the consumer? The modification should mitigate—at least to some extent for certain populations—the undesirable policy consequence of reduced consumer choice and added inconvenience under the Governor’s overtime restriction.
- Administrative Cost and Complexity. Is the modification administratively costly and complex to implement? The modification should not be overly burdensome to implement at the state and county levels.
- Need for Additional Providers. Would the modification require the recruitment of new IHSS providers? The modification should not require a significant number of additional providers.
Within the framework of the Governor’s proposal to restrict overtime, we find the Legislature has options to modify the proposal in a manner that addresses the policy concerns we raise. We assess each modification based on the criteria described above. We note that because IHSS is a Medi–Cal benefit, the implementation of some of these modifications would likely require approval from the federal Centers for Medicare and Medicaid Services (CMS) to ensure compliance with federal requirements.
The Legislature could consider a targeted exemption from the overtime restriction for the providers of certain IHSS recipients—recipients who would find themselves in particularly disruptive situations if the overtime restriction applied to their providers. For example, a targeted exemption could include providers of (1) individuals with developmental disabilities who may face particular challenges in adjusting to a new provider, (2) individuals in rural counties who may face difficulties in finding a suitable second provider, or (3) individuals with live–in family or relative providers who strongly prefer to receive all of their care from the family member or relative. Because of federal Medicaid rules, we note there is significant uncertainty as to whether this modification would receive CMS approval. In Figure 3, we assess this modification to the Governor’s overtime restriction based on the criteria discussed above.
Figure 3
A Targeted Exemption From the Overtime Restriction for IHSS Providers of Certain Recipients
|
Criteria
|
Assessment of Modification Relative to Governor’s Proposal
|
|
Costs incurred for overtime
|
Additional costs, with amount dependent upon the overtime exposure of exempted providers delivering services to the targeted recipient population.
|
|
Consumer choice
|
Enhances consumer choice for the targeted recipient population.
|
|
Administrative cost and complexity
|
Results in some additional administrative activities—and thus added costs and complexity—associated with authorizing and tracking overtime for exempted providers of the targeted recipient population.
|
|
Need for additional providers
|
Reduces number of additional providers that would need to be recruited, since the targeted recipient population would not need additional providers.
|
The Legislature could consider modifying the Governor’s proposal by authorizing a limited allotment of overtime hours—for example, 48 hours in a year—to IHSS providers who work for high–hour recipients in order to give these providers some flexibility to work hours exceeding 40 in a week for special circumstances, such as a recipient’s fall or a long doctor’s appointment, without facing disciplinary action. This option could give providers who may already be in a consumer’s home the opportunity to address an unforeseen issue that is limited in duration to just a couple hours and could potentially reduce the number of calls placed to the Provider Backup System. We assess this modification to the Governor’s overtime restriction—using the example of 48 hours of flexible overtime in a year—in Figure 4.
Figure 4
Provide a Limited Allotment of Overtime, Such as 48 Hours Annually, to Certain IHSS Providers
|
Criteria
|
Assessment of Modification Relative to Governor’s Proposal
|
|
Costs incurred for overtime
|
- Additional costs, with amount dependent upon the amount of the flexible overtime allotment and utilization by providers.
- For our example, assuming 49,000 providers working for high–hour recipients claim the full 48 hours per year, the overtime cost would be roughly $5 million General Fund annually
|
|
Consumer choice
|
- Some added convenience and greater consumer choice for the special circumstances in which overtime is used.
|
|
Administrative cost and complexity
|
- Results in some additional administrative activities—and thus costs and complexity—associated with designating and tracking the flexible overtime allotment to ensure it is not exceeded.
|
|
Need for additional providers
|
- Need for additional providers largely unchanged.
|
We noted earlier that it is uncertain if a sufficient number of additional providers will be available in all counties to meet the new demand for providers under the Governor’s proposed overtime restriction. If a county is unable to provide a consumer with a list of alternative providers or a backup provider, the recipient could presumably be forced to forgo authorized care. If the Legislature wishes to ensure that all recipients maintain their current level of access to services, then it could consider authorizing overtime for an existing provider when a county is unable to give recipients a list of alternative providers or supply a backup provider. By authorizing overtime for the recipient’s existing provider in these situations, the state could ensure that the IHSS recipient receives authorized service hours until a second provider or backup provider can be identified. We assess the modification of authorizing overtime for a provider in the event that the county is unable to provide alternative options to the recipient in Figure 5.
Figure 5
Authorize Overtime When Other Providers Are Unavailable
|
Criteria
|
Assessment of Modification Relative to Governor’s Proposal
|
|
Costs incurred for overtime
|
- Additional costs dependent upon the frequency and amount of overtime authorized.
|
|
Consumer choice
|
- Enhances—to some degree—consumer choice by enabling a recipient to receive care from his/her existing provider in the event that a county is unable to provide alternative options.
|
|
Administrative cost and complexity
|
- Some additional administrative activities—and thus costs and complexity—associated with tracking instances of authorized overtime.
|
|
Need for additional providers
|
- Reduces need for additional providers in the short term.
- Need for additional providers largely unchanged in the longer run.
|
The Cash and Counseling Model Is an Alternative to IHSS. Some states have implemented what is commonly referred to as the Cash and Counseling (or “Self–Determination”) Model as an alternative to the IHSS model for the provision of personal care and domestic services. Under the Cash and Counseling Model, consumers receive a monthly sum of available funds, based on the cost of the hours of in–home services that they would otherwise have been authorized to receive under an IHSS–like program. Recipients have more flexibility in the use of these funds than they would in a program like IHSS. They can use these monthly sums to set wage levels; hire a provider; and purchase permissible goods that make it easier to remain at home—expenditures not permitted now under IHSS. Under the Cash and Counseling Model, a counselor (often a social worker) helps consumers craft spending plans; offers advice on hiring, supervising, and training a provider; and monitors use of the available funds. A bookkeeper from a financial management services agency assists the consumer in the paperwork required to pay a provider’s wages and withhold taxes.
Under the Cash and Counseling Model, Live–In Providers Could Potentially Qualify for an Exemption From the Overtime Requirement Under Federal Labor Regulations. Based upon our review of the federal labor regulations, it appears that the Cash and Counseling Model could potentially have the effect of classifying the consumer as the sole employer of a live–in provider. Under such a scenario, the consumer could be able to claim the live–in domestic service worker exemption from the requirement to pay overtime to a home care worker. In effect, this would mean that live–in providers could work more than 40 hours per week and receive the set wage for all hours worked. As we noted earlier, half of IHSS recipients have a live–in provider. The ability of consumers with live–in providers to claim the live–in domestic service worker exemption under a Cash and Counseling Model would depend largely on the operational details of the program. Additionally, consideration of such a significant change to the IHSS program should weigh the benefits to consumers with live–in providers against the overall policy merits of this new model of care. We therefore recommend the Legislature require DSS to report in budget hearings with its initial take on the policy merits and trade–offs of the Cash and Counseling Model as an option for IHSS recipients with live–in providers. We assess this modification of providing a Cash and Counseling Model to recipients with live–in providers in Figure 6.
Figure 6
Cash and Counseling Model for IHSS Recipients With Live–In Providers
|
Criteria
|
Assessment of Modification Relative to Governor’s Proposal
|
|
Costs incurred for overtime
|
- No change in costs to pay overtime.
- Reduced Provider Backup System costs.
|
|
Consumer choice
|
- Enhances the consumer choice of high–hour recipients with live–in providers, who could continue to receive all assistance from a single provider of their choice.
|
|
Administrative cost and complexity
|
- Substantial administrative activities—and thus costs and complexity—associated with providing the “counseling” component of the model.
- Assuming all IHSS recipients with live–in providers chose the Cash and Counseling Model and received quarterly visits from a counselor, the cost of social worker time for these visits could be roughly $20 million General Fund annually.
- Potential additional costs associated with financial management services.
|
|
Need for additional providers
|
- Reduces the number of additional providers that would need to be recruited.
|
If the Legislature wishes to work within the framework of the Governor’s proposal to restrict overtime, then we recommend the following two changes related to implementation of the proposal.
Recommend Revision to Enforcement of Overtime Restriction for IHSS Providers. We described earlier that the Governor’s proposed one–year suspension of IHSS providers who claim overtime on two occasions—without any exceptions—raises concerns in that it could be unduly disruptive to some IHSS recipients. For example, if a provider does not receive the warning notice—because of a change of address or for some other justifiable reason—and as a result, claims overtime on two occasions, the recipient would lose his/her provider for a period of one year. The provider may also submit two timesheets simultaneously or in close succession—both claiming overtime—before he/she receives the warning notice. Short of appealing the suspension, the provider would have no recourse but to wait for the period of one year to elapse. In such instances, we find a one–year suspension to be unduly punitive to both provider and recipient. We therefore recommend the Legislature revise the enforcement of the overtime restriction by adding a suspension that is one month in duration prior to the one–year suspension. In effect, providers would be suspended for a period of one month if they claim overtime on two occasions. We find that a shorter suspension would have a similar deterrent effect as a one–year suspension in preventing IHSS providers from claiming overtime, but would not force a recipient to go without his/her preferred provider for an extended period of one year. We find that if a provider claims overtime on a third occasion, it would then be appropriate to suspend the individual for a period of one year.
Recommend Quarterly Reporting From DSS on Authorized Hours Versus Paid Hours. To increase legislative oversight of recipients’ access to service hours under the Governor’s overtime restriction, we recommend the Legislature require DSS to report quarterly on the total number of IHSS hours authorized compared to the total number of hours claimed by providers in each county statewide. A differential between these two indicators that is greater than the historical average may indicate a possible shortage of IHSS providers in a particular county.
We find the Governor’s proposal to restrict overtime in the IHSS program has merit in that it complies with the federal labor regulations in a manner that controls costs without reducing authorized service hours for IHSS recipients. Our analysis finds that the Governor’s proposal would result in a net fiscal benefit to the state. We therefore believe the Governor’s proposal should be given consideration by the Legislature as a reasonable starting point for addressing the federal labor regulations in the IHSS program. Although our analysis finds that the Governor’s proposal results in a net fiscal benefit to the state, we raise various policy concerns with the proposal. If the Legislature wishes to proceed within the Governor’s proposed framework of restricting overtime, then we recommend the Legislature consider potential modifications to address the policy concerns raised. Ultimately, the Legislature would want to weigh its policy priorities against the cost of each modification in order to arrive at a suitable approach for addressing the budgetary impact of the federal labor regulations in the IHSS program.
Aside from the Governor’s proposal to restrict overtime in the IHSS program, we find his proposal to fund the costs of newly compensable IHSS work activities to be reasonable. In regards to the Governor’s proposal to provide a rate increase for DDS vendors, we find it reasonable to assume that vendors will incur increased administrative costs to minimize overtime payments. Because of current data limitations on the exact amount of these costs, we recommend DDS report to the Legislature—no later than May 1, 2016—on the results of the proposed rate increase on impacted vendors in order to assess whether it is appropriate on an ongoing basis.
Overview of IHSS. The IHSS program provides personal care and domestic services to certain individuals to help them remain safely in their own homes and communities. In order to qualify for IHSS, a recipient must be aged, blind, or disabled and in most cases have income below the level necessary to qualify for SSI/SSP cash assistance. Recipients are eligible to receive up to 283 hours per month of assistance with tasks such as bathing, dressing, housework, and meal preparation. Social workers employed by county welfare departments conduct an in–home IHSS assessment of an individual’s needs in order to determine the amount and type of service hours to be provided. The average number of hours that will be provided to IHSS recipients is projected to be 84 hours per month in 2014–15 (after accounting for a previously enacted service reduction explained below). In most cases, the recipient is responsible for hiring and supervising a paid IHSS provider—oftentimes a family member or relative.
The IHSS Program Receives Federal Funds as a Medi–Cal Benefit. For nearly all IHSS recipients, the IHSS program is delivered as a benefit of the state’s Medicaid health services program (known as Medi–Cal in California) for low–income populations. The IHSS program is subject to federal Medicaid rules, including the federal medical assistance percentage reimbursement rate for California of 50 percent of costs for most Medi–Cal recipients. For IHSS recipients who generally meet the state’s nursing facility clinical eligibility standards, the federal government provides an enhanced reimbursement rate of 56 percent referred to as Community First Choice Option (CFCO). Because of the large share of IHSS recipients eligible for CFCO—about 40 percent of the caseload—the average federal reimbursement rate is 54 percent for the IHSS program. The remaining nonfederal costs of the IHSS program are paid for by the state and counties, with the state assuming the majority of the nonfederal costs.
Counties’ Share of IHSS Costs Is Set in Statute. Budget–related legislation adopted in 2012–13 enacted a county MOE, in which counties generally maintain their 2011–12 expenditure level for IHSS—to be adjusted only for increases to IHSS providers’ wages (when negotiated at the county level through collective bargaining) and an inflation factor of 3.5 percent beginning in 2014–15. Under the county MOE financing structure, the state General Fund assumes all nonfederal IHSS costs above counties’ MOE expenditure level. In 2014–15, the county MOE is estimated to be $994 million, an increase of $34 million above the estimated revised county MOE for 2013–14. To the extent wage increases negotiated at the county level are implemented in the remainder of 2013–14 or in 2014–15, the individual county’s MOE will increase by a percentage share of the annual cost of those wage increases.
Year–to–Year Expenditure Comparison. The budget proposes $6.4 billion (all funds) for IHSS expenditures in 2014–15, which is a 4.9 percent net increase over estimated revised expenditures in 2013–14. General Fund expenditures for 2014–15 are proposed at $2 billion, a net increase of $84 million, or 4.4 percent, above the estimated revised expenditures in 2013–14. This net General Fund increase incorporates the $34 million increase in the county MOE (which offsets General Fund expenditures) and several other factors described below.
- Costs to Comply With New Federal Labor Regulations. Increase of $209 million ($99 million General Fund) in response to recent federal labor regulations (affecting overtime pay and other matters) to take effect January 1, 2015. Please refer to the “Human Services Compliance With Federal Labor Regulations” analysis in this report for more detail on, and our analysis of, this proposal.
- Increase in IHSS Basic Services Costs. Increase of $68 million ($35 million General Fund) because of (1) caseload growth of 1.3 percent and (2) higher costs per hour because of the increase in the state–mandated hourly minimum wage from $8 to $9 beginning July 1, 2014. (Because the state enacted the minimum wage increase, the county MOE is not adjusted to reflect cost increases associated with the new minimum wage.)
- CMIPSII—Transition to New Phase. Decrease of $40 million ($20 million General Fund) due to the transition from the design, development, and implementation phase to the maintenance and operation phase for the CMIPS II IT system that stores IHSS case records, provides program data reports, and authorizes IHSS provider payments. As of November 2013, all 58 counties have transitioned to CMIPS II.
- Partial Rollback of Reduction in Authorized Service Hours. Year–over–year increase of $15 million ($8 million General Fund) as a result of implementing current law that requires an ongoing 7 percent reduction in IHSS authorized service hours beginning in 2014–15, rather than the one–time 8 percent reduction in service hours that applied in 2013–14. Total General Fund savings from the 7 percent reduction are estimated to be $181 million in 2014–15. This 7 percent reduction in service hours is part of an IHSS settlement agreement—adopted by the Legislature—that resolves two class–action lawsuits related to previously enacted budget reductions.
New Services Costs Related to Coordinated Care Initiative (CCI). The budget also reflects an increase of $49 million in total expenditures ($22 million as reimbursement from the Department of Health Care Services (DHCS) originating from the General Fund) for (1) increased IHSS hours for existing recipients as a result of the CCI and (2) new IHSS recipients who are expected to transition out of more costly institutional care settings and into IHSS because of the CCI. As part of the CCI, the IHSS program will shift from a Medi–Cal fee–for–service benefit to a Medi–Cal managed care plan benefit in certain counties beginning April 1, 2014. For more background on the CCI, please refer to The 2013–14 Budget: Coordinated Care Initiative Update.
Caseload Growth. The Governor’s budget assumes the average monthly caseload for IHSS in 2014–15 will be 453,417, an increase of 1.3 percent compared to the most recent estimate of the 2013–14 average monthly caseload.
LAO Comments on Overall Budget Proposal. We discuss elsewhere in this report the Governor’s proposal to respond to federal labor regulations as they apply to IHSS and DDS. The balance of the IHSS budget changes as outlined above appear reasonable. We have reviewed the caseload projections for IHSS as they relate to caseload growth in prior years and do not recommend any adjustments at this time. We note that the 2014–15 caseload estimate does not take into account a relatively small but likely increase in IHSS recipients as a result of the CCI. If we receive additional information that causes us to change our overall assessment, we will provide the Legislature with an updated analysis.
The CCL division of DSS develops and enforces regulations designed to protect the health and safety of individuals in 24–hour residential care facilities and day care. The Governor’s budget proposes expenditures of $118 million ($36 million General Fund) for CCL in 2014–15. This represents an 11 percent increase above estimated 2013–14 total expenditures (and a 37 percent increase above estimated 2013–14 General Fund expenditures). This increase is primarily the result of (1) the Governor’s proposal to take steps to enhance the quality of CCL and (2) providing General Fund monies to backfill federal funds that were lost as a result of the reduction in the federal Social Services Block Grant. Below, we provide some background on CCL and the Governor’s proposal.
The CCL oversees the licensing of various facilities including child care centers, adult residential facilities, group homes, foster family homes, and residential care facilities for the elderly (RCFE). The division is also responsible for investigating any complaints lodged against these facilities and for conducting inspections of the facilities. The state monitors approximately 66,000 homes and facilities, which are estimated to have the capacity to serve over 1.3 million Californians. Additionally, DSS contracts with counties to license an additional 8,700 foster family homes and family child care homes.
CCL Staffing and Facility Monitoring. The roughly 66,000 homes and facilities statewide directly under the regulatory purview of CCL are primarily monitored and licensed by just over 460 licensing analysts. These licensing analysts are located in 25 regional offices throughout the state and are responsible for conducting annually about 24,000 inspections and 13,000 complaint investigations. Current law requires CCL to conduct random inspections on at least 30 percent of all facilities annually, and each facility must be visited no less than once every five years. Although the CCL has had difficulty meeting these time frames in the past, the division is generally meeting these time frames currently.
Past Budget Reductions Have Increased the Time Between Annual Visits. Prior to 2002–03, most facilities licensed by CCL were required to be visited annually. Budget–related legislation enacted in 2003 lengthened the intervals between visits for most facilities from one year to five years. Additionally, the legislation included “trigger” language that initially required CCL to randomly visit 10 percent of facilities each year. If, in a given year, the number of citations identified exceeded that of the prior year by 10 percent, the random visits that were required to be conducted would increase by an additional 10 percent. As a result of this trigger methodology, CCL is now required to randomly visit 30 percent of facilities each year, and the requirement that each facility be visited every five years continues.
The CCL Began to Use a Key Indicator Tool (KIT). As a method to assist CCL in achieving the required inspection frequency, the KIT was formally adopted by CCL in the fall of 2010. This tool allowed CCL to increase the number of enforcement visits licensing analysts were able to conduct within existing budget constraints. The KIT is a measurement tool that is designed to measure compliance with a small number of licensing standards to predict compliance with all of the remaining licensing standards. In other words, whether or not a facility is in compliance with certain measures is considered to be an indicator of whether it will be in compliance with all measures. Due to the reliance on key indicators, rather than the more comprehensive assessment, it takes less time for licensing analysts to conduct a KIT inspection than a more comprehensive inspection. Only facilities that are in generally good standing are eligible for the KIT inspection, and at any given point during a KIT inspection, a licensing analyst may discover issues that trigger a more comprehensive inspection. The DSS has partnered with Sacramento State University to evaluate the KIT process and expects to have more information and analysis of the KIT available in the spring of 2014.
Recent Issues at Licensed Facilities Have Gained Attention. Recent health and safety incidents at licensed facilities have gained the attention of the media and the Legislature. These include incidents of neglect and abuse, as well as evidence in general of inconsistent and inadequate oversight, monitoring, and enforcement of licensing standards.
In response to recent health and safety issues discovered at facilities licensed by CCL, the Governor’s budget proposes a comprehensive plan to reform the CCL program. The proposal includes an increase of 71.5 positions and $7.5 million ($5.8 million from the General Fund) for the support of this proposed plan as well as budget–related legislation. Below, we describe the main components of the proposal and provide our analysis and recommendations in conjunction with each component that is discussed in detail. Overall, we find the Governor’s proposal contains elements that seek to respond to the recent issues and shortcomings identified at CCL. Although we do not raise any particular concerns with the level of staff requested by the department, we recommend some modifications to the accompanying budget–related legislation.
There are currently over 7,500 RCFEs that are licensed by CCL for a capacity to provide care for about 175,000 people throughout the state. Historically, RCFEs have been considered to be different from skilled nursing facilities (SNFs) because their purpose is to serve those with less acute medical needs than those who would qualify for skilled nursing home placement. However, as the population has aged, and the general policy goal of caring for people in the least restrictive setting has been emphasized, the role of the RCFEs has also changed. Although the populations at the RCFEs have changed to include those with more acute medical conditions, the regulatory and enforcement structure at CCL has not changed, and there are currently no staff in the division with medical expertise. Additionally, there are increasing numbers of corporations applying for licenses to operate multiple RCFEs in multiple regional office jurisdictions. Because the RCFEs that are part of a larger corporation are inspected by licensing analysts from various regional offices, it is difficult for CCL to recognize patterns of problems associated with specific corporations.
Begins to Develop Medical Expertise. The Governor’s budget proposes to establish a nurse practitioner at CCL to begin research on potential policy and regulatory changes that the department and Legislature should consider to ensure that there is adequate oversight of the RCFE population that is increasingly more medically fragile.
Establishes a Mental Health Populations Unit. In response to the changing needs of residents in RCFEs, and recent legislation that is expected to increase the number of facilities that treat individuals with mental health needs, the department proposes to establish four positions to create a mental health populations unit. This unit would create mental health and treatment expertise at CCL and be responsible for such things as developing regulations, answering policy questions from the field, and coordinating oversight activities with the DHCS.
Creates a Corporate Accountability Unit. The Governor’s budget proposes to establish two positions to create a corporate accountability unit that would be responsible for identifying and addressing issues of systemic noncompliance by RCFE operators with facilities in more than one of the geographic areas overseen by regional offices.
LAO Analysis: Changing Medical Conditions of RCFE Clients Warrants Initiating Proposed Health Expertise at DSS. Traditionally, DSS has had a contract with a public health nurse consultant to provide medical expertise on specific complaint investigations. Potential evidence that the population in the RCFEs is becoming increasingly more medically complex is that DSS has become more reliant on the use of this contracted nurse in recent years. In 2011–12, DSS used this nurse for 30.5 hours of services. In 2012–13, the use of the contract nurse grew to 252 hours. Finally, only six months into 2013–14, the department has used the nurse for 272 hours of service. Another indication of the increasing medical complexity of residents at RCFEs is that many RCFE providers have successfully secured waivers to provide hospice level care in the facilities. Given the changing medical conditions of RCFE residents, we find merit in the department’s proposal to have a public health nurse assessing the appropriate role for RCFEs and whether changes to the enforcement structure are needed to adequately monitor these changing facilities. Building this capacity at DSS would enable it to consider whether the RCFEs are an appropriate placement for those with more acute medical conditions, and if so, whether licensing requirements should be different for RCFEs that provide services to those with more complex heath needs. Finally, this nurse could assist the department in considering whether partnerships with the Department of Public Health (DPH) (the entity that licenses SNFs) should be established for the monitoring of RCFEs that are authorized to serve clients with more complex medical conditions.
Due to the increasing workload associated with recent legislation, and the changing profile of those applying for licenses to operate RCFEs, we also recommend approving the Governor’s request to establish a mental health populations unit and corporate accountability unit for CCL.
Currently, licensed facilities are responsible for paying an application fee and an annual fee which is set in statute. The revenue from these fees are used to partially offset the cost of CCL enforcement and oversight activities. We note that the last fee increase for licensed facilities was a 10 percent increase in 2009. In addition to these annual fees, facilities are assessed civil penalties in the event they are found to have committed a licensing violation. Below, we describe the Governor’s proposal to increase licensing fees and penalties.
Increases Application and Annual Licensing Fees for Facilities. This proposal increases the application and annual licensing fees for facilities by 10 percent. Additionally, the budget includes trailer bill language that would require fees to be adjusted annually by the Consumer Price Index. The DSS estimates that this increase in the application and annual licensing fees would generate about $2 million in additional annual revenue to support CCL operations. (The fee is estimated to generate a total of roughly $21 million in 2014–15.) For the 2014–15 budget, the Governor assumes revenue from the fee increases to be $1 million to account for the time needed to allow for a notification period for facility providers. Figure 7 provides examples of what this change in the fee structure would mean for various provider types.
Figure 7
Selected CCL Fee Levels: Current Law Compared to Governor’s Proposal
|
Examples of Facilities
|
Current Law
|
|
Governor’s Proposal
|
|
Difference
|
|
Application
|
Annual
|
Application
|
Annual
|
Application
|
Annual
|
|
Residential care facility for the elderly (4–6 people)
|
$825
|
$413
|
|
$908
|
$454
|
|
$83
|
$41
|
|
Adult day program (16–30 adults)
|
275
|
138
|
|
303
|
152
|
|
28
|
14
|
|
Family child care center (1–8 children)
|
66
|
66
|
|
73
|
73
|
|
7
|
7
|
|
Child care centers (31–60 children)
|
880
|
440
|
|
968
|
484
|
|
88
|
44
|
|
CCL = Community Care Licensing.
|
Requires DSS to Monitor the Appropriateness of the Fee Over Time. Proposed budget legislation requires the department to analyze the fees at least once every five years to determine whether the levels are appropriate or should be adjusted.
Increases Civil Penalties. The Governor’s budget proposes to increase civil penalties imposed on licensees for three types of serious noncompliance—(1) initial finding of the violation, (2) repeat violations, and (3) failure to correct the violation. The fact that the maximum civil penalty under current law is $150 per day has been a concern for the department and stakeholders—especially in instances of significant noncompliance or even death of a client. The proposed changes are as follows.
- Serious Violations. Current law defines a serious violation as such things as (1) fire clearance violations, (2) accessible firearms, and (3) accessible bodies of water. The Governor’s budget proposes to add “violations that result in the injury, illness, or death of a client” to the list of serious violations. In addition to this change, proposed budget–related legislation increases the amount of the civil penalty that can be assessed for these violations from a maximum of $150 per day to five times the licensee’s annual fee per day. This means that facilities with higher annual fees (larger facilities) would pay more in civil penalties than those with lower annual fees (small facilities). As noted above, under this proposal, annual licensing fees will be adjusted each year for inflation. Since this proposal ties the civil penalties to annual fees, the civil penalties would also be adjusted annually.
- Repeat Violations. It is proposed that any facility that is cited for repeating the same serious violation within 12 months of the previously cited violation will have an immediate civil penalty assessed that is three times the facility’s annual licensing fee. If the violation continues, a penalty of 1.5 times the annual fee will be assessed daily until the violation is corrected. Under current law, facilities with repeat violations are assessed an immediate civil penalty of $150 and $50 for each day the violation continues. Figure 8 provides examples of what the proposed change in civil penalties for serious violations would mean for various facility types.
- Failure to Correct Violations Within Specified Time Frame. If a violation is not corrected within the time frame specified in the notice of the violation, a civil penalty that is 25 percent of the annual fee is assessed for each day the violation continues.
Figure 8
Selected CCL Civil Penalty Levels for Serious Violations:
Current Law and Governor’s Proposal
|
Examples of Facilities
|
Current Law
|
|
Governor’s Proposal
|
|
Initial
|
|
Repeat Within
12 Months
|
Initial
|
|
Repeat Within
12 Months
|
|
(Per Day)
|
(First Day)
|
(Each Additional Day)
|
(Per Day)
|
(First Day)
|
(Each Additional Day)
|
|
Residential care facility for the elderly (4–6 people)
|
$150
|
|
$150
|
$50
|
|
$2,270
|
|
$1,362
|
$681
|
|
Adult day program (16–30 adults)
|
150
|
|
150
|
50
|
|
760
|
|
456
|
228
|
|
Family child care center (1–8 children)
|
150
|
|
150
|
50
|
|
365
|
|
219
|
110
|
|
Child care centers (31–60 children)
|
150
|
|
150
|
50
|
|
2,420
|
|
1,452
|
726
|
|
CCL = Community Care Licensing.
|
Creates a Late Fee. The budget proposal requires the department to charge a late fee that represents an additional 10 percent of the unpaid civil penalty when the licensee fails to pay the penalty by the due date. The late fee would not be assessed on licensees who are in compliance with a payment plan developed by DSS. The proposal also prevents facilities that have not paid the civil penalties from new admissions or expansions of facility capacity.
Broadens Eligible Uses of the Civil Penalty Fine Revenue. Currently, civil penalties that are assessed on licensed facilities are deposited in the Technical Assistance Fund and are required to be used by the department exclusively for the technical assistance, training, and education of licensees. Proposed budget–related legislation amends current statute to state that these funds may be used for these activities. In addition to the proposed statutory change in the allowable usage of the penalty revenues, the department is proposing budget bill language that would allow the Director of Finance to use the unspent revenue from the penalties deposited in the fund to offset the overall General Fund cost of the program. We note that the change in the civil penalty structure could result in significantly more penalty funds being deposited in this fund than in prior years.
LAO Analysis: Reporting Back on the Appropriateness of Fees Will Increase Legislative Oversight. We find that the Governor’s proposal to increase fees has merit. Since the changes the Governor is seeking through the overall CCL proposal are aimed at improving the CCL system generally, it makes sense that facilities would share in the cost of those improvements. Although we are unsure of the exact level that the application and annual fees should be, the Governor’s approach requires the department to report back on the appropriateness of the fee levels on an ongoing basis. This report would enhance the Legislature’s oversight of the fees and assist it in determining whether the growth in fees is outpacing or keeping pace with the growth in the total program, and whether any adjustments to the fee structure are warranted.
LAO Analysis: CCL Penalties Should Be Increased Incrementally. On the issue of civil penalties, we think it is reasonable to increase the maximum penalty for the most serious violations beyond what current law allows. It is difficult to assess the “right” level of civil penalty that serves to deter serious violations. Other states perform similar licensing functions to CCL and there is variation in the levels of civil penalties in place across states. California’s assessment of $150 per day for serious noncompliance, however, is relatively low compared to other states. Although it is difficult to determine the appropriate levels at which to set civil penalties, we agree with the concept of basing the level of the civil penalty on the size of the facility. This is because setting a flat rate for all facility types (such as the $150 in place under current law) could result in an unequal deterrent effect across facility types—a $150 penalty for a very small facility with a limited amount of revenue may be a larger deterrent than it would be for a larger facility that generates more revenue. Additionally, the act that resulted in the civil penalty puts more people at risk in larger facilities than in smaller facilities.
Because of the uncertainty surrounding the appropriate level of civil penalties, and the variations in these levels across states, the Legislature may wish to consider a more gradual ramp up of civil penalty levels than that which is proposed by the Governor. For example, the Legislature could set civil penalties for the initial serious violation at three times the annual licensing fee (rather than at five times as proposed by the Governor) and repeat violations equivalent to the annual license fee level (rather than at three times as proposed by the Governor).
This gradual increase to the civil penalties would still allow for a significant increase in penalty levels in the budget year, but also allow the Legislature to evaluate the appropriateness of the penalties again in a year to determine whether additional increases should be implemented. We understand that the current, low civil penalties for serious violations are especially concerning when the violation is related to the serious injury, or even the death, of a resident. One option would be to implement an even more significant increase in the civil penalty amounts for these particular violations. We recommend the Legislature require DSS to report back annually with information that will help the Legislature evaluate the appropriateness of the levels of civil penalties and determine whether further adjustments are warranted. This report should include the number of serious violation penalties issued, the number of penalties that were appealed, and the rate of the collection of the penalties.
LAO Analysis: Reasonable to Use Penalty Revenues to Offset General Fund Costs. Because the funding from penalties is not a predictable and reliable revenue source, the Governor’s budget does not assume revenue from penalties to fund the CCL proposal. However, as we noted, the proposed legislation opens up the possibility to use these funds for purposes beyond what current law allows. Additionally, the proposed budget bill language would authorize the Director of Finance to use unspent penalty revenues to offset General Fund costs in the program. We find it to be reasonable to use penalty revenue to fund the basic cost of the CCL program. We note that using fee and penalty revenues to support licensing/permitting and enforcement activities is a common practice among state regulatory programs. However, if the Legislature has other priorities for the penalty revenues, beyond offsetting General Fund costs, it could enact statutory changes that stipulate such priorities.
The Governor’s proposal requests 34.5 positions to centralize two activities that are currently being provided at each regional office. By centralizing these activities at the state headquarters level, it is intended by this proposal that staff at the regional offices will be freed up to conduct more inspections.
Creates a Centralized Application Processing Unit. Currently, applications for licensure are handled at the regional office level. Licensing analysts who would otherwise be in the field conducting inspections dedicate a portion of their time to processing applications for licenses. The budget proposes to centralize this function by creating a specialized, trained application processing unit at the state headquarters level.
Establishes a Statewide Complaint Hotline. Similar to license application processing, complaints against licensed facilities are handled at the regional offices. Licensing analysts who would otherwise be conducting inspections rotate the responsibility to stay in the office to receive complaint calls. The Governor’s budget proposes to centralize the complaint intake process and to create a statewide toll–free public complaint hotline. In 2012–13, DSS received 9,698 licensing related complaints. In addition to receiving calls related to complaints, the regional offices receive general inquiries from the public and requests to verify licensing status.
Provides Support Staff to Assist Special Investigators. The Governor’s budget requests six positions to assist special investigators at CCL. These special investigators have peace officer status and are responsible for investigating the most serious complaint allegations received by CCL.
LAO Analysis: Centralizing Application Processing and Complaint Intake Could Increase State Oversight and Efficiency. We find that centralizing these activities could result in efficiencies, increased consistency, and better state–level oversight for CCL operations. It is our understanding that the current process for applying for a license is cumbersome from the applicant perspective. In some cases, an applicant that is applying for licensure in several different regions may receive different application–related questions and guidance from the different licensing analysts in the various regional offices. By creating a centralized application processing unit where staff are trained specifically on processing applications, CCL would be able to ensure that a single licensee with multiple applications gets one reviewer and one set of instructions. Additionally, from the state’s perspective, having the application processed centrally would allow it to better track applicants who are operating multiple facilities throughout the state.
By providing a statewide complaint hotline, there would be benefits to both the public and state. The public would have one number to call for any complaint they would like to report to the licensing agency. Additionally, the public could call this number to verify a facility’s licensure status and the citation and complaint history for a particular facility. From the state’s perspective, creating this centralized unit would allow for improved consistency in complaint intake and response. By centralizing the intake of complaints, the state will be able to better track the types of complaints coming in statewide and potentially recognize patterns that may indicate a need for an inspection or increased enforcement.
LAO Analysis: Support for Special Investigators Appears Reasonable. It is reasonable to provide these support staff for the special investigator peace officers at CCL. These assistants would perform the activities that do not require peace officer status, but are currently being done by peace officers. By freeing the investigators of this workload, they could be available for more field work.
Currently, CCL has the authority for three major enforcement actions after discovering instances of serious noncompliance—(1) create a corrective action plan (2) issue civil penalties, and (3) revoke or suspend the license of a facility. In some cases, while issuing a civil penalty or corrective action plan may not seem like enough of a penalty for a particular violation, revoking the license may seem to be too severe. Additionally, there are significant logistical details involved when a decision has been made to revoke a license—most importantly, alternative placements for residents or clients of the facility that had its license revoked must be secured. For the clients of these facilities, these relocations can be physically and emotionally challenging.
Governor’s Budget Establishes a Temporary Manager and Receivership Process. The Governor’s budget proposes to provide DSS with an additional enforcement tool for CCL. Essentially, in instances where the department determines that the residents of a particular facility are likely to be in danger of serious injury or death, and the immediate relocation of clients is not feasible, a temporary manager or receiver could be appointed to act as the provisional licensee. The temporary manager or receiver would stay in the role until the facility has become compliant with the law, a new operator takes over the facility and becomes the licensee, or the facility is closed and residents are transferred to other facilities. The proposal does not apply to small facilities that serve less than six residents and are also the principal residence of the licensee. It is our understanding that the funds to pay for this process would be paid from the revenues generated by the facility. To the extent these revenues are not enough, the department could advance funding from the Technical Assistance Fund (the fund that holds the civil penalties) to cover the costs. The budget–related legislation requires the licensee to ultimately reimburse the department for the advanced costs.
LAO Analysis: New Enforcement Tool Makes Sense in Concept, but Details Warrant Careful Consideration. We agree with this proposal in concept. As a result of the complex issues involved in revoking the license of a facility, it is reasonable to authorize CCL to use the additional enforcement tool involving a temporary manager and receivership structure. However, we note that the Governor’s proposed trailer bill language includes many implementation and policy details related to such things as (1) limits on the amount of funding the temporary manger or receiver is able to spend while acting in this role, (2) appeal rights of the licensee, and (3) length of time that the temporary manger or receiver is authorized to act in this capacity. It is our understanding that this temporary manager and receivership process was largely modeled off of the process DPH uses in its oversight of SNFs. Given the significant implementation details that are specified in the proposed legislation, we recommend that the Legislature require the department to report at budget hearings on (1) the main differences between the CCL proposal and how DPH currently administers its receivership and temporary manager process for SNFs, and (2) the rationale for these differences.
The current IT systems used for CCL were not designed to have the capacity to produce automated reports that allow for statewide oversight and tracking of complaints, penalty actions, or enforcement outcomes. As a result, compiling data for CCL to use to perform oversight and provide information to the public is mostly done manually and is not usually able to be done quickly. The Governor’s budget proposes to establish six positions to form a unit dedicated to conducting quality assurance reviews on a regular basis. This unit would be tasked with reviewing the data that is available in the current system to (1) respond to requests for information, (2) identify training needs in the field, and (3) identify patterns that may indicate vulnerabilities in the current enforcement process.
The administration has acknowledged the shortcomings of its current CCL IT infrastructure. In response to this, the administration has indicated that it is currently in the early stages of analyzing the costs and potential benefits of implementing a new IT system for CCL.
LAO Analysis: Given Current IT Limitations, Quality Assurance Unit Proposed Is Reasonable. Given that there is an immediate interest in the collection of quality licensing data, we recommend approving the department’s request to create a quality assurance unit. It is our understanding that this unit would be able to track performance of staff at the regional office level. Additionally, this unit would be able to identify training needs based on patterns it may uncover in the review of data. Although we recommend approving the establishment of a quality assurance unit, since the department is currently in the early stages of evaluating the costs and benefits of a new IT system, we recommend that these positions be limited–term to allow for a future evaluation of the workload as the state moves towards the implementation of the IT project. Additionally, if there are certain activities that the Legislature would want the new system to have the capacity to perform, these priority functions should be communicated to the administration during the budget hearings process. Examples of these priority functions could be the ability for the new system to allow the public to access current and historical licensure and citation history online and the ability to run statewide compliance and demographic reports.
Training for Licensing Analysts. The department indicates that in difficult budget times, it reduced the amount of training it required licensing program analysts to complete from six weeks of intensive training to 18 hours of webinar training and 80 hours of in–person training. The Governor’s budget proposes to restructure the training for licensing analysts to require two additional weeks of in–class training and an ongoing training requirement.
Training for Licensing Managers. Although licensing managers participate in 80 hours of state–required general supervisory training, DSS currently does not have CCL–specific training for licensing managers. The licensing managers are responsible for reviewing complaint investigations and administrative actions taken by the licensing analysts. In some cases, the documents they are reviewing involve allegations of injury, illness, or death. The Governor’s budget proposes one position and funding for a contract with an academic institution to develop a CCL–specific training curriculum for licensing managers.
LAO Analysis: A More Robust Training Program Could Increase Enforcement Consistency. It is our understanding that there is significant variation and inconsistency across the state in terms of how licensing analysts and managers perform their enforcement–related duties. The lack of a robust training program for licensing analysts and managers is likely a contributor to this. We recommend adopting the administration’s proposal to create a more robust training program for analysts and managers. Providing this training could result in a more consistent application and enforcement of licensing statutes and regulations across the state. This training is increasingly important when coupled with the Governor’s proposal to increase fines for civil penalties. Because the civil penalties are proposed to be higher under the Governor’s proposal, it is even more important that the licensing analysts and managers are appropriately assessing these penalties.
One issue that has been raised by licensees is that the increase in the time between periodic, scheduled annual inspections has resulted in CCL providing more “reactive” enforcement than “proactive” enforcement. It is thought that if licensing analysts were visiting facilities more frequently, they could provide advice to licensees that would help them maintain compliance with the law and avoid penalties in the first place. To address some of the concerns from the licensees, the Governor’s budget contains two components that aim to provide more guidance to facility licensees and administrators to potentially reduce the instances of noncompliance. The first component of the proposal is the establishment of a technical assistance unit at the state level that is available to respond to questions and requests for guidance from licensees and licensing analysts. It is our understanding that this unit would be able to provide field staff and licensees with guidance to ensure that the actions they take comply with the law and assist in preserving the health and safety of the clients.
Currently, facilities with residential clients are required to have certified administrators who are responsible for the operation of the facility. These administrators must attend 40 hours of department–approved training in order to be certified. This proposal also includes a component that would provide for the department to conduct quality assurance monitoring of the training programs facility administrators are required to attend.
LAO Analysis: Increased Intervals Between Inspections Makes Up–Front Guidance Important. We find that these additional resources to provide more up–front guidance to licensees, administrators, and licensing analysts in the field is a good investment. Since the Governor’s proposal increases penalties for noncompliance, it is important that program rules and expectations are clearly communicated to facility licensees and administrators to ensure that the state is holding them accountable for complying with rules that were effectively communicated to them.
Governor’s Approach to First Address CCL Infrastructure Makes Sense. Overall, we find this to be a comprehensive proposal that seeks to respond to identified failings of CCL, including the recent health and safety issues uncovered in facilities licensed by CCL. We understand that there is interest in exploring options to decrease the time intervals between required licensing visits, but we find that it is reasonable to first address these general, programmatic infrastructure–related issues—such as developing a training curriculum for analysts, evaluating the changing role of RCFEs, reforming the fee and penalty structure, and changing the way complaints and applications are processed—prior to making an increased investment in additional inspectors at the local level. This is because, until the administration addresses the current inefficiencies and shortcomings of CCL, the actual level of additional resources needed to appropriately increase the frequency of inspections is unknown. Addressing the inefficiencies and implementing a new quality assurance unit and IT system for CCL could lead to a more targeted, informed approach to conducting inspections and oversight. Further, there are some aspects of the Governor’s proposal, such as training improvements, that should be in place before there is a significant increase in licensing analysts to conduct inspections.
In summary, we support the administration’s proposal to begin to respond to the recent problems identified at CCL. Although we do not raise any particular concerns at this time with the level of the staffing request—71.5 positions proposed (with the exception of recommending that six positions be approved as limited term)—we do make several recommendations for modifications to the accompanying budget–related legislation. Specifically, we recommend that the Legislature consider:
- Implementing a more gradual increase in the level of civil penalties assessed for findings of serious noncompliance, with periodic reports to the Legislature.
- Using the budget hearing process to (1) require the department to provide more detail on the temporary manager and receivership process, and (2) communicate CCL IT–related priorities to the administration.
The CalWORKs program was created in 1997 in response to the 1996 federal welfare reform legislation, which created the federal Temporary Assistance for Needy Families (TANF) program. CalWORKs provides cash grants and welfare–to–work (WTW) services for families whose income is inadequate to meet their basic needs. Grant amounts vary across the state and are adjusted for family size, income, and other factors. For example, a family of three in a high–cost county that has no earned income currently receives a monthly cash grant of $638 per month (equivalent to 39 percent of federal poverty guidelines). A family in these circumstances would generally also be eligible for food assistance through the CalFresh program in the amount of $494 per month and health coverage through Medi–Cal.
CalWORKs Work Requirement. As a condition of receiving aid, CalWORKs families that include able–bodied adults are required to be employed or participate in WTW activities (hereafter referred to as the “work requirement”) and are entitled to receive services intended to help meet this requirement. Adults that fail to comply with the work requirement without good cause are sanctioned by being removed from the calculation of the family’s grant, resulting in decreased assistance (generally about $125).
Barriers to Employment. Many CalWORKs recipients face circumstances, commonly referred to as “barriers,” that make it difficult to obtain long–term employment. These barriers can include low educational attainment, low English proficiency, lack of work experience, responsibility of caring for disabled parents or children, lack of child care, learning disabilities, poor mental health, substance abuse, domestic violence, prior criminal convictions, and others. In some cases, the CalWORKs program will exempt recipients with certain barriers from the work requirement. In other cases, the CalWORKs program provides services intended to help address the barriers. These services include adult basic education, English as a Second Language services, subsidized child care, unpaid and subsidized work experience opportunities, mental health and substance abuse treatment, domestic violence services, and others.
CalWORKs Funding. CalWORKs is funded through a combination of California’s federal TANF block grant allocation ($3.7 billion annually), the state General Fund, and county funds (including significant amounts spent by counties as a result of state–local realignment). In order to receive its annual TANF allocation, the state is required to spend an MOE amount from state and local funds to provide services to families eligible for CalWORKs. In recent years, this MOE amount has been $2.9 billion. While the CalWORKs program makes up the majority of TANF and MOE spending, it is important to note that the TANF block grant is used to fund a variety of programs in addition to CalWORKs, and some General Fund expenditures outside CalWORKs are counted toward the MOE requirement.
As shown in Figure 9, the Governor’s budget proposes $5.5 billion in total funding for the CalWORKs program in 2014–15, a net increase of $83 million over estimated current–year funding. This increase is the net effect of a $176 million increase in employment services and $5 million in other increases, partially offset by a total of $98 million in decreased funding for cash grants, child care services, and program administration. These year–over–year changes largely reflect (1) lower costs due to expected CalWORKs caseload decline; (2) the implementation of program changes enacted in previous years, including various significant changes to CalWORKs employment services and a 5 percent grant increase effective March 2014; and (3) a $10 million increase in funding tied to a proposed Parent/Child Engagement Demonstration pilot project. Each of these items is discussed in greater detail below.
Figure 9
CalWORKs Budget Summary
All Funds (Dollars in Millions)
|
|
2013–14
Estimated
|
2014–15
Proposed
|
Change From 2013–14
|
|
Amount
|
Percent
|
|
Cash grants
|
$3,072
|
$3,051
|
–$22
|
–1%
|
|
Employment services
|
1,185
|
1,361
|
176
|
15
|
|
Stage 1 child care
|
406
|
385
|
–22
|
–5
|
|
Administration
|
567
|
511
|
–55
|
–10
|
|
Othera
|
172
|
177
|
5
|
3
|
|
Totals
|
$5,402
|
$5,485
|
$83
|
2%
|
While total funding for CalWORKs would increase under the Governor’s proposal, General Fund support for CalWORKs would decrease from $1.2 billion in 2013–14 to $637 million in 2014–15. This primarily reflects a decision made as part of the 2013–14 budget package to use certain funds provided to counties under 1991 realignment for local health programs to offset General Fund expenditures in the CalWORKs program. Under the Governor’s proposal, the amount of health realignment funds used to offset General Fund costs in CalWORKs would increase by $600 million in 2014–15 to a total of $900 million. (For more information on the redirection of health realignment funds, see the Medi–Cal write–up in our report The 2013–14 Analysis of the Health Budget.)
CalWORKs Caseload Decline Expected to Continue During Budget Year. The CalWORKs caseload rose substantially during the recent recession, peaking in June 2011 at over 597,000 cases. Since that time, the caseload has been declining due to enacted policy changes and an improving labor market. The budget estimates that the average monthly caseload in 2013–14 will be 545,647 cases—2.5 percent lower than during the previous year. The average monthly caseload is projected to further decline by 3 percent in 2014–15 to 529,367 cases. A declining CalWORKs caseload generates program savings as fewer families receive cash assistance and WTW services. In the Governor’s budget, these savings are more than offset by net costs associated with ongoing and proposed initiatives discussed below. We find the administration’s caseload estimate reasonable and consistent with our expectations of a long–term downward caseload trend as the labor market and earnings prospects for low–income families continue to improve.
The following sections will (1) discuss the implementation of recently enacted program changes; (2) review the role of realignment in the CalWORKs budget, focusing on a recently created mechanism that funds future CalWORKs grant increases with 1991 realignment growth revenues; and (3) evaluate the Governor’s Parent/Child Engagement Demonstration proposal.
Several significant program changes enacted in prior years will continue to be implemented during 2014–15. The following section briefly describes the state’s progress in implementing these changes and the associated fiscal impact assumed in the Governor’s budget.
Phase–Out of Short–Term Young Child Exemptions
Beginning in 2009–10 and continuing through half of 2012–13, the Legislature temporarily broadened the circumstances under which counties could exempt CalWORKs recipients from the work requirement. Budgetary savings were achieved by not providing subsidized child care and employment services to most of the exempted population (some exempted recipients chose to participate in WTW activities despite their exemption). These temporary exemptions were eliminated effective January 2013, and counties are required to meet with all formerly exempt recipients by the end of 2014 to inform them that, unless the recipients are eligible for and choose to take an additional exemption, they are now subject to the work requirement and are entitled to receive supportive services. As shown in Figure 10, the rate of exemption from the work requirement increased dramatically in 2009–10, but has begun to decrease since early 2013 as counties have begun to make contact with formerly exempt recipients. The DSS estimates that 11,769 cases remain to be contacted before the end of December 2014. The Governor’s budget proposal includes $99 million (General Fund) to provide child care and employment services to families newly participating in WTW. This amount appears reasonable and is consistent with our understanding of the pace and cost of phasing out the short–term exemptions.
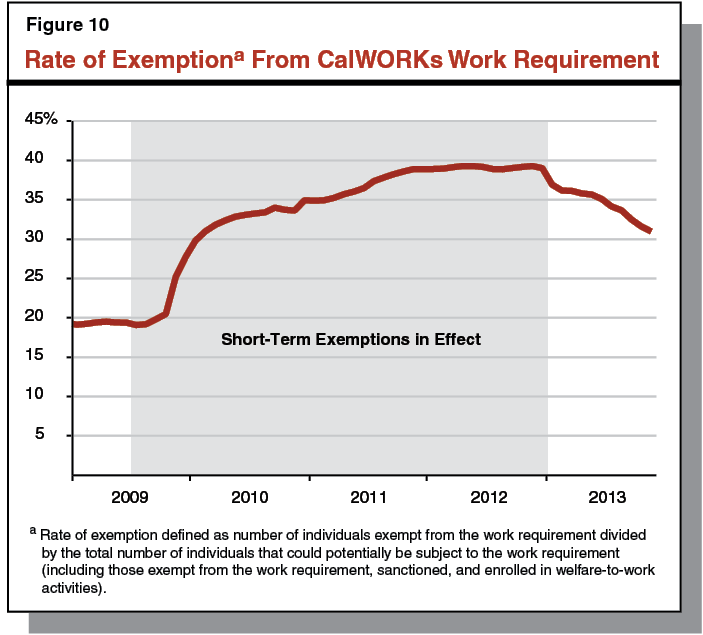
WTW 24–Month Time Limit
As part of the 2012–13 budget package, the Legislature enacted two fundamental, ongoing changes to CalWORKs. First, the state rules that govern the activities a recipient may participate in to meet the work requirement were altered to provide greater flexibility to recipients to participate in activities and receive services that best align with addressing barriers to employment. Second, a new 24–month limit on adult eligibility for CalWORKs assistance under these more flexible rules was introduced. Once 24 months of assistance under the flexible state rules are exhausted, adult recipients are required to meet the work requirement under relatively less–flexible federal work rules, which generally have a heavier emphasis on employment, as opposed to education, training, or certain activities designed to address barriers to employment (such as mental health or substance abuse treatment). Recipients that fail to meet the applicable work rules at any time while receiving aid are sanctioned by having their family’s grant reduced by the adult portion. Months of participation under the 24–month time limit need not be consecutive, meaning that cases that participate in activities that meet federal requirements in a given month will not have that month counted against their limit. Additionally, counties may grant up to 20 percent of cases that have passed the 24–month limit and meet certain criteria an extension to continue to participate under state rules.
We expect that the implementation of the WTW 24–month time limit may result in some General Fund savings in two primary ways. First, increased work rule flexibility may result in a greater number of families finding employment with wages high enough to disqualify them from CalWORKs assistance. Second, some adult recipients will reach the 24–month time limit, fail to comply with federal work rules, and not be granted extensions, resulting in decreased cash assistance and employment services for these families. The administration has not estimated any savings from the WTW 24–month time limit during 2014–15. We believe this is appropriate for a few reasons. First, if a greater number of recipients found employment because of the program changes, we would expect the CalWORKs caseload to decline. However, there are many factors that could cause the CalWORKs caseload to decline and data are not available to isolate the effect, if any, of the new time limit and related changes. Second, the earliest any recipient could reach the 24–month time limit is January 2015; however, there are many situations that can result in a month not being counted toward the 24–month limit, thereby extending the earliest date for most to reach the 24–month limit past January 2015. Based on limited, preliminary data, less than one–third of recipients participating in WTW had the month of November 2013 count against their limit. Based on this limited data, we expect that the number of recipients exhausting their 24–month limit in the latter half of 2014–15 will be relatively small. Additional data needed to more precisely estimate the fiscal and policy effects of the 24–month limit will become available as implementation continues during 2014.
As part of the 2013–14 budget package, the Legislature enacted Chapter 21, Statutes of 2013 (AB 74, Committee on Budget), which included three strategies intended to help recipients more effectively engage with the WTW component of CalWORKs in light of increased work rule flexibility and the introduction of the 24–month time limit. Similar to these previous changes, the early engagement strategies were in part intended to further assist CalWORKs recipients to address barriers to employment. These strategies, collectively known as “early engagement,” include an expansion of subsidized employment; additional funding for counties to provide enhanced services, known as “family stabilization services,” to certain CalWORKs families; and funding to develop and implement a new statewide WTW appraisal tool. The Governor’s budget proposes a combined $139 million (General Fund) for early engagement in 2014–15, a $92 million increase over estimated spending on these initiatives in 2013–14. This increase essentially reflects the costs of a full year of implementation. Progress on implementing each of the early engagement strategies and proposed funding for 2014–15 are discussed in detail below.
Expanded Subsidized Employment. Counties were allocated $39 million in September 2013 to create additional subsidized employment positions for CalWORKs recipients. This amount was budgeted to allow for gradually building up the number of new subsidized positions to roughly 8,250 by June 2014. Chapter 21 defined broadly how the additional funds could be used and required counties to submit plans to DSS describing in greater detail how they intend to use the funds. The DSS reports that several counties have submitted plans to date, with more expected in the coming months. For 2014–15, the Governor proposes to increase the amount of funding for expanded subsidized employment to $134 million (General Fund), with offsetting grant savings of $38 million (a net amount of $96 million). Offsetting grant savings occur because of reductions in cash assistance received by subsidized employment recipients to reflect increased wages. This amount represents funding to continue 8,250 positions through the 2014–15 fiscal year. As we have noted in previous analyses, this represents a substantial expansion of the role of subsidized employment in the CalWORKs program. In light of the Legislature’s approval of expanded subsidized employment in the 2013–14 budget package, we find that the magnitude of increased funding for subsidized employment is consistent with the costs of continued implementation for a full year.
Family Stabilization Services. Counties were allocated $11 million in November 2013 to provide intensive case management and specialized services to adults and children in CalWORKs families facing certain immediate, destabilizing needs during the second half of 2013–14. Chapter 21 broadly defines eligibility for family stabilization services and what types of services may be provided, and requires counties to submit plans to DSS outlining how family stabilization funds will be used. However, implementing instructions from DSS were delayed and no county plans had been received by DSS at the time this analysis was prepared. For 2014–15, the Governor proposes to increase the amount of funding for family stabilization services to $26 million (General Fund), which largely represents the same level of funding as was provided in 2013–14 but for a full year of services. Without the experience of county implementation, it is difficult to assess the ongoing need for family stabilization services. We find the budgeting methodology used by the administration to establish the funding level for the services to be a good start and recommend that the Legislature reevaluate the funding level for family stabilization as part of the 2015–16 budget process, taking into account county experience that will have accumulated by that time.
Standardized Appraisal. Chapter 21 expanded the scope of the appraisal performed for new WTW participants, and required counties to use a new standardized appraisal tool to be developed by DSS beginning in January 2014. The 2013–14 budget package included $8 million in additional funding for counties to account for the additional time requirements of the new appraisal. However, the development of the standardized appraisal has also been delayed. As of the writing of this analysis, DSS is in the final stages of engaging a contractor to customize and implement a standardized appraisal tool that will be known as the Online CalWORKs Appraisal Tool, or OCAT, which is anticipated to be available to all counties by July 2014. The Governor proposes $16 million (General Fund) in additional funding for counties for 2014–15. This amount reflects a full year of implementation of OCAT.
As part of the 2013–14 budget package, the Legislature also approved a 5 percent CalWORKs grant increase that will take effect in March 2014. For a family of three in a high–cost county that has no earned income, the amount of cash assistance received will increase to $670 per month (41 percent of federal poverty guidelines), while the statewide average grant is expected to rise to $480 per month during 2014–15. The administration estimates that the cost of providing this grant increase from March through June of 2014 is $58 million, with a full–year cost in 2014–15 of $168 million. As described in greater detail in the following sections, the costs of this grant increase are to be funded with certain 1991 realignment growth revenues, to the extent that such revenues are estimated to be available. The Governor’s budget assumes that the realignment growth revenues will be more than sufficient to cover the partial–year cost of the 5 percent increase during 2013–14, but that realignment revenues will be insufficient in 2014–15, such that $6.3 million of the total cost of the increase would be borne by the General Fund.
State–Local Realignment and the CalWORKs Budget
State–local realignment plays an important role in funding the CalWORKs program. The following section provides some background on state–local realignment, recent changes to realignment, and the ways that these recent changes affect the CalWORKs budget.
Program Changes. In 1991, the state enacted a major change in the state and local government relationship, known as realignment. The 1991 realignment package: (1) transferred several programs from the state to the counties, including indigent health, public health, and mental health programs; (2) changed the way state and county costs are shared for certain social services and health programs (CalWORKs, IHSS, California Children’s Services, and child welfare programs); and (3) increased the sales tax and vehicle license fee (VLF) and dedicated these increased revenues for the increased financial obligations of counties.
Funding Allocations Laws. The realignment legislation established the Local Revenue Fund, and within it a series of accounts and subaccounts, into which dedicated revenues are placed to fund different groups of programs. These included the Social Services subaccount, the Health subaccount, and the Mental Health subaccount. These three subaccounts, along with others added through subsequent legislation, are displayed in Figure 11. A revenue allocation system was also established in which the total amount of revenues allocated to each of these subaccounts in one year becomes the base level of funding in the next year. Growth in revenues between two years is allocated to these subaccounts based on a separate set of statutory formulas. Under these formulas, growth revenues are first allocated to the Caseload subaccount, which provides funding to repay counties for the changes in cost–sharing ratios for programs funded through the Social Services subaccount. Approximately 4 percent of any remaining growth revenues are then allocated to the County Medical Services Program subaccount. All remaining growth revenues, if any, are then allocated to the General Growth subaccount. Prior to the changes discussed immediately below, revenues deposited in the General Growth subaccount were distributed back among the Social Services, Health, and Mental Health subaccounts, with about 8 percent going to the Social Services subaccount, a little more than half going to the Health subaccount, and about 40 percent to the Mental Health subaccount.
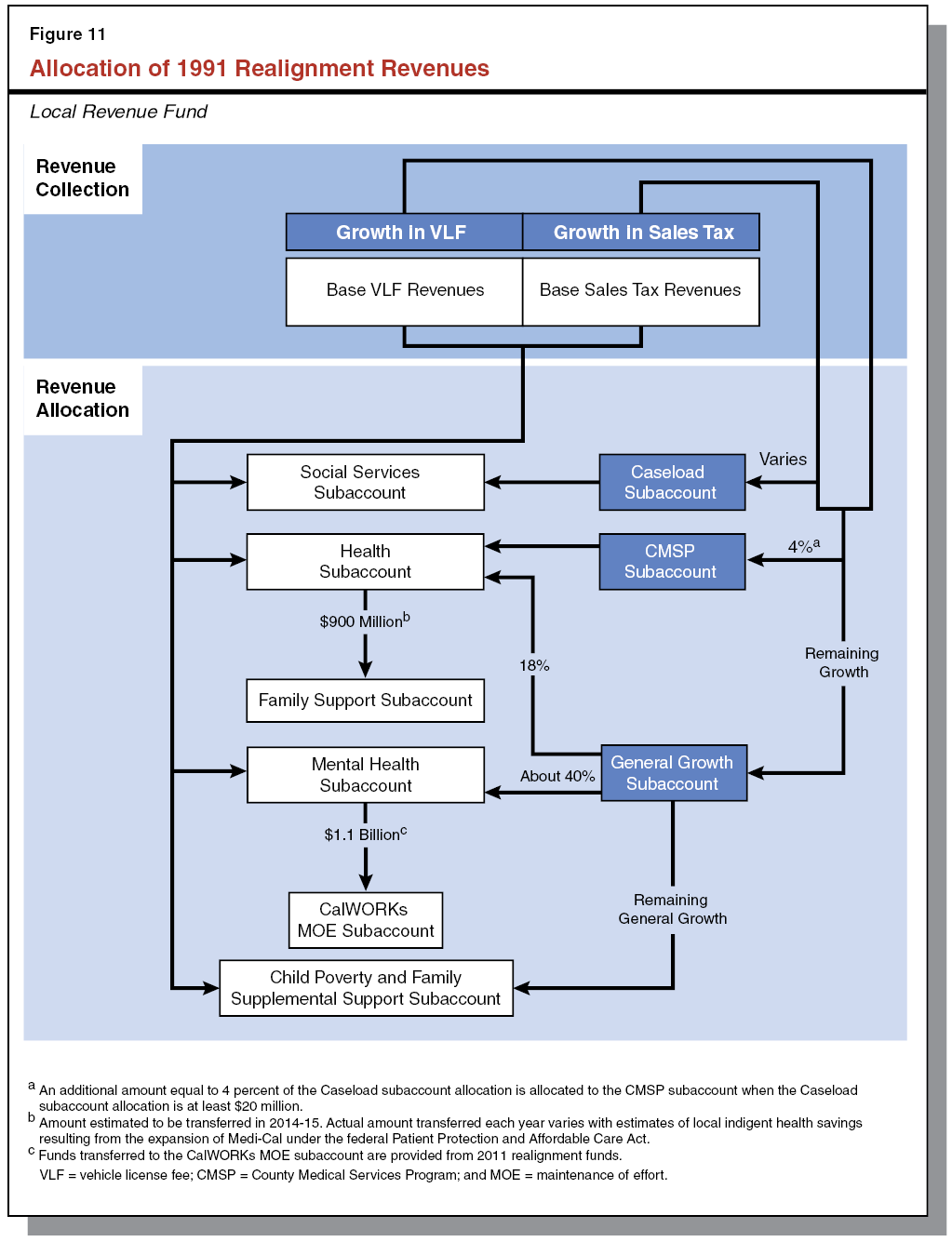
2013–14 Budget Changes to General Growth Allocation. In 2013, budget–related legislation changed the way that growth revenues are allocated. This legislation (1) reduced by roughly two–thirds the amount of General Growth allocated to the Health subaccount by fixing the allocation at 18 percent; (2) eliminated General Growth allocations to the Social Services subaccount; and (3) instead deposited these General Growth revenues in the newly created Child Poverty and Family Supplemental Support subaccount (hereafter referred to as the “Child Poverty subaccount”), which pays for the costs of certain future increases to CalWORKs grants.
Family Support Subaccount. The 2013 legislation additionally created the Family Support subaccount in the Local Revenue Fund. This subaccount receives annual transfers of funds from the Health subaccount in an amount that roughly reflects estimated county indigent health savings resulting from the expansion of Medi–Cal through the ACA. The Family Support subaccount does not receive base or growth allocations from dedicated 1991 realignment revenues. Funds deposited into the Family Support subaccount are used to pay for an increased county share of CalWORKs grant costs, directly offsetting General Fund expenditures.
Program Changes. The Legislature again enacted a major change in the state and local government relationship in 2011 by shifting certain additional state program responsibilities and revenues to local governments (primarily counties). As with the 1991 realignment, the 2011 realignment provided dedicated sales tax and VLF revenues to support increased county fiscal responsibility for various criminal justice, mental health, and health and social services programs. The 2011 realignment resulted in the creation of the Local Revenue Fund 2011, within which numerous accounts were established to distribute dedicated revenues among the realigned programs.
CalWORKs/Mental Health Transfer. Among other things, the 2011 realignment legislation provides counties with revenue from the Local Revenue Fund 2011 for mental health programs, freeing up county mental health funding provided through 1991 realignment. The 2011 realignment legislation requires these freed up 1991 realignment funds to be used to pay for a higher county share of CalWORKs grant costs within each county, offsetting state General Fund costs. This transfer of funds takes place as follows. Each year a specified amount of 2011 realignment revenues is transferred to the Mental Health subaccount in the Local Revenue Fund (1991 realignment). An equal amount of funding is then transferred from the Mental Health subaccount to a new subaccount created in the Local Revenue Fund, called the CalWORKs MOE subaccount. Similar to the Family Support subaccount, the CalWORKs MOE subaccount does not receive base or growth funding from 1991 realignment dedicated revenues.
As a result of the realignment changes discussed above, significant CalWORKs costs that otherwise would be borne by the General Fund are instead paid for with realignment revenues. Specifically, in the Governor’s 2014–15 budget proposal, General Fund spending on CalWORKs is directly offset by (1) $1.1 billion from the CalWORKs MOE subaccount, (2) $900 million from the Family Support subaccount, and (3) $162 million from the Child Poverty subaccount. Taken together, funding from these three realignment sources represent 72 percent of proposed spending on CalWORKs grants from all funds, and 40 percent of proposed spending on the entire CalWORKs program from all funds.
As noted above, budget–related legislation enacted in 2013 created a statutory mechanism by which CalWORKs grant payments will be automatically increased in years when a dedicated revenue stream (consisting of the growth in certain 1991 realignment revenues) is estimated to be sufficient to cover the cost of such an increase, as well as the ongoing cost of all previous increases provided under the mechanism. The 5 percent increase that takes effect in March 2014 is the first increase to be funded with the dedicated revenues. Going forward, additional grant increases will be provided under a process that is laid out in statute. Specifically, the new statutory mechanism requires that the Department of Finance (DOF) regularly perform various calculations to determine the level of grant increase, if any, to be provided each year. Specifically, each January and May, in connection with the release of the Governor’s budget and May Revision, DOF will estimate the amount of dedicated revenues available to support grant increases previously provided under the mechanism. If the available funds exceed the cost of previous increases, DOF will calculate the percentage increase in CalWORKs grants that can be supported by these excess funds. Such an increase would take effect the following October and would be ongoing. If, on the other hand, no excess funds are estimated to be available, no additional grant increase will be provided. In the event that dedicated realignment revenues are estimated to be insufficient to cover the costs of previous grant increases, the previous increases remain in effect and the shortfall will be paid for from the General Fund. In this scenario, no future grant increases would be provided until past increases are fully supported by the dedicated revenues.
Dedicated Revenues Estimated to be Insufficient for Additional Increase in October 2014. As noted previously, DOF estimates that dedicated revenues will be insufficient to fully cover the cost of the 5 percent grant increase in 2014–15. Under the process laid out in statute, this means that no additional grant increase would be provided in October 2014. We find the DOF estimate reasonable; however, we note that the estimated amount of dedicated revenues may be updated as part of the Governor’s May Revision as additional information becomes available to estimate revenues and costs in 2013–14 and 2014–15.
Magnitude of Future Grant Increases Uncertain, but Likely Around 2 Percent Annually. Beyond 2014–15, we estimate that CalWORKs grants could be increased through the statutory mechanism on average by around 2 percent each year. We further estimate that this level of grant increases will largely keep pace with annual increases in the federal poverty guidelines, such that the level of grants as a percentage of federal poverty guidelines may remain relatively constant over the next few years. This estimate is subject to uncertainty, and the amount of grant increase that can be provided in any given year will vary. The three main sources of uncertainty in the estimate are:
- Revenue Growth Projections. As shown in Figure 11, the amount of dedicated funds deposited in the Child Poverty subaccount depends first on the amount of growth in sales tax and VLF revenues deposited in the Local Revenue Fund. Year–over–year changes in these revenue streams are sensitive to economic conditions and are difficult to predict with precision.
- Caseload Subaccount Allocations. As shown in Figure 11, the allocation to the Caseload subaccount is met before distributing remaining growth funds to other accounts, including the Child Poverty subaccount. The application of the methodology for calculating the Caseload subaccount allocations is difficult to predict—allocations to the subaccount have varied significantly, ranging from less than $1 million to more than $100 million in the past decade. As a result, growth in revenues dedicated to provide additional grant increases may not be stable from year to year.
- CalWORKs Caseload Projections. Finally, the size of grant increase that can be paid for with a given amount of dedicated revenues depends on the number of CalWORKs cases that receive assistance. As the caseload continues to decline, a given amount of dedicated revenues can provide a larger percentage grant increase. Fluctuations in the CalWORKs caseload will affect both the cost of previously provided grant increases as well as the size of future grant increases.
Future Grant Increases Sensitive to Economic Conditions. It is important to note that our estimate of the likely magnitude of future grant increases assumes continued steady, moderate growth in the economy. In a hypothetical scenario in which the state economy experiences a moderate recession, growth in dedicated revenues could slow or stop and the costs of grant increases previously provided under the statutory mechanism would increase as more families enter the CalWORKs caseload. This would likely result in a period of years in which no new grant increases would be provided and the General Fund would bear some of the costs of previous grant increases.
Governor Proposes Testing New Approach to Addressing Needs of Families With Multiple Barriers to Employment. The Governor proposes in 2014–15 to begin a demonstration project that would focus on improving outcomes for CalWORKs families that face multiple barriers to employment and are at higher risk of being sanctioned. As noted previously, sanctions occur when adult recipients do not comply with the work requirement. When sanctioned, the adult is excluded from the calculation of the family’s grant, resulting in reduced monthly cash assistance for the family (generally about $125). The administration highlights a few issues relating to families with multiple barriers to employment that motivate the proposal, specifically: (1) children in these families are less likely to access high–quality child care, (2) parents in these families may not be engaged in the educational development of their children, and (3) these families have very limited income and resources and, if sanctioned, receive decreased assistance and are not accessing CalWORKs WTW services that could help address their barriers to employment.
Proposed Pilot Seeks to Address These Issues by Providing Intensive Services for Children and Parents. To enable an evaluation of a potential approach to address these issues, the pilot, beginning in March 2015 and extending through December 2017, would (1) provide intensive case management and services under the existing CalWORKs program intended to address the parents’ barriers to employment and improve work–readiness; (2) provide “stable, high–quality” child care; and (3) require parents to participate in certain parental involvement activities for a number of hours each week with their children at the child care location. The demonstration would involve an estimated 2,000 families in six counties. Participating counties would be selected through a competitive application process. The demonstration would result in General Fund costs of $10 million in 2014–15, and an estimated total General Fund cost of $115 million over three years. This total cost would be made up of roughly $5 million for intensive case management and barrier–removal services, $80 million for high–quality child care, and $31 million for parental involvement activities, with minor offsetting savings assumed to result from higher earnings of pilot participants.
Specific Demonstration Elements to Be Determined by Implementing Counties. While the administration has indicated some of the features it wants included in the demonstration, other features of the intervention to be demonstrated would be determined by the six implementing counties. For example, it appears that counties would largely determine what standard and type of child care providers would be used (for example, counties could partner with State Preschool programs or licensed family child care homes), the format of parental involvement activities, and which families would participate (participation by families would be voluntary). Counties would be expected to consult with local child care organizations, such as Local Child Care and Development Planning Councils, as they develop their applications. A project consultant from DSS would work with selected counties as they plan for implementation. Participating counties would be required to submit regular progress reports and a final report on various outcomes, including child care attendance, participation in parental involvement activities, parent work readiness and employment, and school readiness.
Administration Raises Valid Concerns. In general, we find that the concerns raised by the administration about CalWORKs families facing multiple barriers to employment are valid, particularly when these families are sanctioned. As of November 2013, about 52,000 adults were sanctioned (roughly 16 percent of all adults that could be subject to the work requirement) and the number of sanctions is gradually rising. Given the numerous negative outcomes that are associated with poverty, particularly for children, we believe that focusing on addressing barriers to employment for those families that face the most significant barriers is an appropriate priority for the Legislature. In including access to high–quality child care as a component of the pilot, the administration also raises some important questions about the role of standards–based child care in the CalWORKs program.
Proposed Pilot Intervention Is Complex. The pilot seeks to address multiple concerns using a multifaceted intervention and would examine effects on several outcomes. As noted, the pilot would seek to improve outcomes for both parents and children in families with multiple barriers to employment—specifically, work–readiness and employment outcomes for adults and school–readiness and developmental outcomes for children. The three main components of the intervention might intuitively be expected to affect different sets of outcomes. The first component, intensive case management and barrier–removal services, might be expected to primarily affect adult work–readiness and employment outcomes. The second component, stable, high–quality child care, might be expected to affect both adult and child outcomes, but in different ways. Lack of child care is a common barrier to employment—providing child care makes it possible for adults to participate in other barrier–removal activities and ultimately work. Stable, high–quality child care might also be expected to improve child developmental outcomes. The final component of the intervention, parental involvement activities in the child care setting, might be expected to affect both adult work–readiness outcomes and child developmental outcomes. We address each component of the intervention below.
Intensive Case Management and Barrier Removal Component Overlaps With Existing CalWORKs Services. The proposed pilot would provide intensive case management and barrier removal services to CalWORKs families with multiple barriers to employment. In our view, this aspect of the intervention has the greatest direct relevance to improving parent work–readiness outcomes—one of the fundamental objectives of the CalWORKs program. However, this component also appears to largely overlap with existing CalWORKs services, particularly in light of recent program changes (enacted by the Legislature in 2012 and 2013), some of which are still under implementation. As discussed previously, recent significant changes to the CalWORKs program, including increased flexibility in work rules and early engagement strategies, were intended to increase the capacity of the CalWORKs program to help recipients address barriers to employment. In particular, Family Stabilization Services includes an intensive case management component and provides specialized services to families facing an identified destabilizing situation that would interfere with participation in WTW—a condition that we believe would apply to at least some of the families that the proposed pilot would target. We note that the Legislature has already required an evaluation of the extent to which changes related to the WTW 24–month time limit (including the new work rules) result in addressing barriers to employment more effectively.
CalWORKs Families Already Entitled to Child Care as Means to Improve Adult Employment Outcomes. As part of the CalWORKs program, families that are employed or participating in WTW activities already are guaranteed access to subsidized child care. This pilot therefore would not provide anything substantially different in terms of addressing adult work–readiness and employment outcomes than what is currently available.
State Child Care Programs With Educational Emphasis Currently Exist, but Access Issues for CalWORKs Families Arise. In terms of addressing child outcomes, the pilot could provide a different type of child care program than CalWORKs families currently access. Currently, some child care providers that serve CalWORKs families must meet basic health and safety standards, but are not required to include educational components in their programs. The Governor’s proposal suggests that the child care offered as part of the pilot demonstration would include a greater emphasis on “quality,” which would appear to feature a stronger educational focus. (Increasingly, research indicates that early childhood programs that focus on education can have positive impacts on children’s outcomes.) The state, however, already funds several child care programs that have considerable educational components, suggesting the state does not need to create a new pilot program to demonstrate the impacts of such programs. CalWORKs families historically have had a difficult time accessing these programs because of the way the state structures services—an important policy question for the Legislature to consider.
Little Evidence to Suggest That Parental Involvement Activities Would Directly Improve Employment Outcomes. In our view, the parental involvement component is the primary aspect of the pilot relating to adult outcomes that appears to both exceed the services generally available through CalWORKs and present an opportunity to test a new strategy through a demonstration. Little is known about the effect of parental involvement activities on adult work–readiness or employment outcomes. While we acknowledge the possibility that such activities could affect these adult outcomes, we think this effect would be very indirect and that the potential value added from demonstrating the impact of parental involvement on work readiness does not justify the pilot.
Parental Involvement as Means to Improve Child Outcomes Outside CalWORKs Program Focus. The potential effect of parental involvement on child outcomes would be more direct. Providing parental involvement activities in a child care setting is an approach that could be worth investigating. However, we do not believe the added value of investigating the impact of parental involvement on child outcomes would justify the proposed pilot either, given the CalWORKs program’s focus on assisting parents to become work ready as a means to reduce child poverty.
On Balance, Recommend Rejecting Governor’s Proposal to Create New Pilot Program. While the Governor raises valid concerns about CalWORKs families with multiple barriers to employment, we have several issues with the proposal. Specifically, in our view (1) certain aspects of the proposed pilot would provide services that largely duplicate those already available in the CalWORKs program, particularly given recent significant statutory changes that are still partially under implementation; (2) the state currently funds child care programs with an educational focus for similar low–income children, so a new pilot is not necessary to demonstrate the impact of these programs on child outcomes; and (3) the potential added value of testing the impact of parental involvement activities is not sufficiently compelling to justify a CalWORKs pilot, particularly given the pilot’s substantial cost ($115 million over three years).
Recommend Legislature Explore Ways to Address Inconsistencies in Child Care Standards. The proposed pilot does not directly address challenges faced by CalWORKs families in accessing educationally focused child care programs funded by the state, but this issue does merit legislative consideration. We recommend the Legislature explore alternative ways to provide CalWORKs families more access to child care programs with an educational focus.
State Hearings Division (SHD). The mission of the SHDa division of DSS—is to resolve disputes of applicants and recipients of various health and social services in an impartial, independent, and timely manner, ensuring that due process is met. Appeal claimants can dispute how an application or benefits/services are/were handled for various programs, including Medi–Cal, CalWORKs, CalFresh, and IHSS.
Federal and state law, along with judicial decisions, require DSS to provide claimants with a timely due process in the adjudication of claims. To comply with the timeliness standards, SHD is generally required to adjudicate claims within 90 days from when a claimant requests an appeal (within 60 days for CalFresh claims). According to a court decision, the state is assessed financial penalties to the benefit of the claimants if the timeliness standards are not met by DSS. Penalties vary by program and are based on complex penalty formulas that can change from month to month depending on whether SHD adheres to a 95 percent timeliness standard. In January 2014, the penalty rate per day of a late decision was $82.50 for Medi–Cal, $55 for CalWORKs, $12.50 for CalFresh, and $82.50 for IHSS. Penalties levied on the state for untimely SHD adjudication in 2012–13 totaled $5.2 million.
ACA–Related Growth in Appeals Caseload. In order to make health care coverage more accessible and affordable, the ACA establishes entities called Health Benefit Exchanges. Through these exchanges, individuals and small businesses are able to obtain information about health coverage and purchase coverage. The California Health Benefit Exchange (also known as Covered California) built a web–based portal designed to be a streamlined resource from which individuals and small businesses are now able to research, compare, check their eligibility for, and purchase coverage.
Covered California has designated SHD to adjudicate all appeal requests related to various of its determinations, including those regarding Advanced Premium Tax Credits and Cost–Sharing Reductions, Modified Adjusted Gross Income (MAGI) Medi–Cal, and Small Business Health Option Programs. The SHD currently provides the appeal function for the Medi–Cal caseload, which will also increase to cover new populations and additional enrollees under the ACA. The implementation of the ACA is projected to increase in 2014–15 SHD’s overall caseload by 53 percent above 2012–13, an equivalent of over 9,400 appeals.
State Hearings System (SHS). The SHD is supported—technology wise—by an antiquated mainframe application and 21 “ad–hoc” applications to track, schedule, and manage appeal claims received from claimants in all 58 counties. Collectively, these systems are known as the SHS. According to DSS, the SHS does not meet existing SHD needs and will not be able to support the increased caseload associated with ACA implementation.
Since the base technology for the SHS was built over 30 years ago, business needs of the SHD have changed so that the system can no longer address new information tracking requirements, information security challenges, additional reporting needs, and other changes. Although these requirements have been addressed for the time being through the development of the 21 ad–hoc systems, these applications are largely manual and are not a sustainable solution to SHD’s changing business needs.
Office of Systems Integration (OSI). The OSI—an office of the Health and Human Services Secretary—was established in 2005 to provide project management, oversight, procurement, and support services to a portfolio of large, complex, and high criticality health and human services IT projects. Since its inception, OSI has developed a track record of successfully managing and deploying mission critical IT systems that support health and human services programs at the state, federal, and local level.
The Governor’s budget includes a proposal to address the growth in SHD caseload associated with the ACA and the deficiencies of the SHS, at a total cost of $11.1 million ($1.8 million General Fund) in 2014–15. The proposal includes two components:
- Staff Resources to Address ACA Caseload Growth. The Governor proposes 63 two–year limited–term positions to address the addition of the ACA caseload to SHD. The proposal requests a mixture of administrative law judges (39 positions) and support staff (24 positions).
- Staff Resources for Appeals Case Management System (ACMS). The Governor also proposes 11 three–and–one–half–year or four–year limited–term positions to develop and begin to implement and maintain the new ACMS over a four–year period. The ACMS project is intended to replace the SHS with a modernized case management database that would consolidate intake, scheduling, and reporting functions. The ACMS project is estimated to cost $12.3 million and expected to be complete in March of 2017. The proposal also requests $130,000 in expenditure authority for one one–year limited–term position at OSI to provide procurement and acquisition expertise to DSS on the ACMS project.
ACA Caseload Projections Appear Reasonable. The SHD’s standard caseload assumption is that 2.5 percent of applicants of programs overall for which it performs an appeals function will request a state hearing, while 25 percent of hearing requests will result in a full hearing. The SHD applies this standard assumption in estimating the impact of ACA on its caseload. This appears reasonable. However, given the significant uncertainty about the actual impact of the ACA on SHD’s caseload, it is appropriate for the requested additional staff to address ACA caseload be limited–term, as has been proposed by the Governor.
New ACA Workload Cannot Be Absorbed by SHD. The SHD experienced a growth in penalties assessed against it for not meeting timeliness standards over the last five years due to a convergence of trends—a 26 percent growth in caseload over the past five years and a loss of experienced staff due to a high rate of retirements. Given the challenges SHD has had complying with timeliness standards for existing caseload, the SHD is unlikely to absorb the additional ACA–related caseload without jeopardizing timely due process and increasing the state’s penalty exposure.
Proposed Staffing Model Fosters Efficiencies at SHD. In addition to increasing the number of administrative law judges, the proposal also depends heavily on support staff to address the ACA–related caseload. Support staff are critical to reducing the number of cases that go from hearing requests to actual hearings by performing prehearing functions, including reviewing all hearing requests, preparing administrative dismissals of invalid hearing requests, confirming the need for a language interpreter, contacting claimants and authorized representatives to assure hearing readiness of case, assisting in the transmission and exchange of hearing documents, and preparing postponement and withdrawal of cases as appropriate. Collectively, the support positions can increase efficiencies attained from assessing the readiness of cases, thereby reducing administrative law judges’ time spent on hearing cases.
Extensive SHS Deficiencies Compromise SHD. The SHD determined that the SHS did not have the capacity to manage the added volume created by the ACA caseload. To accommodate the new caseload, SHD built a duplicative skeleton SHS to process ACA–related appeals. This solution is not an efficient response and does not represent a long–term solution. The SHS also has a series of deficiencies that compromise its ability to efficiently manage existing caseload. The proposed ACMS project would create a single case management database that would consolidate intake, scheduling, and reporting functions. The consolidation of the SHS is intended to streamline the workload that is currently highly dependent on inefficient manual processes.
Delaying or Rejecting Request Jeopardizes Timeliness of Adjudication and Increases State’s Penalty Exposure. Given the safety–net nature of the programs adjudicated through the SHD, timely due process for claimants is critical for effective and appropriate support of children, the aged, blind, disabled, and their families. Without the staffing resources requested and efficiencies created by ACMS development, SHD would face significant challenges addressing a claims backlog while simultaneously providing due process to the new ACA–related claimants.
We recommend approval of the Governor’s proposal for 74 limited–term positions and $11.1 million to address the growth in caseload associated with the ACA and the replacement of SHS with ACMS. This approach better positions SHD to provide timely due process for additional claimants as a result of ACA implementation and reduces the state’s penalty exposure through the development of a more efficient automated case management system to support SHD. It is particularly appropriate that the added staff related to ACA–driven caseload be limited term, as proposed by the Governor, given uncertainty about the extent of this new workload as well as the impacts of adding the requested staff. At the end of the limited term, ongoing ACA–related staffing requirements can be reevaluated, by considering what had been achieved in terms of decreased penalty exposure and compliance with timeliness standards as a result of the addition of the requested limited–term staffing.
Overview of DDS. The Lanterman Developmental Disabilities Services Act of 1969 (known as the Lanterman Act) forms the basis of the state’s commitment to provide individuals with developmental disabilities with a variety of services and supports, which are overseen by DDS. The Lanterman Act defines a developmental disability as a “substantial disability” that starts before age 18 and is expected to continue indefinitely. The developmental disabilities for which an individual may be eligible to receive services under the Lanterman Act include: cerebral palsy, epilepsy, autism, intellectual disabilities, and other conditions closely related to intellectual disabilities that require similar treatment (such as a traumatic brain injury). The department works to ensure that individuals with developmental disabilities, regardless of age, have access to services and supports that sufficiently meet their needs, preferences, and goals in the least restrictive setting. Unlike most other public social services or medical services programs, services for the developmentally disabled are generally provided without any requirements that recipients demonstrate that they or their families do not have the financial means to pay for the services themselves. The department administers two main programs, described in detail below.
Community Services Program. Community–based services are coordinated through 21 nonprofit organizations known as regional centers (RCs), which provide diagnosis, assess eligibility, develop individual program plans for each consumer, and help consumers coordinate and access the services they need. The DDS provides RCs with an operations budget in order to conduct these activities. The DDS also provides RCs with a budget to purchase services from vendors for an estimated 265,709 consumers in 2013–14. These services can include day programs, transportation, residential care provided by community care facilities, and support services that assist individuals to live in the community. The RCs purchase more than 100 different services on behalf of consumers. As the payer of last resort, RCs generally only pay for services if an individual does not have private insurance or if the RC cannot refer an individual to so–called “generic” services such as other state–administered health and human services programs for low–income persons or services that are generally provided at the local level by counties, cities, school districts, or other agencies. We note that the majority of consumers receiving services through the Community Services Program are enrolled in Medi–Cal, California’s Medicaid program. (For a description of the Medi–Cal Program, please see the “Medi–Cal” section in The 2014–15 Budget: Analysis of the Health Budget.)
More than 99 percent of DDS consumers receive services under the Community Services Program. These consumers live with their parents or other relatives, in their own houses or apartments, or in residential facilities or group homes designed to meet their needs. Less than 1 percent live in Developmental Centers (DCs), discussed below.
During a period of recent budget deficits, the Legislature enacted numerous DDS budget reductions and cost savings measures to yield General Fund savings, such as rate changes and provider payment reductions for RC vendors, service changes, and reliance on increased federal funding. The provider payment reductions experienced by RC vendors—including the 3 percent reduction in 2009–10, the 4.25 percent reduction in both 2010–11 and 2011–12, and the 1.25 percent reduction in 2012–13—have expired with no new provider payment reductions proposed for 2014–15. However, rates paid to providers established by statute or by the department have generally been frozen since 2003–04. Rates negotiated by the RCs for new providers were limited beginning in 2008 to no higher than the median rate for that service. Certain RC programs and services have experienced further ongoing reductions. In 2008–09, the Supported Employment Program provider rates were cut by 10 percent (after having been increased by 24 percent in 2006–07) and remain at that level with no restorations proposed for 2014–15. In 2009–10, a number of ongoing reductions were made to the Early Start program, which provides services to infants and toddlers under the age of three who have a developmental disability (and prior to 2009–10, to children who were at–risk for a developmental disability). Also in 2009–10, the DDS suspended the availability of certain services, including social/recreation activities, camping services and associated travel, educational services for school–aged children, and certain nonmedical therapies. The Governor’s budget does not propose any restorations for the Early Start program or for the suspended services.
DCs Program. The DDS operates four 24–hour facilities known as DCs—Fairview DC in Orange County, Lanterman DC in Los Angeles County, Porterville DC in Tulare County, and Sonoma DC in Sonoma County—and one smaller leased community facility (Canyon Springs in Riverside County), which together provide 24–hour care and supervision to approximately 1,300 consumers in 2013–14. Each DC is licensed by the Department of Public Health (DPH), and certified by DPH on behalf of CMS, as Skilled Nursing Facilities, Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICF/IID), and General Acute Care hospitals.
The DCs are licensed and certified to provide a broad array of services based on each resident’s individual program plan, such as nursing services, assistance with activities of daily living, specialized rehabilitative services, individualized dietary services, and vocational or other day programs outside of the residence. The DCs must be certified in order to receive federal Medicaid funding. The vast majority of DC residents are enrolled in Medi–Cal. Generally, for Medi–Cal enrollees living in DCs, the state bears roughly half the costs of their care and the federal government bears the remainder. Over the past 15 years, the DCs have faced a history of problems identified by oversight entities, such as DPH and the United States Department of Justice, including inadequate care, insufficient staffing, and inadequate reporting and investigation of instances of abuse and neglect. For more background on the history of problems identified at DCs, please refer to the DDS analysis in The 2013–14 Budget: Analysis of the Health and Human Services Budget.
Task Force Provides Framework for Long–Term Future of DCs. While the Governor’s budget (discussed below) addresses the immediate funding needs of the DCs, a task force convened by the administration during the seven–month period from June to December 2013 released a plan on January 13, 2014, for the long–term future of DCs. The task force included consumers, family members of DC residents, RC directors, consumer rights advocates, labor union members, community service providers, and staff from DDS. The plan released by the task force on the future of DCs recognizes the need to reevaluate the role of DCs in light of the historical trend of individuals with developmental disabilities moving out of institutional settings and into the community. We note that budget–related legislation enacted in 2012–13 imposed a moratorium on new admissions to DCs, with exceptions for individuals involved in the criminal justice system and consumers in an acute crisis needing short–term stabilization. The plan released by the task force recognizes the varying needs of existing DC residents and makes recommendations for improving community services and supports, while retaining institutional facilities for individuals who are in acute crisis or involved in the criminal justice system.
Overall Budget Proposal. The budget proposes $5.2 billion (all funds) for DDS in 2014–15, which is a 4.5 percent net increase over estimated revised expenditures in 2013–14. General Fund expenditures for 2014–15 are proposed at $2.9 billion, a net increase of $132 million, or 4.7 percent, over estimated revised expenditures in 2013–14. This net increase in total expenditures generally reflects increases in the budget for the Community Services Program, partially offset by decreasing costs in the DCs Program budget.
Community Services Program Budget Proposal. The budget proposes $4.7 billion (all funds) for the Community Services Program in 2014–15, which is a 5.7 percent net increase over estimated revised expenditures in 2013–14. Of this total, $580 million is proposed for RC operations expenditures and the remainder of $4.1 billion is for the purchase of services from RC vendors. General Fund expenditures for the Community Services Program in 2014–15 are proposed at $2.6 billion, a net increase of $162 million, or 6.5 percent, above the estimated revised expenditures in 2013–14. This net increase mainly reflects caseload growth and greater utilization of services, along with rising costs for vendors as a result of the state–mandated increase in the hourly minimum wage and recent federal labor regulations impacting home care workers. The 2014–15 Community Services Program budget plan reflects the following year–over–year budget changes:
- Caseload Growth and Greater Utilization of Services. Increase of $139 million ($83 million General Fund) because of caseload growth and greater utilization of services.
- State–Mandated Hourly Minimum Wage Increase From $8 to $9. Increase of $110 million ($69 million General Fund) for increasing the rates paid to certain RC vendors that employ workers currently earning less than $9 per hour. Chapter 351, Statutes of 2013 (AB 10, Alejo), will increase the state–mandated hourly minimum wage from $8 to $9 beginning July 1, 2014. We analyze this component of the Governor’s proposal later in this section.
- Federal Labor Regulations. Increase of $8 million ($4 million General Fund) in response to recent federal labor regulations to take effect January 1, 2015. Please refer to the “Human Services Compliance With Federal Labor Regulations” analysis in this report for more detail on, and our analysis of, this proposal.
- Decrease in RC Purchase of Services Due to Medi–Cal Benefit Restorations. Decrease of $3 million General Fund because of the restoration of certain Medi–Cal benefits, including the full restoration of enteral nutrition coverage and the partial restoration of adult dental services.
DCs Program Budget Proposal. The budget proposes $526 million (all funds) for the DCs Program in 2014–15, which is a 5.4 percent net decrease below estimated revised expenditures in 2013–14. General Fund expenditures for 2014–15 are proposed at $275 million, a net decrease of $31 million, or 10 percent, below estimated revised expenditures in 2013–14. This net decrease in the DCs Program budget reflects the following year–over–year budget changes.
- Staffing Reductions Due to Decreased Resident Population. Decrease of $13 million ($7 million General Fund) because of staffing reductions as the population of the DCs declines (these staffing reductions exclude Lanterman DC, which is discussed separately below).
- Completion of Lanterman DC Closure. Net decrease of $23 million ($12 million General Fund) related to the ongoing closure of Lanterman DC. The net decrease takes into account costs for closure and post–closure activities, which are more than offset by savings from staff reductions as the resident population is assumed to decline to zero by December 31, 2014.
- Restoration of Lost Federal Funds at Sonoma DC. Decrease of $16 million General Fund (increase of $16 million in federal funds) assumed in 2014–15 because of the expected restoration of previously lost federal funds as a result of the implementation of the improvement plan, discussed below, for four decertified ICF living units at Sonoma DC.
- Deferred Maintenance. Increase of $10 million General Fund for deferred maintenance projects in the DCs budget. It is our understanding that the funds will be used to replace boilers at Sonoma DC and Porterville DC and retrofit boilers at Fairview DC to ensure compliance with emissions regulations established by local Air Quality Management Districts. The funding is part of the Governor’s proposal to spend $100 million General Fund statewide on deferred maintenance projects in 2014–15.
- Sonoma DC Improvement Plan. Increase of $2 million ($1 million General Fund) to fund improvements needed at Sonoma DC to ensure compliance with federal certification requirements for ICF living units. We note that DDS requested—and the Joint Legislative Budget Committee (JLBC) approved—$7 million ($4 million General Fund) in 2013–14 to begin making needed improvements at Sonoma DC. We analyze this component of the Governor’s proposal later in this section.
Headquarters Budget Proposal. The budget proposes $41 million ($26 million General Fund) for headquarters operations expenditures, which is a 1.8 percent increase above the revised estimate of expenditures in 2013–14.
RC Caseload Has Steadily Grown in Recent Years. Between 2006–07 and 2013–14, the RC caseload is projected to grow from 211,180 to an estimated 265,709—an average annual growth rate of 3.3 percent. The caseload trend is shown in Figure 12.
Figure 12
Regional Center Caseload Growth Trend
|
|
Average Annual Caseload
|
Increase From Prior Year
|
|
Consumers
|
Percent
|
|
2006–07
|
211,180
|
|
|
|
2007–08
|
221,069
|
9,889
|
4.7%
|
|
2008–09
|
229,675
|
8,606
|
3.9
|
|
2009–10
|
236,858
|
7,183
|
3.1
|
|
2010–11
|
242,977
|
6,119
|
2.6
|
|
2011–12
|
249,532
|
6,555
|
2.7
|
|
2012–13
|
256,224
|
6,692
|
2.7
|
|
2013–14a
|
265,709
|
9,485
|
3.7
|
|
Average
|
239,153
|
7,507
|
3.3
|
RC Caseload Estimate Appears Reasonable. The Governor’s budget assumes the RC caseload in 2014–15 will be 273,643, an increase of 7,934 consumers, or 3 percent, compared to the most recent estimate of the 2013–14 caseload. Based upon our review of recent RC caseload data, we find the administration’s caseload estimate to be reasonable. If we receive additional information that causes us to change our overall assessment, we will provide the Legislature with an updated analysis.
DC Caseload Has Steadily Declined in Recent Years. Between 2006–07 and 2013–14, the DC population has declined from 2,877 to an estimated 1,333—an average annual decline of 10.4 percent. This decline in the DC population is mostly attributable to the closure of DCs and the corresponding transition of consumers to community–based settings, which is consistent with federal and state policy to provide services to developmentally disabled individuals in the least restrictive setting. In 2009, Agnews DC in Santa Clara County was closed and Lanterman DC is scheduled to close by December 2014. In addition, the moratorium on new admissions to DCs established in 2012–13 has contributed to a decline in the DC caseload.
DC Caseload Estimate Appears Reasonable. The Governor’s budget assumes the DC caseload in 2014–15 will be 1,110, a decrease of 223 consumers, or 16.7 percent, compared to the most recent estimate of the 2013–14 caseload. This caseload estimate includes the population residing in Lanterman DC—which is expected to decline to zero consumers by December 31, 2014. We note that 22 consumers are expected to reside in Lanterman DC at the beginning of 2014–15. The ability of DDS to transition all Lanterman DC consumers to community–based settings by December 31, 2014 assumes the successful execution of transition plans developed for Lanterman DC residents. Based upon our review of recent DC caseload data, we find the administration’s caseload estimate to be reasonable. If we receive additional information that causes us to change our overall assessment, we will provide the Legislature with an updated analysis.
Because of the structure of the Community Services Program, in which RCs purchase services from vendors on behalf of consumers, the DDS does not maintain data on the number of workers employed by RC vendors and their wages. However, since the state–mandated hourly minimum wage is scheduled to increase from $8 to $9 beginning July 1, 2014, the Governor’s budget proposes to increase the rates paid to certain vendors who employ workers who currently earn less than $9 per hour. Because DDS does not have data on the workers who will be impacted by this increase, the Governor’s budget includes a proposal for budget–related legislation that would establish a process whereby most vendors could provide documentation to either DDS or the RC on the number of employees earning less than $9 per hour in order to receive an appropriate rate increase. The Governor’s budget assumes that seven types of RC vendors will receive rate increases—these vendors include community care facilities, day programs, habilitation services, transportation services, support services, in–home respite, and out–of–home respite—at an estimated cost of $110 million ($69 million General Fund) in 2014–15. Because DDS intends to provide rate increases to vendors that are impacted by the minimum wage increase and because there is no existing data available on impacted workers, the exact cost of funding the minimum wage increase is uncertain. We note that Supported Employment Program providers would not receive a rate increase, nor have the ability to apply for a rate adjustment, based on the administration’s current approach, and we are still evaluating whether this is appropriate.
Analyst’s Recommendation. We recommend the Legislature approve the Governor’s budget proposal to provide $110 million for DDS to comply with new minimum wage requirements, as we find it to be a reasonable approach for addressing the need to increase rates for certain vendors that employ workers who currently earn less than $9 per hour. We also agree that, in the absence of data demonstrating the exact number of impacted workers, the administration’s flexible approach of allowing impacted vendors to seek a rate adjustment is appropriate. However, because we are unsure of the exact cost of funding the minimum wage increase, we further recommend that the Legislature create a separate appropriation to fund this expenditure. The separate appropriation would ensure that the funds are used for the intended purpose of vendors’ payroll costs associated with the new minimum wage.
The state’s DCs undergo annual recertification surveys conducted by DPH to ensure that the facilities meet federal requirements for receipt of federal Medicaid funds. A July 2012 recertification survey conducted by DPH identified problems impacting residents’ health and safety at Sonoma DC. In December 2012, DPH announced it was taking significant action to protect Sonoma DC residents due to the identified deficient practices at the DC. In January 2013, DDS voluntarily withdrew four ICF living units at Sonoma DC from federal certification, leading to the loss of federal Medicaid funds in the amount of $16 million in 2013–14 (partial–year effect for 2012–13 was $7 million). The lost federal funds have been backfilled by an equivalent amount of General Fund to ensure that DC residents continue to receive services.
During annual recertification surveys conducted by DPH in 2013, ICF units at Fairview, Porterville, and Lanterman DCs were also found to be out of compliance with various federal requirements. The facilities were found to have some common deficiencies, including inconsistent treatment plans, residents who were not adequately protected from abuse or harm, and inconsistent implementation of policies generally related to clients’ health and safety and client rights. Fairview and Porterville DCs were found to have additional deficiencies unique to each facility.
Generally, when a DC is found to be out of compliance with federal certification requirements, it must implement a program improvement plan that involves several steps—(1) an independent review conducted by outside experts who develop an action plan that identifies the “root cause” of deficiencies and proposes action items to prevent the deficiencies, (2) DPH approval of the action plan and implementation by the facility, and (3) a recertification survey by DPH.
Current–Year Funding Augmentations for Sonoma DC Approved by Legislature. In order to attain federal certification for the four decertified ICF living units, Sonoma DC must undertake the three–step program improvement plan process described above. In January 2014, the DDS requested—and the JLBC approved—$7 million ($4 million General Fund) for the unanticipated costs of implementing the action plan for Sonoma DC beginning in 2013–14. The funding approved by the JLBC for the remainder of 2013–14 will enable Sonoma DC to make the following improvements.
- Augment Staffing Levels for Licensed Medical Professionals and Other Staff Positions at Sonoma DC. Increase of $4 million ($2.1 million General Fund) to augment staffing levels for licensed medical professionals and other staff including: psychiatrists; direct care staff, such as registered nurses, licensed vocational nurses, and psychiatric technicians; rehabilitation, occupational, and physical therapists; speech pathologists; office technicians; and independent program coordinators. The augmentation provides for 112 new positions (which includes 8 positions secured through contracts).
- Provide Training for All ICF Staff at Sonoma DC. Increase of $2.7 million ($1.5 million General Fund) to provide a one–time enhanced training to all ICF staff and to pay overtime costs to backfill direct care staff attending training.
- Open New ICF Unit at Sonoma DC. Increase of $400,000 ($200,000 General Fund) to open a new ICF living unit to decrease the population in existing ICF units and reduce aggressive incidents between clients. The opening of a new ICF unit does not require a capital outlay expenditure. Some of the additional direct care staff positions will staff the new ICF unit.
- Purchase Three Additional Wheelchair–Accessible Vehicles. Increase of $100,000 General Fund to purchase three additional wheelchair–accessible vehicles so each ICF living unit at Sonoma DC has access to transportation for community outings or on–campus transport.
Governor’s Budget Proposes to Continue Funding Improvements at Sonoma DC to Ensure Restoration of Federal Funds. The Governor’s 2014–15 budget proposal requests $9 million ($5 million General Fund) for the full–year, ongoing cost of implementing the action plan for Sonoma DC. This full–year, ongoing cost mostly funds staffing at the augmented level approved by the Legislature as a current–year adjustment. The Governor’s budget indicates that the earliest possible date for the four decertified ICF living units at Sonoma DC to attain certification is March 30, 2014. Given this date, the Governor’s budget assumes that lost federal funds in the amount of $16 million will be restored beginning July 1, 2014.
Analyst’s Recommendation. Based upon our review of the proposal to make improvements at Sonoma DC, it appears reasonable for the budget to assume that the federal funding will be restored beginning July 1, 2014. We find the 2014–15 budget request to be reasonable and appropriate, as the funding will enable DDS to make improvements at Sonoma DC that are needed to restore federal funding and comply with federal certification requirements.
To ensure legislative oversight of the implementation of the action plan, we recommend the Legislature require the department to report at budget hearings on its progress in implementing the changes at Sonoma DC, with particular attention to the status of filling needed positions for licensed medical professionals and other staff.
Fairview, Porterville, and Lanterman DCs Will Retain Federal Funding During Improvement Process. The DPH and DDS have reached agreements as of January 16, 2014, that will enable the Fairview, Porterville, and Lanterman DCs to retain federal Medicaid funding while the facilities make improvements to meet federal standards. Like Sonoma DC, the Fairview and Porterville DCs will implement improvements based on an action plan specific to the DC—to be developed through an independent review by outside experts on the root cause of deficiencies and action items to prevent the deficiencies. For Lanterman DC, which DDS plans to close by December 2014, an independent monitor will oversee the facility’s closure to ensure the health and safety of the remaining consumers. The specific plan for each of the three DCs will dictate the amount of state funding, if any, needed to make improvements to avoid federal decertification and the loss of federal Medicaid funds. Based on our conversations with DDS, the timing for the completion of a specific plan for each of the three DCs is uncertain. Additional state resources may be required to make improvements at each of the three DCs.
The CHHSA—headed by the office of the Secretary of CHHSA—is the largest state agency, with direct oversight of 13 departments and other entities. With an estimated cost of $1.8 billion to complete projects in progress, the CHHSA also has one of the largest and most complex IT project portfolios in the state. Some of the largest projects include (1) the Los Angeles Eligibility, Automated Determination, Evaluation, and Reporting Replacement System—which replaces an existing automated welfare system, (2) California Medicaid Management Information System—which processes payments to Medi–Cal fee–for–service providers, and (3) Child Welfare Services–New System—which modernizes Child Welfare Services’ case management system.
The Office of the Agency Information Officer (OAIO). Legislation enacted in 2007 vested broad responsibilities to improve the governance and strategic planning of IT with an agency Chief Information Officer. The CHHSA’s Chief Information Officer was established as the OAIO—an office of the Secretary. It is charged with (1) overseeing the IT portfolio of CHHSA departments, (2) ensuring that all CHHSA departments are in compliance with state IT policy, and (3) developing an “enterprise architecture”—the organization of IT infrastructure to reflect integration, consolidation, and standardization of requirements. Historically, the OAIO has not had dedicated staff; instead, its functions have been performed primarily through the sporadic redirection of staff from various CHHSA departments.
The OSI. The OSI—also an office of the Secretary—was established in 2005 to provide—under contract with CHHSA departments—project management, oversight, procurement, and support services to a portfolio of large, complex, and high criticality health and human services IT projects. (Outside CHHSA, departments are responsible for their own project management, unless project management services are contracted out to a third–party vendor.) Although there is collaboration between OAIO and OSI, typically OSI begins its project management role once the strategic planning is competed by OAIO. Since its inception, OSI has developed a track record of successfully managing and deploying mission critical IT systems that support health and human services programs at the state, federal, and local level. Given OSI expertise, departments inside and outside CHHSA have requested OSI’s technical assistance for their IT projects. In other cases, at–risk projects have been referred to OSI by CHHSA or the Department of Technology. The OSI’s funding and staffing is project–specific. Therefore, OSI does not have the ability to redirect staff resources to provide technical assistance to projects not under contract with OSI. Rather, it needs to obtain reimbursement and position authority on a project–by–project basis. The OSI indicates that given barriers to securing reimbursement authority, discussed further below, OSI has not accommodated requests or referrals for technical assistance in the past.
The Governor’s budget proposes various programs intended to bolster CHHSA’s ability to strategically plan IT projects under the agency. Specifically, the proposal requests three permanent positions and $431,000 in reimbursement authority to establish three agency–wide programs located in OAIO.
- Strategic Enterprise Architecture Program. The strategic enterprise architecture program would set the IT strategic vision for CHHSA and ensure proposed IT projects under the agency align with CHHSA’s strategic vision. The program would also foster the development of flexible technologies that facilitate information sharing across CHHSA departments. In other words, the building of systems with similar structures so they can communicate with each other is encouraged.
- Governance Program. A committee established through the governance program would be responsible for reviewing IT projects to identify opportunities for multiple departments with similar IT needs to leverage a single system. The committee would encourage collaboration and partnership across departments to facilitate data sharing and adoption of common standards and solutions across CHHSA.
- Project Assessment Program. The project assessment program would advise and collaborate with CHHSA departments during the early initiation and planning phases of a project to ensure that best practices are incorporated into project plans. The OAIO would also assess if projects are appropriately resourced and if timelines and cost projections are accurate.
Collectively, these programs are intended to enhance CHHSA’s ability to provide oversight and advisory services to CHHSA departments so that projects are best positioned to succeed. While one of the requested permanent positions would focus on strategic enterprise architecture, the remaining two positions would share responsibility for governance and program assessment, with one position taking a management role while the other position taking a staff analyst role. The requested positions would replace the redirected staff used sporadically in the past.
Provisional Language to Strengthen OSI’s Ability to Share Timely Expertise With IT Projects Statewide. The Governor’s budget also proposes provisional budget language that is intended to expedite OSI’s ability to provide as–needed technical assistance to departments inside and outside CHHSA. Specifically, the provisional language would exempt augmentations to reimbursements for OSI from Section 28.50 of the annual budget act—which provides a legislative review process for authorizing mid–fiscal year increases in reimbursement authority above $200,000—and instead only require the Director of Finance to provide written notice to the Legislature within 30 days when the increase to reimbursements exceeds $200,000. This would allow OSI to receive reimbursements and administratively establish the positions necessary to provide the technical assistance to the requesting or referred department as soon as the request or referral for its assistance is initiated. If ongoing reimbursement and position authority were necessary, it would be requested through the annual budget process.
Limited Capacity for IT Strategic Planning Currently Exists. The OAIO’s historical reliance on staff sporadically redirected from other CHHSA departments to address its staffing requirements has resulted in it having limited success in ensuring CHHSA–wide coordination and strategic planning of IT projects. The OAIO currently lacks the structure for comprehensive evaluation and prioritization of its IT investments. There is also no formal governance structure in place to review and assess whether multiple departments are pursuing duplicative solutions—such as when multiple departments each develop their own case management system rather than leveraging a single case management system. Pursuing duplicative solutions does not support the most cost–effective or efficient approach to technology development. Ultimately, undedicated and unstable sources of funding results in little ability to ensure IT investments are maximized so that systems are interoperable (can communicate with each other) and easily leveraged across multiple CHHSA departments with common technology needs. The ability of OAIO to fulfill its mission would be strengthened through dedicated full–time staff—a component of the Governor’s budget proposal.
Strategic Planning Could Eliminate Duplicative Projects, Improve System Interoperability, and Lead to Enhanced “Customer” Service. Once implemented, duplicative technology systems often do not align well and introduce program inefficiencies and interoperability issues, including systems being unable to share data. Collectively, the strategic enterprise architecture and governance programs proposed by the Governor’s budget could help eliminate duplicative projects by coordinating IT investments and aligning projects towards a CHHSA strategic vision. The enhanced interoperability of technology systems would create more flexible architecture that enables information sharing. A flexible architecture in turn could significantly improve the experience of Californians serviced by the programs administered through CHHSA departments. For example, in a fully interoperable environment, a recipient of multiple CHHSA administered benefits could provide a change of address notice to a single program that would then be shared with the other programs, instead of providing the change of address notice to multiple programs.
Guidance During Planning Phase Could Improve Project Success. The state takes on additional risk when strategic planning of IT investments is absent. High–quality and thorough planning best positions projects for success. The best practices shared by the OAIO and incorporated into project plans of CHHSA departments during the early stages of a project could have a critical impact on the success of the project. Guidance provided by the project assessment program that is part of the Governor’s budget proposal could be the difference between a successful project and a failed project.
Potentially Significant Cost Avoidance. The proposal could lead to potentially significant cost savings. First, the proposed project assessment program could produce better–planned projects, which could avoid costly rework commonly associated with inadequate planning. Second, the proposal’s focus on coordination and interoperability of CHHSA IT systems would allow the agency to identify opportunities where a single system could be leveraged—representing a more cost–effective approach to system development.
Ambitious Proposal With Limited Resources. The proposal requests modest resources to achieve ambitious policy objectives. It is the first time OAIO would be allocated dedicated staff towards fulfilling its mission. The historic use of redirected staff creates uncertainty regarding the amount of resources necessary to adequately achieve the objectives of the OAIO.
Proposed Provisional Language Does Not Appear to Facilitate Desired Outcome. We agree that requests and referrals for technical assistance from OSI likely often require timely attention in order for the assistance to be valuable. The administration has stated that OSI would be better positioned to provide timely assistance if it were granted an exemption from the Section 28.50 process, and it has proposed provisional budget language to this effect. It has stated that the review process for these requests (which includes the review of the DOF) can take three months or more. Since Section 28.50 allows for a waiver of what is at most a 30–day legislative review period, and given that most requests to increase reimbursement authority to accommodate requests for technical assistance have been below the cost threshold requiring legislative review under Section 28.50, it does not appear that Section 28.50 is the root cause of the problem identified by the administration. Rather, it appears that it is the administration’s own internal review processes that are impeding the provision by OSI of timely technical assistance to requesting projects.
We agree that the strategic enterprise architecture, governance, and project assessment programs included in the Governor’s budget proposal could better position the state for successful deployments of CHHSA technology systems and, therefore, support the crux of the Governor’s proposal in concept. However, it is uncertain what level of resources will be necessary to meet the proposal’s ambitious goals. Therefore, we recommend that the three requested positions be approved on a three–year limited–term basis, along with approval of $431,000 in reimbursement authority, to be followed by a status report to the Legislature from the Secretary of CHHSA on the effects of the proposal and the extent to which it met its statutory charge at the budgeted level of resources. The three–year duration and subsequent evaluation would also provide OAIO with an opportunity to assess workload demands and propose staffing adjustments to maximize the impact of strategic IT planning across CHHSA. This approach would strengthen OAIO’s ability to better meet its responsibilities in the near term, while allowing OAIO staffing levels to be revaluated and adjusted as needed in the long term.
At this time, we do not recommend approval of the proposed budget provisional language that would exempt augmentations to reimbursements for OSI from Section 28.50 of the annual budget act given that this exemption would not address what appear to be delays in the administration’s own internal review processes. In this regard, we recommend that the administration report at budget hearings on the steps that it can take to provide more efficient review to facilitate the provision of timely assistance by OSI to projects requesting such assistance.