Several state departments administer health care programs and some departments administer more than one program. For example, DHCS administers the state–federal Medicaid Program—known as Medi–Cal in California—as well as the California Children’s Services Program and other programs. Similarly, DPH administers the AIDS Drug Assistance Program (ADAP) and other programs aimed at protecting California’s population from infectious diseases. The health programs administered by state departments provide a variety of benefits to California’s citizens, including purchasing health care services for qualified low–income persons and performing various public health functions.
Most major state health programs are administered by one of the following three departments: (1) DHCS, (2) DPH, and (3) DSH. (Funding for state employees to administer health programs at the state level and/or provide services is known as “state operations.”) The actual delivery of many of the health care services provided through state programs takes place at the local level and is carried out by local government entities, such as counties, and private entities such as commercial health plans. (Funding for these types of services delivered at the local level is known as “local assistance.”) Most health services are provided through the local service delivery model.
Overview of Health Budget Proposal. The Governor’s budget proposes $18.8 billion from the General Fund for health programs. This is an increase of $714 million—or 3.9 percent—above the revised estimated 2013–14 spending level, as shown in Figure 1. The net increase reflects increases in caseload and changes in utilization of services as well as the impact of major ongoing initiatives.
Figure 1
Major Health Programs and Departments—Budget Summary
General Fund (Dollars in Millions)
|
|
2012–13Actual
|
2013–14 Estimated
|
2014–15 Proposed
|
Change From 2013–14
|
|
Amount
|
Percent
|
|
Medi–Cal—Local Assistance
|
$14,862
|
$16,230
|
$16,900
|
$670
|
4.1%
|
|
Department of State Hospitals
|
1,277
|
1,505
|
1,515
|
10
|
0.7
|
|
Healthy Families Program (HFP)—Local Assistancea
|
176
|
22
|
—
|
–22
|
—
|
|
Department of Public Health
|
129
|
115
|
111
|
–4
|
–3.5
|
|
Department of Alcohol and Drug Programs (DADP)b
|
34
|
—
|
—
|
—
|
—
|
|
Other Department of Health Care Services programs
|
110
|
87
|
141
|
54
|
62.1
|
|
Emergency Medical Services Authority
|
7
|
7
|
7
|
—
|
—
|
|
All other health programs (including state support)
|
149
|
165
|
171
|
6
|
3.6
|
|
Totals
|
$16,744
|
$18,131
|
$18,845
|
$714
|
3.9%
|
Summary of Major Budget Proposals and Changes. The budget plan reflects the fiscal effects of a major Medi–Cal provider payment proposal and two proposals to make state–level organizational changes. Regarding the latter, the administration proposes to transfer $200 million in all funds ($5 million General Fund) and 291 positions for the administration of DWP from DPH to SWRCB. The administration also proposes to transfer three health insurance programs from MRMIB to DHCS and eliminate MRMIB effective July 1, 2014. This would continue the shift of health insurance programs from MRMIB to DHCS that began with the transfer of the Healthy Families Program (HFP) in January 2013. As shown in Figure 1, General Fund spending for HFP decreases from a revised estimate of $22 million in 2013–14 to no expenditures in 2014–15 to reflect the completed transfer of children in HFP to Medi–Cal in November of 2013.
In 2011, budget–related legislation authorized reductions in certain Medi–Cal payments by up to 10 percent. Until recently, federal court injunctions prevented the state from implementing many of these reductions. In June 2013, the injunctions were lifted, giving the state authority to: (1) apply the reductions to current and future payments to providers on an ongoing basis and (2) retroactively recoup the reductions from past payments that were made to providers during the period in which the injunctions were in effect. The Governor’s budget proposes to exempt certain (but not all) classes of providers and services from the retroactive recoupments, and includes $36 million in increased General Fund expenditures in 2014–15 associated with this exemption proposal. Because the recoupments were otherwise scheduled to take place over several years, the total General fund cost of the proposal over this multiyear period is estimated to be $218 million. (We note that the budget assumes that the provider payment reductions—unless exempted legislatively or administratively—will continue prospectively, resulting in ongoing General Fund savings of $245 million in 2014–15.)
Summary of Major Ongoing Initiatives. The budget plan reflects the fiscal effects of major health policy initiatives that are under implementation. First, the budget assumes a couple of major fiscal effects associated with various provisions of the ACA that were enacted as part of the 2013–14 budget. For example, the budget assumes about $400 million in net General Fund costs in 2014–15 largely associated with the implementation of simplified Medi–Cal eligibility and enrollment processes that are expected to increase enrollment among individuals who are eligible for the program—often referred to as the mandatory Medi–Cal expansion. In addition, the budget assumes General Fund savings of $300 million in 2013–14 and $900 million in 2014–15 from implementation of the optional Medi–Cal expansion. These savings are realized through changes to the 1991 health realignment that were authorized as part of the 2013–14 budget and result in lower state General Fund costs in the California Work Opportunity and Responsibility to Kids (CalWORKs) budget.
The budget plan also assumes a General Fund cost of $173 million from beginning implementation of the Coordinated Care Initiative (CCI) in 2014–15. (The CCI is scheduled to begin no sooner than April 2014 in eight counties.) Once fully implemented, CCI is estimated to save hundreds of millions of General Fund dollars annually. The CCI is intended to better serve seniors and persons with disabilities through improved integration of long–term care, behavioral health, and medical services. Specifically, the CCI includes two main components: (1) a three–year demonstration project, known as Cal MediConnect, for individuals—often referred to as “dual eligibles”—who are eligible for both Medi–Cal and Medicare and (2) integration of long–term services and supports (LTSS) into managed care and a requirement for nearly all Medi–Cal beneficiaries to be enrolled in managed care to receive these benefits. Implementation of CCI involves several departments, including DHCS, the Department of Social Services, and the Department of Aging.
Caseload trends are one important factor influencing state health care expenditures. Below, we highlight the caseload trends assumed in the Governor’s budget for Medi–Cal—by far the largest state–administered health program.
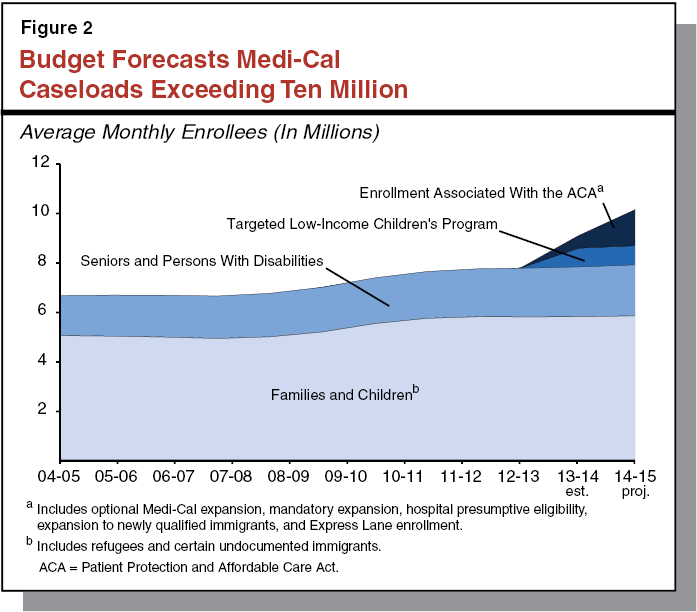
Medi–Cal Caseload. The Governor’s budget plan projects an average monthly Medi–Cal caseload of 9.2 million in 2013–14 and 10.3 million in 2014–15—an 11.6 percent year–over–year increase. This increase is mainly the result of implementing various ACA–related provisions. Figure 2 illustrates past Medi–Cal caseloads and the Governor’s projected caseload trends for Medi–Cal in 2013–14 and 2014–15, divided into four groups: (1) seniors and persons with disabilities (SPDs), (2) families and children, (3) the Targeted Low–Income Children’s Program, or TLICP (including children formerly in HFP), and (4) individuals who will enroll as a result of various ACA–related changes. The SPDs and families with children categories include estimated underlying caseload trends for these populations, absent the effects of recent major policy changes. These two underlying caseload categories are projected to grow by about 1 percent between 2013–14 and 2014–15. The TLICP enrollment is projected to grow by 2.7 percent between 2013–14 and 2014–15. The remaining year–over–year caseload increase is largely the result of ACA implementation, including expanded eligibility for certain adult populations that began January 1, 2014, and various changes to the eligibility determination process that are expected to increase the proportion of eligible individuals who enroll. We discuss the Governor’s Medi–Cal caseload estimates, including estimated caseload increases associated with the ACA, in more detail below.
In California, the federal–state Medicaid Program is administered by DHCS as the California Medical Assistance Program (Medi–Cal). Medi–Cal is by far the largest state–administered health services program in terms of annual caseload and expenditures. As a joint federal–state program, federal funds are available to the state for the provision of health care services for most low–income persons. Until recently, Medi–Cal eligibility was mainly restricted to low–income families with children, SPDs, and pregnant women. California generally receives a 50 percent Federal Medical Assistance Percentage (FMAP) (federal share of costs) for these populations—meaning the federal government pays one–half of Medi–Cal costs for these populations. As part of the ACA, beginning January 1, 2014, the state expanded Medi–Cal eligibility to include additional low–income populations—primarily childless adults who did not previously qualify for the program. The federal government will pay 100 percent of the costs of providing health care services to this newly eligible Medi–Cal population from 2014 through 2016; the federal matching rate will phase–down to 90 percent by 2020 and thereafter.
There are two main Medi–Cal systems for the delivery of medical services: FFS and managed care. In a FFS system, a health care provider receives an individual payment from DHCS for each medical service delivered to a beneficiary. Beneficiaries in Medi–Cal FFS generally may obtain services from any provider who has agreed to accept Medi–Cal FFS payments. In managed care, DHCS contracts with managed care plans, also known as health maintenance organizations, to provide health care coverage for Medi–Cal beneficiaries. Managed care enrollees may obtain services from providers who accept payments from the managed care plan, also known as a plan’s “provider network.” The plans are reimbursed on a “capitated” basis with a predetermined amount per person, per month regardless of the number of services an individual receives. Medi–Cal managed care plans provide enrollees with most Medi–Cal covered health care services—including hospital, physician, and pharmacy services—and are responsible for ensuring enrollees are able to access covered health services in a timely manner.
The Governor’s budget proposes $16.9 billion General Fund in 2014–15 for local assistance under the Medi–Cal Program, including the provision of health care services and administrative costs. This is a $670 million net increase, or 4.1 percent, over estimated 2013–14 expenditures. Generally, the level of expenditures and changes in year–over–year spending are driven by various factors, including:
- The total enrollment of beneficiaries in the program and per–person cost of providing health care services, which is affected by both the price and level of utilization for individual services.
- Technical changes that result from the timing of receipt or payment of funds.
- Implementation of various state and federal policy changes enacted in recent years.
Major Policies Affecting Year–Over–Year Spending Changes. The Governor’s 2014–15 budget reflects recent implementation and planned implementation of major programmatic changes enacted in recent years, including:
- ACA Implementation. The budget includes a variety of significant fiscal effects related to ACA implementation. Changes related to the ACA result in both costs and savings to the Medi–Cal Program that are hundreds of millions of dollars annually in some instances. We discuss the major ACA–related changes in the “ACA Implementation” section below.
- CCI. The budget assumes a General Fund cost of $173 million from beginning implementation of CCI no sooner than April 1, 2014. This is because the state will incur upfront costs from making both managed care payments and retroactive FFS payments as beneficiaries and services transition to Medi–Cal managed care. (Once fully implemented, CCI is estimated to save hundreds of millions of General Fund dollars annually.) The administration recently announced that one of the demonstration plans, CalOptima in Orange County, was subject to a federal audit of its existing Medicare Special Needs product for dual eligibles. As a result of this audit, the Cal MediConnect portion of CCI will not proceed in Orange County—which represents about 14 percent of the estimated 456,000 beneficiaries eligible for enrollment in Cal MediConnect—until CalOptima takes corrective actions to address the deficiencies uncovered by the audit. At the time of this analysis, the administration had not released updated fiscal estimates to reflect anticipated changes in CCI enrollment resulting from CalOptima’s temporary removal from the demonstration.
- Payment Reductions. The budget assumes that the state will continue to implement reductions to payments, enacted in 2011, to certain providers and managed care plans for certain services. (Some providers have been legislatively or administratively exempted from the payment reductions.) The budget assumes net General Fund savings of $100 million in 2013–14 and $246 million in 2014–15. (These estimates reflect reduced savings due to a temporary exemption from the payment reduction for primary care services in 2013 and 2014, as required by the ACA.) We discuss the implementation of these payment reductions in the “Medi–Cal Payment Reductions and Access to Care” section later in this analysis.
- Tax on Medi–Cal Managed Care Plans. The budget assumes General Fund offsets of $256 million in 2013–14 and $462 million in 2014–15 from a tax on Medi–Cal managed care organizations (MCOs), known as the MCO tax, that was authorized as part of the 2013–14 budget. These estimates exclude additional MCO tax General Fund offsets associated with a significant increase in Medi–Cal managed care enrollment under the ACA—$51 million in 2013–14 and $233 million in 2014–15—which are accounted for as General Fund offsets in the “ACA Implementation” section later in this analysis.
- Hospital Fee. The budget assumes General Fund offsets of $155 million in 2013–14 and $713 million in 2014–15 from the recently enacted hospital quality assurance fee. These estimates reflect a delay in implementation as the state seeks federal approval of the new fee program. The administration has indicated that it expects to receive this approval no sooner than June 2014.
Managed Care Enrollment Continues to Increase. Managed care is increasingly becoming the dominate delivery system in the Medi–Cal program as both the number and the percentage of Medi–Cal beneficiaries enrolled in managed care continues to grow. Roughly 65 percent of beneficiaries were enrolled in managed care in 2012–13. The Governor’s budget projects that, on average, 70 percent of beneficiaries will be enrolled in managed care in 2013–14 and 73 percent—about 7.5 million Medi–Cal beneficiaries—will be enrolled in managed care in 2014–15. The increase in managed care enrollment reflects transitions of beneficiaries from FFS to managed care, as well as additional enrollees associated with the transfer of HFP and implementation of the ACA.
Baseline Caseload Estimates Reasonable. The administration projects baseline caseload—or program caseload absent changes associated with recent major policy changes, such as the shift of HFP and implementation of the ACA—will be about 7.7 million average monthly enrollees in 2013–14 and 7.8 million in 2014–15—a 1 percent year–over–year increase. We have reviewed the administrations baseline caseload projections and we do not recommend any adjustments at this time. If we receive additional information that causes us to change our assessment, we will provide the Legislature with an updated analysis at the time of the May Revision.
ACA Estimates Are Generally Reasonable. As shown in Figure 3, the budget assumes that various ACA provisions will result in nearly 1.5 million additional average monthly enrollees in 2014–15. The caseload increase includes additional enrollment associated with the optional expansion, mandatory expansion, hospital presumptive eligibility, and Express Lane enrollment. (Please see our “ACA Implementation” section below for a more detailed description of these changes.) We have reviewed the administration’s caseload estimates and, accounting for the significant amount of uncertainty about how the ACA will affect Medi–Cal caseload, we find the estimates to be reasonable. If we receive additional information that causes us to change our assessment, we will provide the Legislature with an updated analysis at the time of the May Revision.
Figure 3
Major ACA Caseload Estimates
Average Monthly Enrollees (In Thousands)
|
|
2013–14
|
2014–15
|
|
Optional expansiona
|
330
|
779
|
|
Mandatory expansionb
|
130
|
509
|
|
Express Lane enrollmentc
|
17
|
151
|
|
Hospital presumptive eligibilityd
|
25
|
32
|
|
Totals
|
502
|
1,471
|
High TLICP Caseload Projection Raises Questions. The HFP provided health coverage to children in households with incomes too high to qualify for Medi–Cal, but below 250 percent of the federal poverty level (FPL). The transition of children from HFP to Medi–Cal generally did not change the eligibility criteria. Children transferring from HFP were enrolled in the newly created Medi–Cal TLICP, which provides coverage to children in families with incomes too high to qualify for Medi–Cal, but below 250 percent FPL. (Beginning January 1, 2014, state Medicaid programs converted to the new Modified Adjusted Gross Income method for counting income for most beneficiaries and the new converted standard for the TLICP is 261 percent FPL.) When the transition began in January 2013, approximately 850,000 children were enrolled in HFP.
The Governor’s budget estimates that about 995,000 beneficiaries will be enrolled in the TLICP in 2014–15—representing a nearly 17 percent increase in caseload over roughly a two–year period. This is a large increase in caseload, compared to the relatively stable HFP caseload in the years before the transition began. According to the administration, there has been a significant increase in TLICP enrollment that appears to be driven by a large number of children shifting from existing Medi–Cal categories to the new TLICP categories—possibly caused by increasing incomes as the economy improves.
In our view, it is unlikely that the economic recovery alone would explain such a significant increase in TLICP caseload. This is because rising incomes associated with the economic recovery could serve to both increase and decrease the TLICP caseload. For example, individuals who were previously eligible for Medi–Cal who experience an increase in income may become eligible for the TLICP, thereby increasing caseload. On the other hand, individuals who were previously eligible for the TLICP whose families’ experience an increase in income may have incomes that are too high to qualify for the program, thereby decreasing caseload. While the degree to which these two factors offset each other is uncertain, it is unlikely that changing economic conditions alone would cause such a significant and rapid net increase in caseload.
Recommend Legislature Direct DHCS to Report on TLICP Caseload. We recommend the Legislature direct the administration to report at budget hearings on all the factors contributing to the significant increase in TLICP caseload. With more comprehensive information on the basis for the administration’s projections, the Legislature can assess whether the amount budgeted for the TLICP caseload is the appropriate amount and whether the higher caseload reflects any unintended changes in children’s health coverage associated with the HFP transition to Medi–Cal.
The budget assumes a wide variety of fiscal effects—some major and some minor—associated with implementing various provisions of state and federal law related to the ACA. Many of the ACA provisions that affect the Medi–Cal Program went into effect in 2013 or early 2014 and the effects of many of these changes are still highly uncertain. In this section, we: (1) summarize the major ACA state fiscal effects that are estimated in the Medi–Cal budget and provide our assessment of them, (2) identify some potential fiscal effects that are omitted from the budget, (3) provide our assessment of the Governor’s proposal to modify coverage offered to pregnant women in Medi–Cal, (4) raise issues that the Legislature may want to consider in light of recent ACA changes, and (5) provide recommendations that are generally intended to enhance legislative oversight of ACA implementation.
Figure 4 summarizes the major ACA–related fiscal effects (over $10 million General Fund in a year) that are included in the 2014–15 Medi–Cal local assistance budget. Figure 4 also includes estimated General Fund savings (in the CalWORKs budget) from the changes to 1991 health realignment that were enacted as part of the 2013–14 budget. These changes reflect the decreased county indigent care responsibilities as a result of the expansion of Medi–Cal under the ACA. Some of the major ACA fiscal effects are the result of complying with federal requirements, such as the costs associated with the so–called mandatory Medi–Cal expansion. Other major ACA fiscal effects are the result of choices made by the Legislature, such as the decision to adopt the optional Medi–Cal expansion. We note that Figure 4 excludes some other major ACA fiscal effects assumed in the 2014–15 budget, such as additional General Fund offsets gained through increased hospital fee revenue (no estimates of this amount were available at the time of this analysis) and additional federal funding that is used to offset state General Fund spending in other state departments.
Figure 4
Selected Major Fiscal Effects of the Patient Protection and Affordable Care Act on Medi–Cala
(In Millions)
|
|
2013–14
|
|
2014–15
|
|
Federal Funds
|
General Fund
|
Federal Funds
|
General Fund
|
|
Additional Enrollment
|
|
|
|
|
|
|
Optional expansion
|
$2,618
|
–$43
|
|
$6,622
|
–$198
|
|
Changes to 1991 health realignmentb
|
—
|
–300
|
|
—
|
–900
|
|
Mandatory expansion
|
119
|
104
|
|
448
|
419
|
|
Express Lane enrollment
|
70
|
1
|
|
676
|
12
|
|
Hospital presumptive eligibility
|
13
|
10
|
|
43
|
39
|
|
County Administration
|
|
|
|
|
|
|
Additional county administration funding
|
72
|
72
|
|
65
|
65
|
|
Enhanced federal match for certain eligibility determination functions
|
124
|
–124
|
|
248
|
–248
|
|
Changes to Benefits
|
|
|
|
|
|
|
Enhanced mental health services
|
45
|
28
|
|
181
|
119
|
|
Enhanced substance use disorder services
|
51
|
33
|
|
127
|
79
|
|
Shift certain pregnant women to Covered California
|
—
|
—
|
|
–17
|
–17
|
|
Other Changes
|
|
|
|
|
|
|
Temporary rate increase for primary care services
|
1,628
|
34
|
|
575
|
27
|
|
Health insurer fee
|
—
|
—
|
|
67
|
55
|
|
Collect managed care drug rebates
|
–194
|
–194
|
|
–146
|
–179
|
|
One percent increase in federal match for preventative services
|
40
|
–40
|
|
27
|
–27
|
The state budget will continue to be affected by ACA implementation in the future. The estimates included in the budget plan generally do not reflect future state costs and savings associated with ACA implementation that will occur after 2014–15. For example, the enhanced federal cost share for the newly eligible Medi–Cal optional expansion population will begin to phase down in 2017, resulting in increased state costs. However, the federal cost–share for the Medi–Cal population that was formerly enrolled in HFP—now referred to as TLICP—will temporarily increase in October 2015, resulting in state savings.
In the next section of this analysis, we describe eligibility expansions, changes to county administration of eligibility determinations, changes to Medi–Cal benefits, and other major ACA–related changes that affect the Medi–Cal budget.
Additional enrollment in Medi–Cal resulting from ACA implementation will result in both state costs and savings. Much of the additional enrollment is a result of expanded Medi–Cal eligibility. Other ACA changes—such as penalties for not obtaining coverage (also known as the individual mandate), increased outreach activities, and new enrollment pathways—will increase enrollment above the levels that would otherwise have occurred in the absence of these changes. We first describe the major fiscal effects related to increased Medi–Cal enrollment under the ACA that are included in the Governor’s budget.
Optional Expansion. Effective January 1, 2014, Medi–Cal eligibility expanded to include previously ineligible adults with incomes up to 138 percent FPL—largely childless adults. The administration estimates that nearly 700,000 newly eligible beneficiaries will enroll in 2013–14, growing to over 800,000 newly eligible beneficiaries in 2014–15. (Newly eligible persons who enroll through new enrollment pathways such as Express Lane enrollment or hospital presumptive eligibility are estimated separately and discussed in more detail below.) The federal government is paying for 100 percent of the health care costs for the newly eligible population through 2016. Fiscal estimates of the optional expansion incorporate savings achieved from higher General Fund offsets from the MCO tax and costs for providing services to certain newly qualified immigrants who are eligible for state–only Medi–Cal coverage under state law. Savings from changes to 1991 health realignment and stemming from the optional Medi–Cal expansion are estimated separately.
Historically, counties have had the fiscal and programmatic responsibility for providing health care for low–income populations without public or private health coverage—also known as indigent health care. As part of 1991 realignment, the state provided a dedicated funding stream to counties for indigent health care and public health activities—hereafter referred to as health realignment funds. The optional Medi–Cal expansion shifts much of the responsibility for indigent health care to the state and federal governments, and counties are likely to experience significant savings. In recognition of the shifting responsibilities for indigent health care, the 2013–14 budget established a complex structure under which a portion of county health realignment funds will be redirected to help pay CalWORKs grant costs previously borne by the state—thereby offsetting state General Fund costs. The methods used to determine the redirected amount differ among counties and some counties will have the option to choose between two general approaches: (1) the so–called “60/40” option, whereby a predetermined percentage of health realignment funds will be redirected from the county each year, or (2) the so–called “formula” option whereby 80 percent of the estimated savings counties realize under the ACA is redirected to the state. The amount that can be redirected in 2013–14 is capped at $300 million. For more detail on the different methods for determining the redirected amount, see our November report, The 2013–14 Budget: California Spending Plan. The administration projects $300 million will be redirected in 2013–14 and $900 million will be redirected in 2014–15.
Mandatory Expansion. Several federal ACA requirements will result in additional Medi–Cal enrollment and state costs. For example, the ACA includes requirements that will likely encourage individuals who were eligible for Medi–Cal prior to January 1, 2014, but not enrolled, to enroll in the program (hereafter referred to as previously eligible populations). These requirements include streamlining and simplifying the eligibility determination process and a penalty for certain individuals who do not obtain health coverage (also known as the individual mandate). The ACA also requires Medi–Cal to expand eligibility to include former foster youth up to age 26. Collectively, the administration refers to these changes as as the “mandatory expansion.” Generally, the state will continue to be responsible for 50 percent of the costs of providing services to these new enrollees. A small portion of the state costs will be offset by savings from higher MCO tax General Fund offsets that result from the additional enrollment. The administration assumes net mandatory expansion costs of $104 million General Fund in 2013–14 and $419 million General Fund in 2014–15.
Hospital Presumptive Eligibility. Prior to ACA implementation, some Medi–Cal providers have been able to grant temporary presumptive eligibility to a limited group of individuals, including pregnant women and children. Beginning January 1, 2014, under the ACA, hospitals now have the option to make presumptive eligibility determinations for most Medi–Cal applicants on the basis of preliminary information provided by individuals, generally when they seek care at the hospital. Individuals who are determined presumptively eligible may receive full–scope Medi–Cal for up to two months, at which point the individual will need to complete a full Medi–Cal eligibility application in order to continue to qualify for coverage. Implementation of hospital presumptive eligibility will result in an estimated partial–year General Fund cost of $10 million in 2013–14 and a full–year General Fund cost of $39 million in 2014–15.
Express Lane Enrollment. States have the option to implement “Express Lane” enrollment, whereby a streamlined process is used to enroll certain persons who—based on information already available to states—are likely to be eligible for Medicaid, but not yet enrolled. California is scheduled to implement an Express Lane enrollment option in February 2014 for persons who are enrolled in the Supplemental Nutrition Assistance Program, also known as CalFresh in California. The state is targeting its Express Lane enrollment process toward adults who are likely newly eligible for Medi–Cal and, thus, most of the costs associated with providing coverage to the new enrollees would be eligible for a 100 percent federal match. In the future, the state also plans to implement an Express Lane process for parents with children in Medi–Cal and enrollees in other state health programs, such as the Genetically Handicapped Persons Program (GHPP), Every Women Counts, and the Prostate Cancer Treatment Program. The administration estimates that over 300,000 individuals will enroll through the new Express Lane enrollment process in 2014, roughly 50 percent of whom would not have otherwise enrolled in the program through one of the other enrollment pathways. Implementation of Express Lane enrollment will result an estimated partial–year General Fund cost of $1 million in 2013–14 and a full–year General Fund cost of $12 million in 2014–15.
The ACA will increase the number of Medi–Cal applicants and require counties to make changes to how they carry out eligibility determinations for Medi–Cal applicants. In addition, under new federal rules related to the ACA, a significant portion of state General Fund costs for Medi–Cal eligibility determinations may be offset by an enhanced federal match for specified functions.
County Administration Funding for Eligibility Determinations. The ACA contains several provisions that will affect county administration costs for conducting Medi–Cal eligibility determinations. Certain provisions of the ACA—such as those that significantly increase the number of Medi–Cal applications and enrollees—will increase costs for counties conducting Medi–Cal eligibility determinations. On the other hand, ACA provisions that simplify the eligibility determination process will likely reduce the average cost of conducting eligibility determinations and redeterminations. The Governor’s budget provides $65 million of additional General Fund support for counties in 2014–15 to fund costs related to ACA implementation—slightly less than the $72 million of additional General Fund provided in the 2013–14 budget because it removes one–time costs for training county eligibility workers and county/state–level planning and implementation. (These costs do not reflect the ongoing $15 million General Fund cost–of–living adjustment that was provided for county eligibility determination activities in 2013–14.)
Enhanced Federal Funding for Certain Eligibility Determination Functions. Generally, payments to counties for making Medi–Cal eligibility determinations for both the previously and newly eligible populations are eligible for a 50 percent federal match. However, federal guidance released in 2011 allows states to receive a 75 percent federal match for certain eligibility determination functions, including costs for processing applications, case maintenance, and renewals. (Activities classified as policy, outreach, or post–eligibility are not eligible for the 75 percent match.) In order to qualify for the enhanced federal funding, states must meet certain minimum eligibility system requirements outlined by the federal government, including coordinating with the health insurance Exchange operating in the state, which in California is called Covered California. (The federal guidance is not solely related to ACA implementation, but the regulations are, in part, related to changes in Medicaid eligibility determination systems and processes under the ACA.) The DHCS must secure federal approval prior to receiving the enhanced federal match. The budget assumes the state currently meets federal requirements and will be eligible to receive the enhanced federal funding for roughly 70 percent of county eligibility determination costs incurred after January 1, 2014.
Enhanced Mental Health and Substance Use Disorder Services. As part of ACA implementation, California is providing all Medi–Cal–covered nonspecialty mental health services through managed care, including some new mental health services that are included in the benefits package that is covered by plans offered through Covered California. These services will be available for both the previously and newly eligible Medi–Cal populations. The state will also provide an enhanced set of substance use disorder services for previously and newly eligible populations. The budget assumes General Fund costs of $198 million in 2014–15 to provide these additional services.
Shift Certain Pregnant Women to Covered California. The Governor’s 2014–15 budget proposes to shift pregnant women between 109 percent and 208 percent FPL who qualify for Medi–Cal pregnancy–only coverage to plans offered through Covered California. The administration also proposes to provide full–scope coverage—rather than pregnancy–only coverage—to all pregnant women below 109 percent FPL who receive coverage from Medi–Cal. The budget assumes General Fund savings of $17 million in 2014–15 related to this proposal. We discuss the Governor’s pregnancy–only proposal and our assessment of it in more detail below.
Similar proposals were discussed last year in budget subcommittee and policy committees. For example, the administration proposed a similar shift of pregnant women to Covered California and the associated savings were adopted as part of the 2013–14 budget under the assumption that the details of the proposal would be worked out through policy committees. However, the statutory language authorizing such a shift was never enacted.
Temporary Primary Care Physician Rate Increase. The ACA requires states to increase Medicaid primary care physician service rates to 100 percent of Medicare rates for services provided from January 1, 2013 through December 31, 2014. The rate increase applies to services provided in both FFS and managed care. The federal government will pay for 100 percent of the incremental increase above the Medi–Cal rates that were in effect as of July 1, 2009. Since the state enacted a 9 percent payment reduction for Medi–Cal primary care services in 2011, it must temporarily pay for the state share of the incremental difference between existing Medi–Cal rates and the rates that were in effect on July 1, 2009. The budget includes foregone General Fund savings associated with not implementing the scheduled payment reduction for primary care services in 2013 and 2014, as well as additional administrative costs associated with implementing the rate increase in managed care. The budget assumes the higher rates for primary care services sunset at the end of 2014 and the 9 percent reduction to primary care services that was postponed for 2013 and 2014 will go into effect at the start of 2015.
Health Insurer Fee. The ACA established a nationwide fee on the health insurance industry beginning January 2014. The nationwide fee will initially generate $8 billion annually and grow to $14.3 billion annually by 2018. The fee is allocated to qualifying health insurers based on their relative market share and exempts certain insurers such as nonprofit insurers that receive a substantial share of their premium revenue from public programs, such as Medicaid and Medicare. The budget includes costs associated with higher state payments to Medi–Cal managed care plans that are subject to the fee.
Managed Care Drug Rebates. The ACA extended the federal drug rebate requirement to outpatient drugs covered by all Medi–Cal managed care plans. Previously, drug rebates were collected for drugs provided through FFS and certain managed care plans. The fiscal estimates provided in Figure 4 include $33 million savings from a new proposal in the Governor’s budget that would allow the state to collect additional MCO supplemental drug rebates. Many of the details associated with this proposal are still unclear so we are unable to comment on the merits of the proposal at this time.
FMAP Increase for Preventative Services. Effective January 1, 2013, the ACA established a 1 percentage point increase in the federal matching rate for preventative services and adult vaccines in states that meet certain requirements. In order to qualify for the increase, a state must cover all preventative services assigned a Grade A or B by the United States Preventative Services Task Force (USPSTF) and all approved vaccines recommended by the Advisory Committee on Immunization Practices and cannot impose beneficiary cost–sharing on such services. California opted to provide the preventative services necessary to qualify for the enhanced match and to not impose beneficiary cost–sharing for these preventative services. The budget includes $26.4 million General Fund costs from adding screening and counseling services for alcohol and substance use—services that were recently assigned a Grade A or B by the USPSTF—to the existing benefits package effective January 1, 2014. With this addition, the state will provide all services assigned Grade A or B; although we note that, at the time of this analysis, it is unclear whether these preventative services would have been added in the absence of the enhanced FMAP for preventative services. The budget assumes General Fund savings of $27 million in 2014–15 associated with the 1 percent increase in the federal match for preventative services.
We have reviewed the major ACA–related fiscal estimates included in the Governor’s budget, including the major underlying assumptions upon which these estimates are based. There is a significant amount of uncertainty surrounding many of the estimates, generally due to limited available data and actual experience as many ACA changes were only recently implemented. Based on currently available information, we find the administration’s ACA–related fiscal estimates to be reasonable. However, more reliable data and actual experience from the initial months of ACA implementation should become available in the next several months to better inform future ACA–related fiscal estimates. We highlight two major areas of uncertainty below: health realignment savings and mandatory expansion costs.
Health Realignment Savings. In recent weeks, information has been released that helps inform estimates of the amount of health realignment savings that will be achieved in 2013–14 and 2014–15. For example, counties have made decisions about which method they are using to determine realignment savings: the shared savings formula or the 60/40 option. These decisions are shown in Figure 5. In addition, based on information submitted by counties, DHCS determined the historical percentage of health realignment funds that has been spent on indigent health care which, among other things, will be used to establish a cap on the amount of realignment funds that can be redirected from counties that select the shared savings formula. (Counties have until February 28, 2014 to formally dispute these percentages.)
Figure 5
County Health Realignment Decisions
|
County
|
Decisiona
|
|
Counties With County Hospitals
|
|
|
Alameda
|
Formula
|
|
Contra Costa
|
Formula
|
|
Kern
|
Formula
|
|
Los Angeles
|
Formulab
|
|
Monterey
|
Formula
|
|
Riverside
|
Formula
|
|
San Bernardino
|
Formula
|
|
San Francisco
|
Formula
|
|
San Joaquin
|
Formula
|
|
San Mateo
|
Formula
|
|
Santa Clara
|
Formula
|
|
Ventura
|
Formula
|
|
Counties Without County Hospitals
|
|
|
Fresno
|
Formula
|
|
Merced
|
Formula
|
|
Orange
|
Formula
|
|
Placer
|
60/40
|
|
Sacramento
|
60/40
|
|
San Diego
|
Formula
|
|
San Luis Obispo
|
Formula
|
|
Santa Barbara
|
60/40
|
|
Santa Cruz
|
Formula
|
|
Stanislaus
|
60/40
|
|
Tulare
|
Formula
|
|
Yolo
|
60/40
|
While the newly available information helps inform estimates of the amount of health realignment funds that will be redirected to offset General Fund costs in CalWORKs, the state and counties are still in the process of collecting and analyzing data that will be used to project savings in counties that selected the shared savings formula. It is in these counties where the projected savings are subject to the most uncertainty because savings will depend on a variety of ACA impacts that remain highly uncertain. For example, the amount of realignment funds that will be redirected from counties that elect the shared savings formula and operate county hospitals will depend on uncertain factors such as how the ACA affects the number of patients who will receive care from county hospitals and whether these patients have Medi–Cal or other sources of health coverage.
Our office’s November Fiscal Outlook assumed $930 million in General Fund savings from health realignment. Based on our initial review of the additional information that has become available since that projection, our revised savings estimates are similar to what we projected in November. Given the uncertainty discussed above, we consider $900 million—the January budget’s assumed savings—a reasonable “placeholder” number until more detailed and reliable data becomes available. When the administration provides revised projections of health realignment savings, we will provide the Legislature with an updated assessment.
Mandatory Expansion Costs. Mandatory expansion costs largely depend on behavioral responses that are very difficult to predict, such as responses to the individual mandate, and the degree to which the new simplified eligibility processes serve to facilitate enrollment and thereby increase caseload. In addition, the degree to which changes in caseload among the previously eligible population are attributable to factors related to the mandatory expansion versus some other recent policy changes, such as Express Lane enrollment, is highly uncertain. For example, some previously eligible individuals who enroll in Medi–Cal in response to the individual mandate, may have otherwise enrolled through the new Express Lane enrollment process. The degree to which caseload changes associated with the various ACA policy changes overlap is highly uncertain.
Last year, we conducted a detailed analysis of the administration’s mandatory expansion cost estimates. At the time of that analysis, the administration estimated mandatory expansion costs would be roughly $650 million General Fund in 2014–15. Our analysis concluded that the administration’s mandatory expansion cost estimates, while plausible, were significantly higher than what we considered most likely (about $300 million General Fund in 2014–15).
The Governor’s 2014–15 budget now estimates just over $400 million in General Fund costs in 2014–15 for the mandatory expansion. This estimate is similar to our office’s most recent estimate of slightly more than $350 million General Fund. We believe the administration’s mandatory expansion cost estimate is reasonable. Somewhat more reliable mandatory expansion cost estimates may be available in a few months, after more data are collected and analyzed and the effects of ACA implementation are better understood. When the administration provides updated mandatory expansion estimates in May, we will provide the Legislature with an updated assessment.
Budget Does Not Include an Estimate of Savings Related to Claiming Enhanced Federal Funds, as Required by State Law. Under some of the new ACA eligibility rules and the optional expansion, the state may be able to claim a 100 percent federal match for some enrollees who would have previously qualified for a 50 percent match. Chapter 23, Statutes of 2013 (AB 82, Committee on Budget), requires DHCS to report to the Legislature, each January and May, the projected General Fund savings attributable to claiming enhanced federal funding for previously eligible Medi–Cal beneficiaries. The law also required DHCS to confer with applicable fiscal and policy staff of the Legislature by no later than October 1, 2013 regarding the potential content and attributes of the information provided in its savings estimate.
The administration has not complied with either of these requirements. The DHCS did not confer with all of the relevant fiscal staff of the Legislature by October 1, 2013. Furthermore, the Governor’s January budget does not include the required fiscal estimate. According to the administration, the details of the federal claiming process are still being discussed with the federal government and the administration did not provide an estimate because it has no basis on which to estimate savings.
In our view, preliminary fiscal estimates of factors that will likely have significant effects on the amount of General Fund spending in the Medi–Cal Program should be included in the budget—even if these estimates are highly uncertain and subject to change in the coming months. The Medi–Cal budget frequently contains preliminary estimates and assumptions that are based on limited data and experience. For example, many of the other ACA–related fiscal estimates discussed above are subject to substantial uncertainty and are based on assumptions that are based on limited actual experience, yet these estimates are included in the budget. Such estimates serve as placeholders until more refined estimates can be completed and allow for more informed budget deliberations because the Legislature has an opportunity to assess the administration’s estimates and assumptions and discuss the budget with a more complete understanding of the factors affecting expected General Fund spending.
Recommend Legislature Direct Administration to Report on Estimates of Enhanced Federal Funding for Previously Eligible Beneficiaries. We recommend the Legislature direct the administration to report at budget hearings on the reasons it failed to confer with all of the relevant legislative staff and provide a fiscal estimate of enhanced federal funding available for previously eligible beneficiaries, as required by state law. In addition, we recommend the Legislature direct the administration to describe: (1) the previously eligible populations that may now be eligible for the 100 percent federal match, (2) the total amount of General Fund that was spent on these populations in previous years, (3) the major sources of uncertainty that led to the decision to not include a fiscal estimate in the budget, and (4) the administration’s timelines for providing its fiscal estimate. With this additional information, the Legislature can begin to assess the potential magnitude of the fiscal effects and account for these effects as it discusses the 2014–15 budget.
Budget Does Not Assume Caseload Decreases for Some Smaller State Health Programs. Some state health programs, such as certain programs that are optional under federal Medicaid law—such as the Breast and Cervical Cancer Treatment Program (BCCTP)—or funded primarily with state funds (also known as state–only programs)—such as the GHPP—have traditionally provided coverage to individuals who may not qualify for full–scope Medi–Cal and who may not have private health insurance. Figure 6 lists the major optional and state–only health programs. Under the ACA, some of the individuals who would have otherwise enrolled in these programs will likely obtain coverage through the optional Medi–Cal expansion or Covered California—thereby likely decreasing caseload in these programs. In some programs, such as the ADAP, the budget adjusts for savings associated with reduced caseload under the ACA. In other programs, the budget does not adjust for likely caseload declines.
Figure 6
State Health Programs Affected or Potentially Affected by the ACAa
|
Program
|
Major Eligibility Criteriab
|
Description of Services
|
|
Prostate Cancer Treatment Program
|
- Age 18 or older.
- Income up to 200 percent FPL.
- No other health coverage.
|
Prostate cancer treatment, patient education, and case management/patient navigation.
|
|
Every Woman Counts
|
- Female.
- Income up to 200 percent FPL.
- Services not covered by health coverage or coverage has high deductible/copayment.
|
Comprehensive breast and cervical cancer screening and diagnostic services, clinical follow–up, and tailored health eduction.
|
|
Breast and Cervical Cancer Treatment Program
|
- In need of treatment for breast or cervical cancer.
- Income up to 200 percent FPL.
- No other health insurance.
- State–only program for individuals: (1) without satisfactory immigration status, (2) with high cost health insurance, and (3) females 65 years or older.
|
Full–scope coverage for individuals who meet federal eligibility criteria; cancer treatment and cancer–related services for individuals in state–only portion of the program.
|
|
Genetically Handicapped Persons Program
|
- Generally over age of 21.
- Diagnosis of an eligible genetic condition.
- No income limit.
- State–only program for Medi–Cal–ineligible persons.
|
Medically necessary services, including case management services, regardless of whether services are related to qualifying medical condition.
|
|
Major Risk Medical Insurance Program
|
- Persons unable to obtain private health insurance because of a pre–existing medical condition.
|
Health coverage, including preventative care, hospital care, physician visits, and drugs.
|
|
Access for Infants and Mothers Program
|
- Pregnant women.
- Income 200 percent to 300 percent FPL.
- No health coverage or coverage has maternity–only deductible or copay greater than $500.
|
Comprehensive benefits, including pregnancy and non–pregnancy related services.
|
|
AIDS Drug Assistance Program
|
- HIV–infected.
- Over age 18.
- Income up to $50,000.
- Lack health coverage that covers the medications.
|
HIV/AIDS medications.
|
|
Medi–Cal 200 Percent FPL Pregnant Women
|
- Pregnant women.
- Income at or below 208 percent FPL.
|
Pregnancy related and 60–day post partum services.e
|
|
Medi–Cal Medically Needy Share–of–Cost Families
|
- Pregnant women, parent/caretaker relatives, and children.
- No income limit, but income determines share–of–cost amount.
- Asset test.
|
Full–scope Medi–Cal once share–of–cost has been met.
|
|
Family Planning, Access, Care, and Treatment
|
- Income up to 200 percent FPL.
- No other source of health care coverage for family planning, or meet other specified criteria.
|
Family planning and reproductive health services.
|
|
California Children’s Services (CCS)c
|
- Under age 21.
- Diagnosed with CCS–eligible medical condition.
- State–only program for children ineligible for Medi–Cal with family income less than $40,000 per year or estimated annual cost of care that exceeds 20 percent of family income.
|
Pediatric specialty and subspecialty health care, case management, and care coordination; school–based therapy services available regardless of family income.
|
|
Qualified aliens inside the five–year bard
|
- Qualified aliens who otherwise meet Medi–Cal eligibility requirements, but who have been legally residing for less than five years and, thus, do not qualify for federal matching funds.
|
Full–scope Medi–Cal .
|
Many of the major ACA changes only recently went into effect and the magnitude of their effects on caseloads in these optional and state–only health programs are highly uncertain. Some of these programs serve populations that are ineligible for Medi–Cal or subsidized insurance offered through Covered California. However, there will likely be at least minor caseload reductions in many of these programs that are not accounted for in the budget plan. The Department of Finance (DOF) indicated in meetings with legislative staff that it intends to review the impact ACA has on caseload and utilization levels for these programs in the fall of 2014 as part of its 2015–16 budget development process. The DOF also indicated that more complete caseload and utilization data will be available in the latter half of 2014 that will better inform any proposals DOF puts forward to modify these existing state–only programs to account for the impact of ACA implementation. Under this approach, 2014–15 caseload and budgeted funds would be the basis for future discussions about whether to modify these programs.
Recommend Legislature Direct Administration to Report on Effects of ACA on Other State Health Programs. We recommend the Legislature direct the administration to report in budget hearings on the following: (1) the existing state health programs that are likely to experience caseload declines under ACA; (2) factors that would limit any potential decline in caseload and costs in these programs, such as a substantial portion of enrollees who continue to be ineligible for Medi–Cal or subsidized coverage through Covered California; and (3) the administration’s timeline for making adjustments to the budgets of these programs. With this information, the Legislature can better assess potential caseload decreases in these programs under the ACA and potentially adjust the budgets for these programs accordingly.
Pregnancy–Only Proposal Has Merit, but Some Details Remain Unclear
Currently, certain pregnant women up to 208 percent FPL qualify for pregnancy–only Medi–Cal coverage—which includes only services related to a woman’s pregnancy, rather than full–scope Medi–Cal coverage. The Governor’s pregnancy–only proposal has two main components: (1) shifting certain pregnant women between 109 percent and 208 percent FPL from Medi–Cal pregnancy–only coverage to coverage offered through Covered California and paying for “wrap–around” coverage and (2) providing full–scope coverage to pregnant women up to 109 percent FPL who currently receive pregnancy–only coverage. Pregnant women with incomes between 109 percent FPL and 208 percent FPL would have the option to enroll in federally subsidized coverage from plans through Covered California that provide broad benefits, and Medi–Cal would pay for their premiums, cost–sharing, and certain pregnancy–related supplemental services—also known as wrap around coverage. The proposal caps the amount of wrap–around premiums and cost–sharing that Medi–Cal would pay to the amount that would cover all beneficiary premiums and cost–sharing for the second lowest cost “silver” plan. Thus, women in this income band would have the option to choose any plan on the Exchange, but Medi–Cal would not cover all of the costs of more expensive plan options.
In our view, both components of the Governor’s proposal have merit, but some aspects of the proposal remain unclear. Below, we discuss the primary merits of the proposal and identify some key aspects of the proposal that remain unclear at the time of this analysis.
Shift Would Likely Reduce General Fund Spending, While Potentially Providing More Generous Benefits. The proposal to shift certain pregnant women from pregnancy–only Medi–Cal to Covered California would potentially enhance the scope of services available to these pregnant women. Pregnant women would have the option to receive comprehensive coverage from plans offered through Covered California, while maintaining certain wrap–around services that are available in Medi–Cal, such as dental services and access to certain perinatal specialists. In addition, since the women would qualify for federally subsidized coverage through Covered California, the proposal would generate state General Fund savings by leveraging federal subsidies to pay for a large portion of costs that were previously covered by Medi–Cal. For example, most of the costs for these pregnant women—such as costs for most perinatal visits and labor and delivery—would be covered by the plan obtained through Covered California, instead of the Medi–Cal Program. The state would only pay the relatively minor costs of the wrap–around coverage for these women. The administration estimates that the shift would reduce state General Fund spending by about $17 million in 2014–15.
Full–Scope Coverage Would Eliminate Coverage Inconsistencies for Pregnant Women. Under current law, some childless women applying for Medi–Cal would qualify through the optional expansion and receive full–scope Medi–Cal coverage. If a woman becomes pregnant while enrolled in Medi–Cal, she would be allowed to remain in the new adult group and continue to receive full–scope coverage. However, a woman with the same income who applies for Medi–Cal at the time she is pregnant would be eligible for pregnancy–only coverage. The Governor’s proposal to provide full–scope coverage to pregnant women below 109 percent FPL would make the scope of covered services for pregnant women in Medi–Cal consistent, regardless of whether the woman became pregnant before or after applying for Medi–Cal. The administration assumes no additional cost associated with providing full–scope—instead of pregnancy–only—coverage to pregnant women below 109 percent FPL.
Some Details of Proposal Remain Unclear. The Governor’s proposal has merit in concept because it would expand the scope of coverage available to certain pregnant women in Medi–Cal, make the scope of coverage more consistent for pregnant women who enter the program at different times, and at the same time reduce state General Fund costs. However, some details of the Governor’s proposal remain unclear at the time of this analysis, including:
- Differences in Covered Services and Costs Between Full–Scope and Pregnancy–Only Coverage. The specific differences in covered services between full–scope and pregnancy–only coverage are still unclear. The administration estimates no additional costs associated with providing full–scope coverage instead of pregnancy–only coverage—an estimate that is based on the assumption that there are no significant differences in coverage. However, it has not provided the basis for this assumption. While it is likely that the differences in covered services are relatively minor, full–scope coverage may result in the state paying for some additional services for pregnant women and, thereby, result in additional costs that have not been accounted for in the Governor’s budget.
- Continuity of Coverage and Plan Choice. The specific options that would be available to women to remain in the same plan and continue to receive care from the same physician under this proposal are uncertain.
Recommend the Legislature Direct the Administration to Clarify Details of Pregnancy–Only Proposal. While we believe the Governor’s pregnancy–only proposal has merit, there are some details that remain unclear. We recommend the Legislature direct the administration to clarify the details of this proposal, including (1) the differences in covered services between full–scope Medi–Cal and pregnancy–only Medi–Cal, and (2) continuity of coverage and plan choice for individuals moving between Medi–Cal and Covered California. With more complete information, the Legislature can more accurately: (1) assess how this proposal will affect coverage for certain pregnant women on Medi–Cal, (2) evaluate whether the administration’s estimated fiscal effects are appropriate, and (3) identify potential modifications to the proposal.
The ACA has resulted in major changes to the Medi–Cal Program and many other aspects of health care in California. Now that many of the major changes are being implemented, the Legislature will still need to provide oversight of ACA implementation, as well as shift its attention to the future of Medi–Cal and other state health programs. Below, we discuss some of the issues that we believe should be priorities for future legislative consideration.
The Future of Other State Health Programs Under the ACA. As shown in Figure 6, the state currently administers several other health programs that are relatively small compared to the Medi–Cal Program. Many of these other programs provide health care to targeted groups of individuals, often with specific medical conditions. Some of the individuals who currently qualify for these other programs would be newly eligible for Medi–Cal or subsidized coverage through Covered California.
The Legislature may want to consider the future of some of these programs and how they fit into the broader system of coverage established under the ACA. Last year, the administration publicly indicated its interest in discussing potential changes to some of these programs. As a result, options to restrict individuals from enrolling in programs such as ADAP, GHPP, and BCCPT if they were also eligible for Medi–Cal or subsidized coverage through Covered California were discussed in a budget subcommittee last year. While these changes were never officially proposed by the administration or adopted by the Legislature, in our view, the Legislature should consider similar or alternative options to leverage new sources of coverage to reduce costs in some of these programs. For example, the Legislature may want to consider opportunities to shift individuals into subsidized Covered California plans while offering wrap–around coverage—similar to the Governor’s pregnancy–only proposal discussed above.
Any potential modifications to these programs should be thoroughly vetted, as many of the programs serve vulnerable populations with acute health care needs. Some key issues the Legislature may want to consider as it weighs the future of these programs include:
- Need for Services. The Legislature should seek to clarify which services and benefits being provided by these programs are also provided in Medi–Cal or through Covered California plans and which services are only available in these programs. The specialized services offered by these programs may not be available elsewhere, and enrollees who are not eligible for full–scope Medi–Cal or Covered California plans, such as undocumented immigrants, may not be able to obtain these services if the programs are eliminated.
- Federal Requirements. The Legislature should seek to clarify federal requirements and restrictions that limit the state’s options for modifying these programs. For example, several of these programs are subject to federal maintenance–of–effort requirements that limit the state’s ability to modify the programs.
Once these factors were well understood, the Legislature could identify options to modify some of these programs in ways that leverage federal funding to offset state costs and comply with federal requirements. This process would also help identify the key benefits and services provided by these programs that the Legislature would like to preserve or possibly enhance.
Opportunities to Leverage Federal Funds to Improve Program Outcomes. The state’s actuaries develop a range of potential capitation rates that could be paid to Medi–Cal managed care plans that reflect various assumptions about factors affecting future plan costs—also known as the “rate range.” Generally, the state pays Medi–Cal managed care plans at the lower bound of the rate range. However, through 2016, the state can leverage the 100 percent federal match to pay rates for newly eligible populations at the upper bound of the rate range. This gives the state flexibility to pay higher rates to managed care plans for certain beneficiaries at no additional cost to the state.
As part of the changes made to 1991 health realignment last year, the Legislature determined how it would like to use a portion of the rate range flexibility—higher payments to county hospitals. The Legislature required that plans in counties with county hospitals use 75 percent of the difference between the lower bound and the upper bound of the rate range for newly eligible populations to increase managed care payments to those hospitals. At the time of this analysis, it is still unclear whether the remaining 25 percent of the rate range will be paid to plans in public hospital counties and whether any of the rate range will be paid to plans in other counties. The administration is currently in discussions with plans about whether and how the remaining rate range will be used.
The Legislature should begin to identify key activities and outcomes that it would like to achieve in Medi–Cal managed care and explore opportunities to use the rate range flexibility to promote those activities and outcomes. For example, there may be opportunities to leverage the rate range to promote improvements in managed care quality, access, and/or data reporting that are priorities for the Legislature. The Legislature should also bear in mind that the 100 percent federal match is temporary. Therefore, any ongoing commitment to activities financed through the rate range flexibility would be partially financed with state funds in future years as the federal match for the newly eligible population phases down.
Measuring and Monitoring Access to Care in Medi–Cal Managed Care. Access to care and provider network adequacy in the Medi–Cal Program is an important issue for the Legislature to monitor and oversee. The significant increase in Medi–Cal enrollment under the ACA creates additional demand for health care services from providers treating Medi–Cal patients. Most of the additional services will be provided by managed care plans and their contracted provider networks. If these provider networks do not have sufficient capacity to meet the increased demand, then beneficiaries may have difficulty accessing necessary health care services in a timely manner. We believe the Legislature should focus a significant amount of its oversight and monitoring efforts on access to care in Medi–Cal managed care. We provide more information on issues related to monitoring access to care in the “Medi–Cal Payment Reductions and Access to Care” section that immediately follows.
We do not recommend any specific adjustments to ACA–related fiscal estimates included in the budget at this time. However, we recommend the Legislature direct the administration to report on certain fiscal effects associated with the ACA that are not accounted for in the budget. We also recommend the Legislature direct the administration to clarify certain details of the Medi–Cal pregnancy–only proposal. Finally, we identify a few fiscal and policy issues that we think should be priorities for the Legislature to consider as the state implements the ACA. These issues include the future of other state health programs, opportunities to leverage federal funds to improve program outcomes, and measuring and monitoring access to care in Medi–Cal managed care.
Medi–Cal Payment Reductions And Access to Care
Chapter 3, Statutes of 2011 (AB 97, Committee on Budget), authorizes DHCS to reduce Medi–Cal FFS payments to providers for certain services by up to 10 percent, and to reduce capitation payments to Medi–Cal managed care plans by a related amount. The Legislature adopted Chapter 3 as part of a package of expenditure–related solutions to address the state’s 2011–12 budget problem. However, the Legislature has expressed concern that these reductions may impede beneficiaries’ access to services, and—as the state’s fiscal condition improves—has shown interest in restoring Medi–Cal payments that were reduced under Chapter 3.
This analysis begins by summarizing the state’s current approach to implementing the Chapter 3 reductions, including the Governor’s 2014–15 budget proposal. We next evaluate this approach taking into account (1) the quality and relevance of access monitoring information that is presently available, and (2) the distinction between—and relative significance of—access in managed care versus FFS. Lastly, we lay out issues for the Legislature to consider when deliberating over whether to restore funding that was reduced with the payment reductions, as well as recommendations for how the Legislature should proceed on the broader subject of access to care in Medi–Cal.
Chapter 3 authorizes (1) reductions in certain Medi–Cal FFS provider payments by up to 10 percent and (2) a roughly proportionate decrease to managed care capitation payments known as “actuarially equivalent” reductions. These reductions originally applied to a wide range of providers and services, including (1) outpatient services provided by physician and clinics, (2) institutional providers such as distinct–part nursing facilities and intermediate care facilities for the developmentally disabled, (3) ancillary services such as laboratory tests and medical transportation, and (4) retailers of medical goods such as pharmacies and medical equipment suppliers. Chapter 3 allows DHCS discretion to adjust these reductions as necessary to comply with federal Medicaid requirements, including those related to beneficiary access that we discuss later. Until recently, federal court injunctions prevented the state from implementing many of these reductions. In June 2013, the injunctions were lifted, giving the state authority to (1) apply the reductions to current and future payments to providers on an ongoing basis and (2) retroactively recoup the reductions from past payments that were made to providers during the period in which the injunctions were in effect. Since the 2013–14 budget was enacted, several types of providers and services have been exempted from the ongoing payment reductions through either administrative decisions by the DHCS or recently enacted legislation.
The Governor’s budget proposes to exempt certain classes of providers and services from the retroactive recoupments, and includes $36 million in increased General Fund expenditures associated with this proposal. Specifically, the budget proposes that the following providers and services be exempted from the retroactive recoupments: (1) physicians and clinics, (2) certain high–cost drugs, (3) dental services, (4) intermediate care facilities for the developmentally disabled, and (5) medical transportation. Because the recoupments are otherwise scheduled to take place over several years, the total General Fund cost of the proposal over this multiyear period is estimated to be $218 million. The administration has stated that while federal approval is required to forgive the recoupments, no statutory changes are necessary.
The budget assumes that the state will continue to implement reductions to payments to providers and services that have not been legislatively or administratively exempted from ongoing reductions. The budget assumes that these ongoing reductions will result in General Fund savings of $245 million in 2014–15.
The state required federal approval to implement the FFS reductions specified in Chapter 3. As part of the conditions of this approval, DHCS agreed to analyze and regularly monitor access to care in the FFS system. The administration has indicated that its FFS access monitoring continues to inform its decisions to exempt specific providers from the reductions, including the decisions reflected in the Governor’s budget. Below we describe the federal requirements for analyzing and monitoring FFS access with respect to Chapter 3.
Federal “Equal Access” Provision Governs FFS Provider Payments. Generally, states are required to obtain federal approval for reducing provider payment rates in their FFS Medicaid programs. The Centers for Medicare and Medicaid Services (CMS) reviews states’ proposed reductions to ensure they comply with federal Medicaid law—including the requirement that FFS payments be sufficient to enlist enough providers so that care and services are available to Medicaid beneficiaries to at least the same extent that they are available to the general population in a geographic area. This requirement, often referred to as the equal access provision, only applies to provider payments and services in the FFS system—it does not apply to managed care. (Later, we discuss separate requirements that govern access considerations in Medi–Cal managed care.)
Proposed Federal Regulations to Implement Equal Access Provision. Until 2011, the federal government provided little regulatory guidance on how states should comply with the Medicaid equal access provision. Shortly after passage of Chapter 3, CMS proposed new regulations that, if adopted, would require states to conduct reviews of beneficiary access to services in their FFS systems. Under the draft regulations, a state seeking to reduce FFS provider payment rates for a service is required to submit the following materials to CMS.
- A baseline analysis of FFS access to the affected service, conducted within 12 months prior to submitting the proposed reductions.
- A plan for continually monitoring FFS access to the service after implementing the proposed reductions.
There is no state law explicitly specifying the measures that DHCS must collect and analyze to monitor access to care provided through FFS. Moreover, rather than prescribe specific metrics or activities to implement the equal access provision, CMS’ proposed rule gives states flexibility to develop their own approaches to conducting FFS access reviews in their Medicaid programs. States’ approaches can take various forms, as long as they conform to a broad framework that addresses three main criteria: (1) enrollee needs, (2) availability of care and providers, and (3) utilization of services. As a result, the administration’s efforts to monitor FFS access—per its agreement with CMS for implementing the Chapter 3 reductions—have proceeded within a loose regulatory structure at the federal level. To meet CMS’ expectations as reflected in the proposed rule, DHCS produced baseline analyses and a monitoring plan for Medi–Cal services that would be subject to FFS provider payment reductions under Chapter 3.
DHCS Baseline Analyses. The DHCS submitted six baseline analyses of utilization and provider availability for different categories of services in the FFS system. (For example, one analysis focused on ambulatory care provided by physicians and clinics.) The analyses generally relied on (1) FFS claims data, and (2) DHCS’s “provider master file”—a record of providers who have billed Medi–Cal for services provided through FFS—to measure utilization and provider availability respectively. Most of the analyses reported annual summary statistics from these administrative data for the period of 2007 through 2009. To varying degrees, the analyses stratified these data by geography (such as counties and urban regions versus rural regions) and enrollee category (such as families and children versus SPDs). For some services, DHCS also compared utilization rates with statewide or national statistics and/or benchmarks.
For most services, the analyses concluded (1) FFS access was adequate for all enrollees throughout the study period, and therefore (2) the state could reduce FFS payments for these services without negatively impacting access. There were several exceptions. For example, the ambulatory care analysis reported that in FFS Medi–Cal, only half of children above the age of five received an annual physician visit, leading DHCS to exempt pediatric services from the payment reductions.
DHCS Monitoring Plan. The DHCS’s monitoring plan outlines 23 specific measures related to FFS access that the department would collect and report on an ongoing basis. Under the plan, DHCS would report four of these measures quarterly as part of an “early warning” system for detecting and responding to access problems in the FFS system. The four quarterly measures are: (1) provider participation rates, (2) service utilization rates, (3) beneficiary calls to a FFS helpline established by DHCS, and (4) changes in FFS enrollment. The DHCS would report the remaining 19 measures—which relate variously to provider availability, service use, and health care outcomes—annually or biannually.
At the time of this analysis, DHCS had made public the following sets of documents related to Chapter 3 access monitoring for the FFS system: (1) the baseline analyses originally submitted to CMS and (2) quarterly monitoring reports of the four early–warning system measures.
DHCS Does Not Report on FFS Access to Dental Services. Neither the provider participation reports nor service utilization reports issued each quarter contain any information on dental services provided through FFS Medi–Cal. We note Medi–Cal dental services are (1) targeted by the Chapter 3 reductions, (2) are still mostly provided through FFS (as discussed later), and (3) have been the subject of recent legislative concerns over access.
DHCS Has Not Published Annual Measures Outlined in Monitoring Plan. Although two– and–a–half years have transpired since CMS’ approval of DHCS’s FFS monitoring plan, the administration has yet to report on any of the plan’s 19 proposed annual or biannual measures on provider availability, service use, or health care outcomes. Among these annual measures are enrollee–to–dentist ratios and the percentage of children with at least one dental visit. Again, these are measures that are potentially of interest to the Legislature, given the preponderance of dental care that is still covered under FFS Medi–Cal.
We have reviewed DHCS’s baseline analyses and quarterly monitoring reports and come away with numerous concerns about the quality of the data, the soundness of the methodologies, and the assumptions underlying the administration’s findings on access. In our view, these concerns are sufficient to render the administration’s public reporting of very limited value for the purpose of understanding beneficiary access in the FFS system.
There are a multitude of issues that we encountered during our review of the baseline analyses and quarterly monitoring reports.We highlight our most serious concerns below.
Inflated Estimates of Available FFS Physicians. It is likely that the DHCS’s baseline analysis and quarterly monitoring reports overestimate the number of physicians who currently participate in FFS Medi–Cal. The baseline analysis’s statewide count of physicians who are “potentially accessible” to FFS Medi–Cal beneficiaries actually exceeds the total number of active and in–state physician and surgeon licenses as reported by the Medical Board of California. In all but the most recent quarterly reports on provider participation, the counts of FFS Medi–Cal physicians are nearly equal to the total number of medical licenses in the state.
These figures are implausibly high. The DHCS’s counts are based on the number of “enrolled” physicians listed in the provider master file. (Before Medi–Cal will reimburse for FFS physician services provided to a beneficiary, the physician rendering the services must first apply for a Medi–Cal provider number. Once the physician receives this number from DHCS, the physician is entered into the provider master file as an enrolled physician.) Researchers have pointed out that the provider master file likely includes physicians who have left the state, stopped practicing, or passed away. Although DHCS (1) screens the provider master file for known physicians with inactive status and (2) claims that it periodically evaluates the file for accuracy and completeness, it is unclear how frequent or thorough the data cleansing process actually is.
There are also questions regarding the internal consistency of DHCS’s approach. The DHCS’s most recent quarterly count of physicians has dropped sharply from prior quarters. Instead of listing around 100,000 physicians enrolled as Medi–Cal providers—the rough number reported in the baseline analysis and previous quarterly reports—the latest report now lists about 75,000 enrolled physicians for the most recent quarters. The report does not provide an explanation for this 25–percent downward revision. The DHCS has broadly indicated that the adjustment was due to “updates and modifications” to the provider master file, although it has not clarified the exact nature of these changes. The revision suggests the baseline analysis’ count of 100,000 enrolled physicians available to FFS Medi–Cal–only beneficiaries—which were used to justify Chapter 3 reductions to payments for physicians services—was overstated.
Flawed Construction and Interpretation of Enrollee–to–Physician Ratios. The DHCS uses the raw count of enrolled physicians as the denominator in calculating FFS enrollee–to–physician ratios. This approach implicitly assumes that every physician who has ever billed Medi–Cal for a service is a full–time equivalent who actively provides services to FFS Medi–Cal beneficiaries.
The resulting statewide ratios are as low as 15 Medi–Cal FFS beneficiaries to every enrolled physician. By comparison, the ratio of all state residents—more than half of whom have private health insurance—to the total number of licensed physicians in the state is around 377 to 1. The reason behind this disparity is simple. Because (1) DHCS’s reported count of enrolled physicians is close to the total number of state–licensed physicians, and (2) the number of FFS Medi–Cal enrollees is less than three percent of the total state population, the ratio for FFS Medi–Cal enrollees is arithmetically much lower than the ratio for the state population as a whole.
The DHCS concludes that the FFS enrollee ratio compares “favorably” to the statewide population–to–provider ratio—implying that FFS Medi–Cal beneficiaries enjoy equal or perhaps better access to care than the general population. Yet, for the purpose of measuring access to physician services, any attempt to make an “apples–to–apples” comparison between these two ratios is highly misleading. In its discussion of the proposed rule to implement the equal access provision, CMS states that “in order to contribute to beneficiary access, it is significant to know whether enrolled providers have ‘open panels’ which means that they are accepting Medicaid patients.”
The DHCS’s reports do not attempt to account for the portion of enrolled providers who have open Medi–Cal panels. Yet CMS makes a compelling point. To draw any meaningful inference on patient access from the per–capita supply of providers, it is important to have some notion of the average willingness and capacity of these providers to serve additional patients. This is why per–capita ratios typically specify full–time equivalents as the unit of measurement for provider availability. It is possible that many enrolled physicians on the provider master file may have treated and billed for the occasional Medi–Cal patient in the past—and/or agree to continue seeing the Medi–Cal patients who are already part of their current practice—yet generally choose not to open their practice regularly to additional Medi–Cal patients.
A 2008 study conducted by researchers at the University of California, San Francisco (UCSF) reported that about 70 percent of physicians in the state currently have at least one Medi–Cal patient (FFS or managed care) in their practice, and about 60 percent were accepting new Medi–Cal patients. The corresponding figures were 92 percent and 90 percent for private insured patients, and 80 percent and 70 percent for Medicare patients. Moreover, the study found Medi–Cal patients were concentrated within a small share of practices, with 25 percent of physicians providing care for 80 percent of Medi–Cal patients. Taken together, these findings seriously question the validity of (1) treating each enrolled provider in the master file as a full–time equivalent and (2) using the resulting ratios to compare beneficiary access with other populations—particularly privately insured patients. (For information on the UCSF study methodology, see nearby box.)
The findings from the University of California, San Francisco study were based on physicians’ written responses to survey questions that asked about their patient mix. The researchers received permission from the Medical Board of California to append their survey questionnaire to the regular application that physicians are required to complete to renew their medical licenses biannually. The response rate for the survey was 60 percent, and the researchers weighted the responses in proportion to the characteristics of the total physician population.
The Department of Health Care Services has previously held the position that its administrative data are more reliable than self–reported survey responses. However, the discussion of the draft regulations issued by the Centers for Medicare and Medicaid Services indicates that surveys may be the only practical means of estimating the number of providers with open Medicaid panels.
The DHCS’s quarterly monitoring reports for provider participation only cover physician supply. The reports state that physicians represent the “epicenter” of the health care delivery system—for example, providing a gateway to other services through prescriptions and referrals. While we agree with the concept of prioritizing physician availability in an early warning system for monitoring access, we are troubled by the administration’s execution of this concept. The DHCS’s data sources for participating physician counts do not appear fully credible, and the department’s analyses and interpretation of that data are highly problematic. As a result, the baseline analysis and monitoring reports convey little useful information to the Legislature about physician availability in the FFS system.
Figure 7 displays a subset of the FFS provider categories that—by administrative decision or statute—have been partially or fully exempted from ongoing Chapter 3 reductions. (The exemptions for dental pediatric surgery centers are still pending federal approval.)
Figure 7
Subset of Provider Categories Exempted From Ongoing Chapter 3 Reductions
|
Effective Date of Exemption
|
Provider/Service Category
|
Baseline Analysis or Quarterly FFS Monitoring Cited in Decision to Exempt?
|
|
1–Jun–11
|
Pediatric services.
|
Yes—baseline analysis found only half of children in FFS Medi–Cal received recommended annual pediatric visit.
|
|
1–Jun–11
|
Adult day health care outside Southern California and San Francisco metropolitan areas.
|
Yes—baseline analysis found that supply of providers was relatively low outside these areas.
|
|
1–Jun–11
|
Hospital outpatient services.
|
No.
|
|
31–Mar–12
|
Certain drugs and pharmacy providers.
|
No—DHCS cited study of pharmacy invoices indicating that cuts would reduce FFS payments to below providers’ acquisition cost for drugs.
|
|
Rural/frontier
1–Sep–13
All others 1–Oct–13
|
Distinct–part nursing facilities.
|
No.
|
|
Nonprofit 1–Sep–13
For–profit 1–Dec–13
|
Dental pediatric surgery centers.
|
No—DHCS cited “significant volume” of pediatric patients served by centers.
|
For a few of the services exempted after June 2011, the administration has provided relatively clear explanations for its decisions to grant exemptions. For example, in its decisions to exempt certain specialty drugs from the pharmacy reductions, DHCS cited its review of provider invoices showing that the reductions would lower FFS reimbursement for these drugs to less than the drugs’ acquisition cost for many pharmacies. Yet the administration’s reasoning for other services has been more nebulous. For example, when asked about the most recent decision to exempt dental pediatric surgery centers, DHCS has referenced an internal tracking system that captures more “granular” measures than the public quarterly monitoring system.
Chapter 3 declares DHCS has “unique expertise that can inform decisions that set or adjust reimbursement methodologies and levels consistent with requirements of federal law.” Because the FFS monitoring results that DHCS has made public have proven both unreliable and of limited if any value for the actual decisions being made, it is unclear how the administration interprets and implements its requirement to meet the equal access provision under Chapter 3. Simply stating—as the administration has done—that there is no single factor or formula in determining whether to exempt providers does not clarify DHCS’s decision process.
To date, the state’s approach to overseeing Chapter 3 implementation has concentrated on the effect it has had on access to providers and whether to exempt specific categories of providers from reductions. For some services that are still mainly provided through FFS—such as dental services and long–term care—this approach generally encompasses the relevant set of issues. However, as discussed later, this approach only directly addresses access issues within the FFS system, and does not address access issues in Medi–Cal managed care where the majority of beneficiaries receive services.
Early Stages of Chapter3 Implementation Focused on FFS Issues. Only the FFS reductions under Chapter 3 required direct approval from the federal government. As a result, DHCS’ baseline analyses and monitoring plan only covered the state’s FFS system to meet conditions for federal approval. Despite their various problems outlined earlier, the baseline analyses and monitoring reports remain the most recognizable components of the administration’s response to access concerns under Chapter 3. The court injunctions that formed the backdrop for further developments in Chapter 3—including the Legislature’s interest in revisiting the reductions—extensively cited flaws in the FFS baseline analyses, and only applied to specific FFS reductions.
Managed care has overtaken and surpassed FFS as the primary Medi–Cal service delivery system. The amount of attention devoted to FFS issues related to Chapter 3 is understandable. However, it is increasingly important to exercise oversight over access to services in Medi–Cal managed care, given the state’s growing reliance on managed care to cover more complex groups of beneficiaries and services.
Majority of Medi–Cal Beneficiaries Are Mandatorily Enrolled in Managed Care . . . Presently, the vast majority of Medi–Cal beneficiaries with full–scope coverage are mandatorily enrolled in managed care to receive most medical benefits, including primary and specialty care. (Beneficiaries with full–scope coverage are entitled to receive all medically necessary services that are included in the state’s benefit package.) These populations include:
- Families and children in all 58 counties.
- Newly eligible individuals under the optional expansion—mostly childless adults—in all 58 counties.
- Medi–Cal–only SPDs in 30 counties.
During 2014–15, Medi–Cal–only SPDs will also be mandatorily enrolled in managed care in the 28 rural counties where managed care has most recently been established. In the eight CCI demonstration counties—which are among the most populous in the state, such as Los Angeles County—all SPDs, including dual eligibles, will be enrolled in Medi–Cal managed care to receive LTSS such as In–Home Supportive Services and skilled nursing care. Altogether, managed care enrollees will account for more than 70 percent of the entire Medi–Cal caseload projected for 2014–15.
. . .With Significant Enrollment Growth in Recent and Coming Years. . . Figure 8 indicates that approximately 2.7 million, or 36 percent of Medi–Cal managed care enrollees in 2014–15 will be relative newcomers who (1) have transitioned to Medi–Cal managed care within the past three years, (2) are currently in the process of enrollment, or (3) will begin to transition over the next several months. A large portion of the recent arrivals are children formerly covered under HFP. Other incoming populations—beneficiaries in the 28 rural counties, Medi–Cal–only SPDs in 16 counties, and dual eligibles in the 8 CCI counties—previously received their Medi–Cal benefits through FFS. Finally, the optional expansion accounts for 46 percent of the expected managed care influx during 2013–14 and 2014–15. Overall, enrollment in Medi–Cal managed care is projected to have increased by around 60 percent between 2011–12 and 2014–15.
Figure 8
Recent and Upcoming Transitions to Medi–Cal Managed Care Through 2014–15
|
Transition
|
Approximate Enrollment
|
Time Frame
|
|
Medi–Cal–only SPDs
|
240,000
|
June 2011 – May 2012
|
|
HFP to Medi–Cal
|
850,000
|
January – November 2013
|
|
Rural county expansion
|
400,000a
|
September – November 2013
|
|
ACA optional expansion
|
780,000
|
Beginning January 2014
|
|
CCI dual eligibles
|
450,000b
|
Beginning April 2014
|
|
Total
|
2,720,000
|
|
. . .And Increasing Complexity of Beneficiary Needs and Services. Medi–Cal managed care plans will contend with the access implications of (1) extending coverage to populations who face greater challenges obtaining medically necessary services and (2) providing many new benefits to meet the needs of SPDs and dual eligibles that the plans generally did not previously provide. For instance, the Medi–Cal–only SPDs have a high prevalence of complex medical conditions that require referrals to specialists—a category of providers whom historically have been harder for Medi–Cal plans to recruit and retain in their networks. Due to the low supply and geographical dispersion of providers in many rural areas, plans that begin providing coverage in the 28 rural counties may encounter difficulties building networks with sufficient providers in general, and specialists in particular. While beneficiaries who gain coverage under the optional expansion are expected to be healthier on average than the existing Medi–Cal population, the earliest enrollees are likely to be disproportionately represented by the higher–needs segment of the newly eligible, such as individuals with complex and urgent medical conditions who formerly received county indigent health care. Finally, in 2014–15, Medi–Cal managed care plans are required to cover additional services and meet new network standards for contracting with providers of these services, including: (1) enhanced mental health and substance use disorder services in all 58 counties, and (2) LTSS in the 8 CCI counties.
Remaining FFS Population. The remaining population who receive most of their Medi–Cal benefits through FFS will consist primarily of (1) undocumented immigrants eligible for only restricted–scope coverage of emergency and pregnancy–related services, (2) dual eligibles outside the CCI counties who are primarily covered under Medicare for their medical benefits, and (3) the small portion of beneficiaries who are granted special medical exemptions from mandatory managed care enrollment.
Medi–Cal provides dental services through two service models: FFS, also known as Denti–Cal, and dental managed care (DMC). Currently, only two counties—Sacramento and Los Angeles—offer DMC while all other counties offer Denti–Cal. In Sacramento, beneficiaries are mandatorily enrolled in DMC whereas in Los Angeles, enrollment into DMC is voluntary, and if beneficiaries do not enroll in DMC, they are automatically enrolled in Denti–Cal. Currently, about 6.5 million beneficiaries are enrolled in Denti–Cal and about 500,000 beneficiaries are enrolled in DMC. The number of Medi–Cal beneficiaries with dental coverage is expected to grow as coverage for adult dental benefits is partially restored toward the end of 2013–14 and as Medi–Cal eligibility is expanded through ACA. As with the current population of children who receive dental coverage under Medi–Cal, the vast majority of these adult beneficiaries will be served by Denti–Cal.
In concept, shifting beneficiaries and services from FFS to managed care should also improve the state’s monitoring of access to care in the Medi–Cal Program. As discussed earlier, there are no state statutory guidelines for interpreting adequate access in FFS Medi–Cal, other than compliance with the broad equal access provision of federal Medicaid law. Even if FFS access standards were well–developed, no outside entities such as managed care plans exist for the state to hold accountable to such standards. The DHCS is responsible for both directly purchasing and ensuring access to services in FFS Medi–Cal.
In contrast, under Medi–Cal managed care, the state delegates to managed care plans the responsibility for making covered services available and accessible to Medi–Cal beneficiaries, thereby imposing a set of enforceable obligations on specific outside entities. Moreover, the state draws much of its monitoring framework from an existing and comprehensive body of rules, as described below.
Two Departments Monitor Statutory and Contractual Access Requirements for Medi–Cal Managed Care. Medi–Cal managed care plans are overseen by two departments: DHCS and the Department of Managed Health Care (DMHC). The DMHC is responsible for ensuring plans comply with the Knox–Keene Health Care Service Plan Act of 1975 (Knox–Keene Act)—the regulatory structure for most managed care plans in California, including Medi–Cal plans. The DHCS contracts with the plans to provide coverage to Medi–Cal enrollees. Accordingly, DHCS is responsible for ensuring plans meet the Medi–Cal contractual requirements, which include Knox–Keene Act standards and additional requirements that are usually based on federal and state Medicaid standards. For more information on the state’s system for monitoring access in Medi–Cal managed care, see the box below.
Medi–Cal Managed Care Access Monitoring
Both the Knox–Keene Act and Medi–Cal contracts contain a variety of requirements intended to ensure that managed care plans are providing enrollees with adequate access to care. For example, regulations implementing the Knox–Keene Act establish three main categories of standards that plans must follow to demonstrate adequate access. These are (1) minimum ratios of full–time equivalent providers to enrollees, (2) maximum distances between primary care providers and enrollees’ residences and workplaces, and (3) limits on enrollee wait times for appointment and referrals. (The first two categories of requirements are often referred to as “network adequacy” standards and geographic standards, while the third category is a set of recently developed regulations known as “timely access” standards.) The Department of Health Care Services monitors additional contract–specific requirements related to access, often with the Department of Managed Health Care’s assistance under interagency agreements. These additional requirements may account for—among other areas—the number of network providers who are not accepting new patients, the location and types of specialists within the network (with specific requirements that depend on the characteristics and health needs of the plan’s enrollees), and coverage of out–of–network services that the plan may be unable to provide.
Both departments conduct various activities to monitor access to care, including quarterly reviews of provider network data submitted by plans, help lines that may identify early access problems through beneficiary complaints, and periodic on–site audits of plans’ operations.
Three Stages of Managed Care Access Monitoring. Generally, when a new population of beneficiaries is mandatorily enrolled in Medi–Cal managed care, the state’s activities to ensure adequate access for those beneficiaries occur in three main stages.
- Readiness Review. Prior to enrolling any beneficiaries in managed care plans, the state assesses the plans’ preparations to meet access requirements, including the expansion of their provider networks to accommodate incoming enrollees.
- Transition Monitoring. The state monitors the actual process of enrollment with an emphasis on “continuity–of–care” issues, such as the ability of beneficiaries to access their preferred providers.
- Ongoing Monitoring. After the transition is complete and enrollment has stabilized, the state monitors each plan for continuing compliance with statutory and contractual requirements to provide accessible care, and in doing so may investigate issues such as substantial changes to plans’ provider networks.
For Medi–Cal managed care to deliver on its conceptual promise enabling the state to better monitor access to care, two layers of accountability are necessary. First, contracting plans are accountable to DHCS in providing accessible care to their enrollees. Second, the administration must itself be accountable to the Legislature in executing legislative intent to ensure adequate access in managed care. Specifically, at each of the above three stages, the Legislature needs evidence that (1) the administration is carrying out monitoring activities in good faith and (2) the access measures themselves are meaningful.
Questions About Ongoing Monitoring of Managed Care Access Remain. Since the documentation of various problems that occurred during the Medi–Cal–only SPD transition, the Legislature has increased its oversight presence at the readiness review stage, such as the recent hearing on pre–implementation issues in CCI. The Legislature has also made efforts to become more involved during the transition stage, such as requesting DHCS to provide network adequacy updates during each phase of the HFP transition. While access monitoring at these first two stages is important for the well–being of new enrollees, ongoing monitoring is crucial for long–term success in ensuring beneficiary access in managed care.
A detailed evaluation of the state’s current efforts to monitor ongoing access in Medi–Cal managed care is beyond the scope of this analysis. However, we highlight two areas that we believe are deserving of greater legislative oversight.
- Statutory Access Requirements. There are questions regarding DMHC’s implementation of Knox–Keene Act standards, such as (1) how plans demonstrate timely access and (2) whether current provider–to–enrollee ratios meaningfully reflect network adequacy.
- Contractual Access Requirements. So far, DHCS and DMHC have provided only basic descriptions of how they monitor plan contract provisions that extend beyond basic Knox–Keene Act requirements, such as the adequacy of specialist networks to meet the care needs of SPDs.
Under Chapter 3, reductions to FFS trigger actuarially equivalent reductions to managed care rates. (Actuarially equivalent reductions are decreases to managed care capitation payments that are roughly proportionate to FFS reductions to provider payments.) If the administration or the Legislature exempts a provider category from a FFS reduction, then managed care plans are also exempted from the actuarially equivalent reduction. In other words, the state’s finding that an access problem exists for some service in FFS implies—without a separate assessment—that a commensurate problem exists for the same services in managed care. This assumes that under managed care, reductions that are actuarially equivalent to FFS rate cuts are also practically equivalent in terms of their impact on particular provider categories.
While the state administratively sets capitated rates paid to Medi–Cal managed care plans, it generally does not dictate the amount or structure of payments from plans to their contracted providers. (An important exception is the ACA requirement that plans pay Medicare–level rates for primary care services through the end of 2014.) This makes it difficult to determine whether or how plans pass through actuarially equivalent reductions to particular providers in their networks. Consequently, there is no guarantee that exempting specific providers from Chapter 3 would prevent plans from passing through some portion of the remaining cuts onto these providers.
On the other hand, plans may choose to absorb certain actuarially equivalent reductions. Our review of several memoranda composed by plans shortly after passage of Chapter 3 suggests that plans may apportion cuts to different providers after considering various factors—such as their existing contracts and concerns about network adequacy—rather than strictly emulate the FFS reductions that are reflected in their capitated rates. Plans may refrain from cutting contract payments, but instead attempt to weather the reductions by tightening utilization controls or more frequently denying treatment requests. This highlights the importance of the state’s ongoing monitoring system for both network adequacy and timely access in managed care.
The Chapter 3 language on “actuarially equivalent reductions” is simply a vehicle that enables actuaries to certify managed care rates reflecting an overall budget target—one proportionate to total savings from FFS reductions. Capitation, which is designed to move the state away from reimbursing for individual services, rolls the actuarially equivalent reductions into a single rate cut to each plan. There is no clear evidence that the effects of this aggregate cut, either on provider payments or on beneficiary access, will closely mirror the effects of individual FFS reductions. Even as the Legislature recognizes the growing significance of Medi–Cal managed care, the state’s main response to managed care concerns under Chapter 3—reversing actuarially equivalent reductions on a piecemeal basis—does little to directly address access to specific services in the managed care system.
At this time, we withhold recommendation on whether the Legislature should restore funding with respect to any or all of the Chapter 3 payment reductions that have not already been exempted by statute or administrative decision. As explained earlier, the only provider payments directly affected by these reductions are those administered in the FFS system. We do not have a clear picture of FFS access to any of these providers to make an analytical case for further restoring their payments.
In 2001, we observed that FFS Medi–Cal physician rates were roughly 60 percent of those of Medicare, and in many cases well below the rates paid by other health purchasers. However, the fact that FFS Medi–Cal paid lower rates than other payers was not per se a problem requiring legislative action. Rather, our concern was whether the state’s FFS payment policy was consistent with the Legislature’s goal of ensuring reasonable access to care. Due to the lack of objective data about beneficiary access, we did not have a basis for recommending further changes to FFS physician rates in 2001. (For more information, see our 2001 report, A More Rational Approach to Setting Medi–Cal Physician Rates.)
With regard to Chapter 3, we are in many ways confronted by the same data deficiencies as in 2001. While the administration has since established a FFS monitoring system, the public reporting from this system has been unsuitable for drawing meaningful conclusions about beneficiary access. We recognize that the administration has turned to other information to guide implementation of Chapter 3. However, without being privy to the details of the administration’s internal decision process, we can neither assess its quality and relevance, nor apply it to our own independent evaluation of FFS access. If the administration provides these details to the Legislature—for example, the invoice–based cost studies that were used to exempt certain specialty drugs from the pharmacy reduction—we may be able to give recommendations on the remaining reductions in a future analysis.
At the same time, we understand the Legislature’s continuing concern about access to care and how it may relate to provider payment levels. To the extent the Legislature wishes—despite the absence of reliable data on FFS access—to continue pursuing the question of whether to restore payments reduced under Chapter 3, we would suggest it keeps the following points in mind.
Reductions and Restorations Only Directly Affect Payments in FFS. There is a widely held notion that FFS rate–setting strongly and persistently influences capitated rate–setting for Medi–Cal managed care. If provider rates are too low to support adequate access in FFS, the thinking goes, then so must be the case for managed care. However, we are unaware of any compelling evidence to support this claim. According to our discussions with DHCS, the state’s provider fee schedule for FFS—which may not be regularly updated for many categories of providers and services—has little if any direct bearing on the cost assumptions used to construct managed care rates, which are updated annually. While state budgetary considerations certainly do impact capitated rate development, the overall process relies mostly on historic utilization and cost data specific to managed care plans. Finally, as discussed earlier, the structure of capitation makes the degree of plan–to–provider pass–through of reductions or restorations ambiguous.
Reversing Chapter 3 reductions will not necessarily translate into managed care plans increasing their contract payments to corresponding network providers. By the same token, keeping reductions in place will not necessarily lead to lower managed care payments for the same services. Therefore, as the Legislature weighs any options for undoing versus maintaining some of the remaining Chapter 3 reductions, it should recognize that any potential effects on access from exercising these options will mainly be felt by beneficiaries, providers, and services in the receding FFS system.
The Legislature’s future plans for addressing the broader subject of access should prioritize issues that are (1) most material to the Medi–Cal Program, (2) within the proper scope of legislative oversight, and (3) potentially amenable to policy solutions. With these principles in mind, we lay out an oversight agenda that—based on our findings—aims to make the most efficient use of the Legislature’s availability to work on access–to–care issues in Medi–Cal.
Limit Oversight of FFS Access Monitoring on Services Like Dental Care. To make any progress toward raising the quality of the administration’s public FFS access reporting, the Legislature would need to address the present lack of state standards to govern this reporting. The Legislature could take an informal approach to building greater accountability from the administration, such as requesting DHCS to report at budget hearings on strategies to improve its FFS access monitoring. However, without the force of law to guide the administration in developing such strategies, prospects for meaningful improvements in public FFS monitoring would remain dim.
Thus, the Legislature would have to codify FFS access measures and monitoring requirements in statute—requiring, for instance, DHCS to monitor the number of full–time equivalent providers per capita who are accepting new FFS Medi–Cal patients. Crafting this legislation would be a complex and lengthy undertaking, given the overall breadth and scope of access–to–care issues. To enforce these standards credibly, the Legislature would also need to become an active and informed consumer of the administration’s improved monitoring, by studying reported trends regularly and comparing its own interpretation of those trends with the administration’s.
When deciding where to invest its resources with respect to access–to–care issues, we encourage the Legislature to carefully consider (1) the time– and labor–intensive steps involved in producing and overseeing meaningful standards for FFS access monitoring, and (2) the fact that for a growing majority of Medi–Cal beneficiaries, medical and ancillary services are provided through managed care rather than FFS. To the extent the Legislature wishes to address FFS access monitoring, we suggest that it focus on the services that remain FFS benefits for most beneficiaries, such as certain long–term care services, prescription drugs that are “carved out” of managed care, and especially dental services, as described immediately below.
Dental care will remain primarily a FFS benefit for the foreseeable future—for children who are currently covered, as well as adults who will see the benefit partially restored near the end of the current year. Accordingly, we recommend the Legislature enact legislation that would create meaningful standards for monitoring Denti–Cal access. As the Legislature takes up this issue, it should require the administration to present at budget hearings on its current internal efforts for Denti–Cal monitoring. Moreover, the final legislation should direct the administration to consult experts and stakeholders in implementing the new dental reporting standards.
Focus Majority of Oversight on Managed Care Access. We recommend the Legislature refocus its future oversight priorities on monitoring the managed care system, with the exception of certain services like dental care as discussed above. While we understand the Legislature’s concern about the adequacy of individual FFS rates, the state has delegated much de facto control over provider payment policy to Medi–Cal managed care plans. As such, we recommend that the Legislature turn toward the state’s monitoring system for managed care plan, as the object of its efforts to ensure beneficiary access. Moreover, with the benefit of the state’s existing regulatory structure for managed care as a starting point, it should be easier for the Legislature to pursue lasting improvements within a shorter period for managed care access monitoring as compared to FFS.
The growth of Medi–Cal managed care over the past three years has been rapid in pace, vast in scale, and complex in scope. Compared with populations that have been enrolled in Medi–Cal managed care for decades—such as families and children in metropolitan areas—many of the newest managed care enrollees will (1) demand costlier and harder–to–find services (including benefits that are new to Medi–Cal managed care), (2) pose greater challenges to plans in making these services available and accessible, and (3) depend more crucially upon timely access to care to maintain or improve their health. Simply put, the stakes for beneficiary access have become much higher in managed care.
To assist the Legislature in making its oversight task manageable and its efforts more productive, we recommend two main areas of managed care access for the Legislature to concentrate on during 2014–15.
- Ongoing Monitoring. Most major transitions to managed care will be complete by the end of 2014–15. We recommend the Legislature take a longer–term view on access and focus on ongoing monitoring of managed care plans.
- Existing Access Standards. Within ongoing monitoring, we advise the Legislature to narrow its focus to working on the most immediate and tractable problems: the meaningfulness of existing access standards and the administration’s performance in monitoring plans’ compliance with those standards. In future and more detailed analyses, we will outline concrete steps to guide the Legislature’s work in these areas.
Finally, as the Legislature reorients its priorities to align with the reality of the expanding managed care system, it may wish to ask whether the administration has similarly modernized its management of state resources—such as the relative number of positions at DHCS currently dedicated to activities related to managed care versus FFS.
Medi–Cal Eligibility Data System (MEDS)
The ACA. In order to make health care coverage more accessible and affordable, the ACA establishes entities called Health Benefit Exchanges. Through these exchanges, individuals and small businesses can now obtain information about health insurance and purchase coverage. The California Health Benefit Exchange (also known as Covered California) funds the California Healthcare Eligibility, Enrollment and Retention System (CalHEERS) project—primarily through federal grants—to build a web–based portal designed to be a streamlined resource from which individuals and small businesses can research, compare, check their eligibility for, and purchase health coverage. The CalHEERS was designed to interface with various federal, state, and local information technology systems to perform the administrative functions necessary for the purchase of health insurance. For example, CalHEERS is required to interface with a federal data hub—a database that consolidates data from the Internal Revenue Service, Social Security Administration, and other federal entities—to assess income, citizenship, and other data necessary to determine eligibility for various ACA health coverage options.
The MEDS. The MEDS is a statewide automated database—administered by DHCS—that stores information on individuals receiving public benefits from Medi–Cal and other health and human services–related programs. The MEDS consolidates case information, including utilization and benefits data, in an environment where eligibility is determined in a decentralized manner—through county–based eligibility systems. The MEDS serves as the “system of record” for various programs, including Medi–Cal, CalWORKS, CalFresh, and the cancer detection programs. Data maintained in MEDS originates from California’s 58 counties, state and federal agencies, health plans, and most recently from Covered California. The MEDS currently supports records for about eight million beneficiaries. The ACA is expected to add up to two million additional beneficiaries in 2014, whose data would be stored in MEDS. The state currently receives 75 percent federal funding for MEDS maintenance and operation (M&O). The MEDS is over 30–years old and relies on old technology that is difficult and time–consuming to modify.
Medicaid Information Technology Architecture (MITA). The MITA is an initiative of the federal CMS intended to foster a national framework to support improved systems development and health care management for the Medicaid program (Medi–Cal is California’s Medicaid program). The standards established by MITA set a blueprint consisting of models, guidelines, and principles for states as they implement technology systems to support the administration of Medicaid. In 2011, CMS issued a new rule that limits enhanced federal funding—at the 75 percent level—for M&O to eligibility determination systems that meet MITA standards by December 31, 2015. Noncompliant systems would be supported at the standard federal funding rate of 50 percent for M&O. The CMS also indicated federal funding would be enhanced to 90 percent for the design, development, and implementation (DD&I) of modernized Medicaid eligibility determination systems achieving MITA standards. The enhanced DD&I federal funding is scheduled to expire on December 31, 2015. The CMS has subsequently indicated it will consider extending the enhanced federal funding for DD&I if a state submits a plan to achieve MITA compliance that CMS approves but where the system development is not complete by December 31, 2015.
The Governor’s budget for DHCS includes two proposals regarding MEDS.
MEDS Interface With CalHEERS. The Governor’s budget proposes a two–year extension of 12 limited–term positions and $1.8 million ($314,000 General Fund) for the continuing DD&I and M&O of the interface between MEDS and CalHEERS for the implementation of ACA. The MEDS interface with CalHEERS is not an independent IT project—rather, it is a task necessitated by the ACA and identified within the CalHEERS project plan. The proposal requests three positions in the Medi–Cal Eligibility Division (MCED) that will identify needed simplification and streamlining of Medi–Cal eligibility and enrollment processes as required by ACA. The remaining nine positions would be designated within the Information Technology Services Division (ITSD) and be responsible for designing and implementing the changes to MEDS identified by MCED staff.
MEDS Modernization. The Governor’s budget proposes 16 two–year limited–term positions and $3.5 million ($528,000 General Fund) to support the planning and identification of system requirements for an IT project intended to modernize MEDS. The DHCS indicates that some of MEDS functionality is duplicated in existing or planned systems, such as the Los Angeles Eligibility, Automated Determination, Evaluation and Reporting Replacement System. The DHCS plans to develop the modernized MEDS project in a way that reduces duplication of functionality in existing or planned systems. The project to modernize MEDS is expected to begin in July 2014 and continue through June 2020.
Interface Between MEDS and CalHEERS Necessary. The ACA requires a seamless experience for individuals seeking health insurance coverage through Health Benefit Exchanges. For California, that means Covered California’s CalHEERS must interface—share data—with MEDS, the statewide database that consolidates case information for recipients of Medi–Cal and other programs. Given the complexity of the ACA rules, DHCS expects to review the need for eligibility and enrollment process changes with program and legal staff over the next several years. Technical modifications to MEDS would be made subsequently. The implementation of the ACA also requires changes to the county–based welfare automation systems—the three systems that collectively form the Statewide Automated Welfare System (SAWS) consortia. Each of the consortia systems has its own eligibility determination and benefit calculation functionality built into its system. The MCED resources would provide direction to the consortia systems on necessary changes specific to each system, while the ITSD resources would ensure SAWS changes were compatible with MEDS. Failure to make the technical changes to the MEDS and build the interface with CalHEERS would prevent the state from implementing the programmatic changes to Medi–Cal required by the ACA.
Modernization of MEDS Worthwhile. The modernization of MEDS is a worthwhile objective given the antiquated nature of the technology system and the increasing difficulty in maintaining the system caused in part because of the decline in staff skilled in the outdated technology. The aged technology is time–consuming and costly to maintain and update. The MEDS has other deficiencies that warrant the modernization of the system. Information is difficult to query, especially in real time; reporting capabilities are not met; and there are concerns about the security of data maintained in MEDS. A modernized system could provide a more efficient querying of data and address privacy and security concerns.
Failure to Modernize MEDS Could Also Jeopardize Continued Enhanced Federal Funding. The current MEDS does not meet CMS’ MITA standards. Failure to comply with CMS’ MITA standards jeopardizes the state’s ability to secure enhanced federal funding for maintenance and operation of MEDS. (Federal funding for MEDS would revert to a standard 50 percent federal contribution from the enhanced 75 percent contribution.) Delaying the modernization project would also compromise the state’s ability to leverage enhanced federal funding for the DD&I of a modernized MEDS, which is scheduled to expire on December 31, 2015. Modernizing MEDS to achieve MITA compliance would enhance the functionality of the system and position the state to maximize federal funds for the DD&I and M&O of a modernized MEDS.
Budget Proposal’s Focus on MEDS Modernization Planning Seems Reasonable. The MEDS modernization component of the budget proposal takes a new approach to IT development by focusing on the planning phase of the project. Typically, departments absorb the cost of planning a project and instead submit the completed plan to the Legislature for the review and approval of funds to support the DD&I phase of a project. Departments that absorb the cost of the planning phase may not be able to allocate the resources necessary to develop a robust plan. There are potential longer–term consequences of not allocating sufficient resources at the front–end of a project, including costly replanning and rework during the DD&I phase when additional resources have been allocated towards the project and the state’s technology needs are better understood. The Legislature, by approving this proposal, would not be approving the MEDS modernization project in totality. Rather, the Legislature would still have the opportunity to review and approve the project when a project plan was submitted. Given the criticality of this project, this new planning–focused approach has merit.
We recommend approval of the Governor’s proposal for a two–year extension of 12 limited–term positions and $1.8 million for the ongoing DD&I and maintenance of the interface between MEDS and CalHEERS for the implementation of the ACA. The proposal positions the state to comply with ACA–related streamlining and simplification of Medi–Cal eligibility and enrollment processes.
We also recommend approval of the Governor’s proposal for 16 two–year limited–term positions and $3.5 million to support the planning and identification of system requirements for the modernization of the MEDS project. Approval of the planning phase of the MEDS modernization proposal would position the state to leverage continued enhanced federal funding while working towards MITA compliance. Given the criticality of the MEDS modernization project, we also recommend the Legislature direct DHCS to report to the Legislature at 2015–16 budget hearings on the status of the planning and identification of system requirements effort. Specifically, DHCS should report on information gleaned through the planning phase and share details regarding the modernization project’s scope, timeline, and cost.
The ACA, also known as federal health care reform, establishes entities, called Health Benefit Exchanges, where individuals can purchase health coverage. The California Health Benefit Exchange—also known as the Exchange or Covered California—provides access to nonemployer–based health coverage, small–employer–based coverage, federal subsidies for health coverage, and Medi–Cal eligibility referral to counties. The first open enrollment period for purchasing individual market health coverage through the Exchange began October 1, 2013 and runs through March 31, 2014. The Exchange’s performance during this initial open enrollment period will provide insight into the Exchange’s fiscal outlook going forward.
Summary of Analysis. In this analysis, we begin by providing an overview of ACA and the operation of the Exchange in California. We then summarize the Exchange’s fiscal forecast and discuss its fiscal outlook based on the results from the open enrollment period to date. Finally, we recommend that representatives of the Exchange report at budget hearings on its fiscal outlook after the conclusion of the initial open enrollment period.
The ACA is far–reaching legislation that makes significant changes to health coverage and delivery in California. The ACA is, in part, designed to create a health coverage purchasing continuum that makes it easier for persons to access, purchase, and maintain health coverage. As individuals’ incomes rise and fall; as they become employed, change employers, or become unemployed; and as they age, they are to have access to different sources of coverage along the coverage continuum. Creating this continuum requires the modification of existing government programs and integration of these programs with new coverage options created by ACA.
Imposes Individual Mandate. The ACA imposes an individual mandate requiring most U.S. citizens and legal residents to have health coverage or pay a penalty. There are exceptions to the mandate for financial hardship, religious objections, and certain other specified reasons. In 2014, persons signing up for health coverage by the March 31st enrollment deadline will not be penalized for being without health insurance prior to the coverage start date.
Establishes Exchanges Where Individuals Can Purchase Health Coverage. Chapter 655, Statues of 2010 (AB 1602, J. Pérez), and Chapter 659, Statutes of 2010 (SB 900, Alquist and Steinberg), established the California Health Benefit Exchange along with a governing board. Through the Exchange, individuals and employees of small businesses (50 employees or less) that choose to offer coverage through the Exchange are able to enroll in subsidized and unsubsidized health coverage. Coverage offered through the Exchange must include a minimum set of benefits, known as the “essential health benefits.”
Provides Federal Subsidies for Certain Individuals Purchasing Exchange Coverage. Citizens and legal residents with incomes between 100 percent and 400 percent of the FPL who are not offered affordable coverage by their employer and who do not qualify for other public health insurance programs, such as Medi–Cal or Medicare, are eligible for federal subsidies to help them to purchase coverage through the Exchange. In addition, certain newly qualified resident aliens may also be eligible for federal subsidies. The amount of federal subsidies vary based on income, with greater federal subsidies available to households with lower incomes.
Establishes Small Business Health Options Program (SHOP). The ACA established SHOP to allow employers with up to 50 full–time–equivalent (FTE) employees to purchase health coverage for their employees. This service will expand to employers with up to 100 FTE employees beginning January 1, 2016. In California, the Exchange is also operating SHOP, which is projected to account for only about 10 percent of total enrollment through the Exchange.
Requires That Only Qualified Health Plans (QHPs) Be Sold Through Exchanges. The Exchange certifies the QHPs offered through the Exchange. Certification is based upon the plan’s ability to meet federal requirements regarding: (1) benefit design; (2) marketing practices; (3) provider networks, including community providers; (4) plan activities related to quality improvement; and (5) the use of standardized formats for consumer information.
Authorizes Medicaid Expansion up to 138 Percent of the FPL. California chose to participate in ACA’s optional Medicaid expansion. Effective January 1, 2014, California expanded Medi–Cal eligibility to include previously ineligible adults with incomes up to 138 percent of the FPL—largely childless adults. For more information on the Medicaid expansion and its impacts in California, please see our analysis of ACA Implementation in the “Medi–Cal” section of this report.
As discussed above, California decided to operate its own Health Benefit Exchange rather than participate in the federally facilitated health exchange. This gives the state increased flexibility and control over the implementation and ongoing operations of the Exchange, which is a nexus for nonemployer–based health coverage, small–employer–based coverage, access to federal subsidies, and Medi–Cal eligibility referral.
Exchange Is the Only Place to Purchase Subsidized Health Coverage Under ACA. While health coverage in the individual market is available for purchase both inside and outside the Exchange, federal subsidies are only available through the Exchange. It is estimated that 2.6 million people are eligible for subsidized health coverage in California.
Exchange Is a Gateway for Medi–Cal Enrollment. The Exchange provides initial screening for Medi–Cal eligibility and refers individuals likely–eligible for Medi–Cal to county eligibility workers for final eligibility determination. Applicants are also able to indicate interest in learning more about social services programs, including CalFresh and CalWORKs.
Medi–Cal Bridge Plans Are Only Available Through Exchange. Pending federal approval, the Exchange will offer health coverage through Medi–Cal Managed Care plans that have been certified as QHPs. These Medi–Cal Managed Care QHPs will be available to: (1) individuals with incomes below 250 percent of the FPL who are transitioning from Medi–Cal coverage to subsidized coverage offered through the Exchange due to an increase in income and (2) parents or caretaker relatives of Medi–Cal enrolled children who themselves do not qualify for Medi–Cal. Family members who are living in the same household as individuals enrolled in Medi–Cal Managed Care Plans may also be eligible. These plans will provide continuity of care to individuals who experience a disruption in Medi–Cal eligibility and will provide families with Medi–Cal–eligible children and subsidy–eligible parents the option to be covered by the same insurer.
Exchange Enrollment Can Reduce County–Funded Care for the Medically Indigent. Using funds received from 1991 realignment, counties have fiscal and programmatic responsibility for providing health care for low–income populations without public or private insurance—also known as indigent health care. However, under ACA, counties will realize savings because ACA shifts much of the responsibility for indigent health care to the state and federal governments as individuals enroll in Medi–Cal or federally subsidized health coverage. While the majority of savings to counties will be realized through the optional Medi–Cal expansion, there may also be savings to counties from individuals enrolling in health coverage through the Exchange. For example, some adults with incomes above 138 percent of the FPL who previously may have been eligible for indigent health care services in some counties will now be eligible for federally subsidized health coverage through the Exchange. To the extent these adults enroll in subsidized coverage offered through the Exchange, it will relieve the counties from paying for their medical care.
Counties Must Utilize Savings to Support CalWORKs, Thereby Offsetting General Fund Expenditures. In recognition of the shifting responsibility for indigent health care, the 2013–14 budget established a complex structure under which a portion of county health realignment funds will be redirected to pay CalWORKs grant costs borne by the state—thereby offsetting General Fund costs.
During the initial start–up and implementation phase, the Exchange is funded through federal grants, but due to federal requirements, the Exchange cannot be supported by federal funds after December 31, 2014. The Exchange is also prohibited in state statute from receiving General Fund support. To support its operations beyond 2014, the Exchange will charge insurance carriers a per–member, per–month (PMPM) fee based on enrollment into the carriers’ QHPs offered through the Exchange. While the Exchange is authorized by Chapter 655 to charge the level of fee necessary to support its operations, it can only set the fee amount once annually when it enters into contracts with the insurers, usually in August. The Exchange is, therefore, subject to financial risk because it must determine the amount of assessment fee to charge based on its projected enrollment for health coverage through the Exchange and operating costs for the year. To the extent that enrollment does not meet the projection, the Exchange will generate less revenue than anticipated. This is particularly important during the early years of the Exchange’s operation when there is the most uncertainty surrounding the number of individuals who will enroll in health coverage through the Exchange.
Background. The Exchange’s FSP is a comprehensive financial plan developed to determine whether the Exchange’s revenue streams would support its operations in the long term given the requirement for financial self–sufficiency. The FSP is based on a multiyear analysis of the Exchange’s activities, estimated operating costs, projected enrollment, and estimated revenues. The Exchange Board adopted the FSP in November 2012. The FSP’s projections were updated in the Board’s 2013–14 Exchange budget, which was approved in June 2013 prior to the Exchange’s first open enrollment period. The projections include estimates for Exchange enrollment, revenues, and operating costs for each of three enrollment–level scenarios. The Exchange relies on enrollment estimates for the scenarios from the California Simulation of Insurance Market (CalSIM) model, which was developed jointly by the University of California, Los Angeles Health Policy Research Center, and the University of California Berkeley Labor Center. The three enrollment level–scenarios are defined as follows:
- The Enhanced Enrollment Projection (EEP). The EEP is the highest of the potential enrollment levels calculated by CalSIM and assumes English language proficiency is not a barrier to enrollment, that eligibility and enrollment processes and systems are simplified, and that the Exchange implements a robust outreach and education effort to make all potentially eligible individuals aware of their coverage opportunities.
- The Base Enrollment Projection (BEP). The BEP is lower than EEP and relies on different assumptions than EEP. For example, this projection assumes that English proficiency could present a barrier to enrollment.
- The Low Enrollment Projection (LEP). The LEP sets enrollment at 20 percent below BEP.
Our Analysis Focuses on Exchange Enrollment in the Individual Market. In this analysis, we focus on the fiscal outlook for the individual market segment of the Exchange because enrollment, operating costs, and revenues for SHOP are small—less than 7 percent of the Exchange’s total operating budget for 2013–14—relative to the individual market. The Exchange individual market open enrollment period occurs annually beginning in the fall (the first open enrollment period began in October 2013 to allow individuals to enroll in coverage beginning January 1). Only individuals undergoing a specified change in circumstance (for example, a change in income) may enroll outside of the open enrollment period. Figure 9 shows CalSIM estimates for three potential levels of enrollment over four state fiscal years.
Figure 9
Individual Market Enrollment Projectionsa
As of Fiscal Year End
|
Enrollment Projection Level
|
2013–14
|
2014–15
|
2015–16
|
2016–17
|
|
Enhanced
|
894,000
|
1,478,000
|
1,942,000
|
2,308,000
|
|
Base
|
629,000
|
999,000
|
1,281,000
|
1,578,000
|
|
Low
|
274,000
|
587,000
|
940,000
|
1,258,000
|
|
aAs estimated in June 2013.
|
PMPM Fee Assessed on QHPs Linked to Enrollment. The Exchange projects that the fee assessed on QHPs in future years will be higher under BEP and LEP relative to the fee charged under EEP. The higher fee levels that would be assessed under BEP and LEP are necessary to generate enough revenue to pay for Exchange operations and ensure a sufficient reserve. (The fee is likely to be passed on to consumers in the form of higher premiums.) The projected fees under each enrollment scenario are summarized in Figure 10.
Figure 10
Exchange Individual Market PMPM Assessment Fee Projections
|
Enrollment Projection Level
|
2014
|
2015
|
2016
|
2017
|
|
Enhanced
|
$13.95
|
$10.46
|
$9.94
|
$9.44
|
|
Base
|
13.95
|
12.83
|
12.83
|
12.83
|
|
Low
|
13.95
|
16.04
|
20.86
|
12.51
|
Exchange Budget Projections Under Three Scenarios. The Exchange forecasted its operating budget from 2013–14 through 2016–17 under the three enrollment–level scenarios. Each of these scenarios include estimates of total annual revenues and total annual operating costs (explained in more detail below). We summarize the Exchange’s individual market operating budget projections for 2013–14 through 2016–17 under each of the three enrollment scenarios in Figure 11.
Figure 11
Exchange Individual Market Operating Budget Projectionsa
(In Millions)
|
Enrollment Projection Level
|
2013–14
|
2014–15
|
2015–16
|
2016–17
|
|
Enhanced
|
|
|
|
|
|
Total revenues
|
$411
|
$400
|
$212
|
$248
|
|
Federal grants
|
(351)
|
(227)
|
—
|
—
|
|
PMPM assessment revenue
|
(60)
|
(172)
|
(212)
|
(248)
|
|
Less operating costs
|
358
|
288
|
280
|
279
|
|
Net Income
|
$52
|
$112
|
–$69
|
–$31
|
|
Fiscal year–end reserve balance
|
52
|
164
|
95
|
65
|
|
Base
|
|
|
|
|
|
Total revenues
|
$394
|
$365
|
$178
|
$223
|
|
Federal grants
|
(351)
|
(233)
|
—
|
—
|
|
PMPM assessment revenue
|
(43)
|
(132)
|
(178)
|
(223)
|
|
Less operating costs
|
358
|
255
|
247
|
245
|
|
Net Income
|
$36
|
$111
|
–$69
|
–$22
|
|
Fiscal year–end reserve balance
|
36
|
146
|
78
|
56
|
|
Low
|
|
|
|
|
|
Total revenues
|
$370
|
$311
|
$175
|
$219
|
|
Federal grants
|
(351)
|
(234)
|
—
|
—
|
|
PMPM assessment revenue
|
(19)
|
(78)
|
(175)
|
(219)
|
|
Less operating costs
|
358
|
226
|
218
|
216
|
|
Net Income
|
$11
|
$85
|
–$43
|
$3
|
|
Fiscal year–end reserve balance
|
11
|
96
|
53
|
56
|
Exchange Revenues. The Exchange has received over $1 billion in federal grants to support its operations through December 31, 2014. This includes a $155 million grant that was awarded in January 2014 (as this grant was recently awarded, it is not included in the Exchange’s fiscal projections presented in this report). In 2014, the Exchange is assessing a PMPM fee of $13.95, or 4.4 percent of the average monthly premium of $320, for products offered on the Exchange.
Revenue Driven by Individual Market Enrollment. As the Exchange’s revenue generation relies on PMPM fees assessed on QHPs, it is highly dependent on enrollment. During the first few years of the Exchange’s operations, its revenue is projected to increase steadily as enrollment ramps up to a level where revenues will be sufficient to cover all of the Exchanges operating costs. However, initially revenues will be insufficient to cover operating costs. The Exchange accounts for this in its projections by building up a reserve using PMPM fee revenues collected during 2014 while operations are supported by federal grants. During 2015–16 and 2016–17, the Exchange anticipates drawing on this reserve to cover part of its operating expenses.
Exchange Operating Costs. The Exchange will have the following broad categories of operating costs:
- Exchange Staffing, Service Center Staffing, and Ongoing Operations. As of November 2013, the Exchange reported a staffing level of 725 FTE positions, with plans to increase the number of service center staff to meet demand during open enrollment.
- IT Infrastructure. The Exchange has contracted with an independent vendor to design, develop, and implement CalHEERS to determine eligibility and manage the population enrolled by the Exchange.
- Marketing Outreach and Education. The Exchange has implemented a broad array of marketing, outreach, and education activities and believes that it will require considerable resources going forward to effectively reach a culturally and linguistically diverse target population spread over a large geographic area.
PMPM Fees Would Be Increased and Operating Costs Would Be Decreased Under BEP and LEP. In addition to raising the PMPM fee assessed on QHPs, the Exchange will also consider other mechanisms to bring revenues in line with expenses if enrollment falls below EEP, including reducing its operating costs. The BEP and LEP scenarios reflect reductions in operating expenses to bring them in line with revenues and to maintain a sufficient reserve.
The Exchange’s Goal Is to Maintain a Reserve of at Least Three Months of Operating Expenses. In the statutes which established the Exchange, the board of the Exchange is directed to maintain a prudent operating reserve. The Exchange has determined that it will maintain a reserve equivalent to three to six months of operating expenses. Under all three of the scenarios described in this analysis, the Exchange maintains a reserve roughly equal to or greater than three months of operating costs in all years.
On October 1, 2013, the Exchange began enrollment into health coverage for 2014. Given that enrollment is ongoing until March 31, 2014 and this is the first year of Exchange enrollment, there is significant uncertainty surrounding the final enrollment of individuals into health coverage for 2014.
Number of Enrollees Paying Premiums to Date Unknown. According to the Exchange, over 625,000 individuals had selected a health plan through the Exchange as of January 14, 2014. At the time of this analysis, the number of individuals who made their first premium payment was not available. The distinction between individuals who select a plan through the Exchange and then make a premium payment versus those individuals who select a plan and never make a premium payment (such that they are not actually enrolled in a plan) is important because the Exchange only receives PMPM fee revenues when individuals pay premiums.
Enrollment Rate Likely to Increase Prior to Mandate Penalty Deadline. The Exchange may experience an uptick in enrollment prior to the March 31 deadline for one to either obtain health coverage or face the individual mandate penalty. Massachusetts implemented state–level health care reform in 2007 including an individual mandate penalty for not having health coverage and subsidies for individuals below 300 percent of the FPL. An analysis of enrollment trends in Massachusetts found an uptick in enrollment leading up to the mandate penalty deadline. In California, a similar increase may occur prior to the mandate penalty deadline in March.
Exchange Will Have to Reevaluate Fiscal Projections Based on Enrollment. After the end of open enrollment, the Exchange will have to reevaluate and adjust its fiscal projections in order to prepare its 2014–15 budget for approval by the board. If the EEP is not reached, the Exchange is likely to need to adjust its operating budget as shown under EEP. If the Exchange determines it needs to charge higher–than–projected PMPM fees, the fees may still be less than the current fee of $13.95, although, potentially not as low as the $10.46 fee for 2015 projected under EEP shown in Figure 10.
Future Enrollment Considerations. We note that Latinos represent only 18 percent of total enrollment through mid–January despite representing 57 percent of the uninsured population as of 2012. In order to reach enrollment targets going forward, the Exchange will likely need to achieve higher levels of enrollment among Latinos, as well as among other populations with high rates of the uninsured, such as young adults.
The Legislature should ask representatives of the Exchange to report on its fiscal outlook at budget hearings as soon as practicable after the March 31 open enrollment deadline. This will allow the Exchange sufficient time to evaluate its enrollment and financial projections after the open enrollment period ends, thereby providing a better sense of the Exchange’s fiscal outlook as the Legislature nears the May Revision. We recommend that the Exchange report on the following:
- Final Enrollment Numbers. The Exchange should provide updated Exchange enrollment numbers for the first open enrollment period including the number of individuals who (1) selected a health plan through the Exchange and (2) made their first premium payment. The Exchange should also report on any issues encountered by consumers in paying their premiums.
- Continued Marketing and Outreach Efforts. The Exchange should report on which marketing and outreach efforts were successful, where it has identified issues, and how it plans to modify its marketing and outreach efforts to improve enrollment among hard to reach populations, including Latinos and young adults.
- Integration Efforts With Counties. The Exchange should also provide an update on the status of federal approval for Medi–Cal bridge plans. The Exchange should report on any barriers or issues it has faced in working with counties to determine Medi–Cal eligibility and enroll eligible individuals.
Updated Fiscal Projections for Next Four Years at May Revision. We recommend the Exchange report at budget hearings during the May Revision on its updated fiscal forecast for 2014–15 through 2017–18. The updated fiscal forecast should include projections of enrollment, PMPM fee amounts, operating costs, and revenues.
Overview of DPH. The DPH administers and oversees a wide variety of programs with the goal of optimizing the health and well–being of Californians. The DPH is organized into several offices and centers, including the Center for Chronic Disease and Health Promotion, the Center for Infectious Diseases, the Center for Family Health, the Center for Environmental Health, and the Center for Health Care Quality. The department’s programs address a broad range of health issues, including maternal and child health, chronic diseases, communicable disease control, injuries, environmental health, food and drug safety, emergency preparedness, and oversight of health facilities. Many public health programs and services are delivered at the local level, while the state provides funding, oversight, and overall strategic leadership for improving public health. The state also directly administers certain public health programs, such as licensing and certification of health facilities.
Overall Budget Proposal. The budget proposes $3 billion (all funds) for support of DPH programs in 2014–15—$683 million for state operations and $2.3 billion for local assistance—which is a net decrease of $472 million, or 14 percent, below revised 2013–14 expenditures. General Fund expenditures for 2014–15 are proposed at $111 million, a net decrease of $4 million, or 3.5 percent, below the revised estimate of 2013–14 expenditures. The net decrease in General Fund and total expenditures is mainly attributable to the Governor’s proposal to transfer DWP from DPH to SWRCB. (For our analysis of this proposal, please see The 2014–15 Budget: Resources and Environmental Protection report, which is forthcoming.)
The Governor’s budget for DPH reflects technical budget adjustments due to changes in caseload and costs for some programs, such as ADAP and the Women, Infants, and Children program. It also reflects the proposed transfer of DWP from DPH to SWRCB (which we recommend in our aforementioned analysis) and seven other budget change proposals. Overall, we find the Governor’s budget proposal generally to be reasonable. However, later in this analysis, we discuss issues identified with ADAP and Licensing and Certification (L&C) Program estimates. We have analyzed the following seven budget proposals and have not identified any issues. However, if we receive additional information that causes us to reassess our findings, we will apprise the Legislature. The seven proposals are as follows:
- Increase Resources for L&C Program Evaluation. Increase expenditure authority by $1.4 million (special funds) to expand work related to the L&C Program evaluation. The first phase of the program evaluation is ongoing and will provide a high–level program assessment to identify issues and barriers to a timely fulfillment of state and federal certification workload. As a next step, DPH will hire a contractor to provide quality improvement recommendations and an implementation plan to address the issues identified in the first phase of the evaluation.
- Increase Resources for L&C Program Review of State Licensing Standards. Increase expenditure authority by $201,000 (special funds) in 2014–15 to contract with the University of California, Davis to conduct an independent research analysis that assesses the extent to which federal certification standards for chronic dialysis, rehabilitation, and surgical clinics are sufficient as a basis for state licensing standards, as required by Chapter 722, Statutes of 2013 (SB 534, Hernandez).
- Increase Resources for the Center for Health Care Quality’s Medical Breach Privacy Enforcement. Increase expenditure authority by $251,000 (special funds) and shift three positions from the California Office of Health Information Integrity to DPH to combine two existing programs charged with enforcing medical privacy violations. This proposal requires statutory changes to allow DPH to take enforcement actions against individuals who commit medical privacy breach violations.
- Convert Two Division of Communicable Disease Control Contract Positions. Convert two contract positions within the Division of Communicable Disease Control to full–time, permanent state positions to eliminate reliance on contracting for essential program services. Assumes savings of $46,000 (special funds).
- Increase Resources for the Infant Botulism Treatment and Prevention Program (IBTPP). Increase expenditure authority for IBTPP by $3 million in 2014–15 and $951,000 in 2015–16 (special funds) in order to sustain production, distribution, regulatory compliance, and other activities for BabyBIG (a drug used to treat infant botulism).
- Convert 45 Nutrition Education and Obesity Prevention Branch (NEOPB) Contract Positions. Convert 45 contract positions within NEOPB to full–time, permanent positions to eliminate reliance on contracting for essential program services. Assumes savings of $9.3 million in 2014–15 and $12.7 million (federal funds) in subsequent years which will be reinvested into direct services provided by local lead agencies to increase nutrition education.
- Increase Resources for the Office of Health Equity’s (OHE) Health in All Policies (HiAP) Task Force. Increase DPH’s budget by $458,000 (federal and special funds) and add four positions to staff HiAP Task Force within OHE.
Below, we provide a summary of the issues identified in ADAP and L&C estimates and give our recommendations.
DHCS Medi–Cal Estimate Does Not Reflect ADAP Estimate Adjustment
Background on ADAP. The ADAP is administered by the Office of AIDS (OA) within DPH. The ADAP helps to ensure that people living with Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) have access to HIV medication. The federal government has mandated that certain federal funds which support ADAP must be the payer of last resort; therefore, all ADAP applicants must be screened to determine if they have private insurance or are eligible for other government programs that provide HIV medications before they can be enrolled in ADAP. Eligibility for ADAP is currently recertified every six months. Over 36,000 people will receive ADAP services during 2013–14.
The ADAP receives funding from the following sources:
- Federal Health Resources and Services Administration (HRSA) Ryan White Grant. In 2013–14, ADAP estimates using $104 million in HRSA funds. The OA receives federal funding from an annual HRSA Ryan White HIV/AIDS Program grant, part of which is earmarked for ADAP–related services.
- Drug Rebates. The ADAP also receives funding through mandatory and voluntary supplemental rebates from drug manufacturers for drugs dispensed to ADAP clients. In 2013–14, ADAP estimates using $308 million in rebate funding.
- General Fund. The ADAP receives $411,000 in General Fund support in 2013–14 for state operations only.
- Federal Safety Net Care Pool (SNCP) Funds. In 2013–14, ADAP estimates using $8.3 million in SNCP funds. (The Medi–Cal estimate reflects ADAP using $66.4 million in SNCP funds; we discuss this discrepancy below.) The SNCP is established under California’s “Bridge to Reform” Medicaid 1115 Demonstration waiver. Two billion dollars ($400 million annually over five years) of SNCP funds are to be utilized for Designated State Health Programs, including ADAP, California Children’s Services, Genetically Handicapped Persons Program, and other specified programs.
2014–15 Budget Proposal. The budget proposes $412 million (all funds) for the support of ADAP in 2014–15, which is a net decrease of $9 million, or 2 percent, below revised 2013–14 expenditures of $421 million. General Fund expenditures are proposed at $411,000—the same level as revised 2013–14 expenditures.
ADAP Is Returning $58 Million in SNCP Funds to DHCS in 2013–14. In 2013–14, $66.3 million in SNCP funds were allocated to ADAP in DHCS’s Medi–Cal estimate. The ADAP estimates using only $8.3 million of the available SNCP funds because there is a new federal requirement to spend all available rebate funds before spending federal funds. Pursuant to this requirement, ADAP is spending all rebate funds received in 2013–14 and all rebate funds built up in its reserve. Accordingly, the November 2013 ADAP estimate shows that ADAP is returning the remaining $58 million in SNCP funds to DHCS. Due to timing issues, DHCS was unable to incorporate the $58 million in returned SNCP funds into the Medi–Cal estimate. The department has indicated that it will make appropriate adjustments at the time of the May Revision.
Analyst’s Recommendation. We recommend the Legislature recognize in its budget deliberations that $58 million in federal SNCP funds are unallocated in 2013–14. We further recommend DHCS to report in budget hearings on options for allocating these funds so that the Legislature can ensure that their allocation best reflects legislative priorities. We have reviewed the ADAP estimate and do not have any issues to raise. We will review the ADAP estimate at the time of the May Revision and advise the Legislature whether we recommend any adjustments.
Background. The L&C program, within DPH’s Center for Health Care Quality, is responsible for ensuring that health care facilities comply with state and federal laws and regulations. The CMS contracts with L&C to ensure that facilities accepting Medicare and Medi–Cal payments meet federal requirements. The L&C program also oversees the licensing of nursing home administrators and the certification of nurse assistants, home health aides, and hemodialysis technicians.
L&C Estimate Includes a $9.2 Million Adjustment to Avoid a Decrease in Funding From the Current Level. The November 2013 L&C estimate projects a $9.2 million decrease in its funding requirement in 2013–14 and 2014–15 resulting from a decrease in overall surveyor workload hours and staffing requirements. Staffing requirements for 2013–14 were overestimated in prior estimates partially due to a technical calculation error. Despite the decrease in staffing requirements, the estimate includes a $9.2 million adjustment in order to maintain funding at current levels in 2013–14 and 2014–15. The majority of this $9.2 million adjustment is made up of funds from fees imposed on facilities regulated by L&C (there is no adjustment to General Fund support). The DPH would like to maintain current funding levels for 2013–14 and 2014–15, because L&C is undergoing a comprehensive program evaluation which aims to help L&C understand its staffing requirements and improve the reliability of its estimate (part of this program evaluation is subject to approval of a budget proposal for 2014–15). This program evaluation is projected to be completed by the fall of 2016.
Analyst’s Recommendation. We find that there is insufficient workload justification to maintain the current level of funding for L&C in 2013–14 and 2014–15. We recommend that the Legislature reject L&C’s proposed $9.2 million adjustment to maintain funding at the current level. The administration should request the level of funding it believes necessary to fund the current projected workload for L&C. Once the results of the L&C program evaluation are available, funding should be adjusted to reflect any new information regarding staffing levels and workload.
The Governor proposes to eliminate MRMIB effective July 1, 2014, and shift the three programs currently administered by MRMIB to DHCS. In this analysis, we provide an overview of MRMIB and a summary of the Governor’s proposal for MRMIB’s elimination. We outline general principles of when a government reorganization, such as the elimination of a board, agency, office, or department makes sense, and provide our assessment of the Governor’s proposal.
The MRMIB consists of five members (hereafter referred to as the board), all of whom serve four–year terms: the Governor appoints the chair and two other members and the Senate Committee on Rules and the Speaker of the Assembly each appoint one member. The board selects an executive director who manages MRMIB’s staff and directs the day–to–day administration of the programs overseen by the board.
The board holds monthly public meetings where its five members are presented with information about the programs MRMIB administers, such as program enrollment reports, state budget updates, and vendor performance reports. Much of the information presented by MRMIB’s executive director and staff at these monthly meetings is made available to the public on MRMIB’s website. The MRMIB currently administers three programs—Major Risk Medical Insurance Program (MRMIP), Access for Infants and Mothers (AIM), and the County Health Initiative Matching Fund Program (CHIM)—that provide health coverage. We describe these three programs below in more detail as well as HFP formerly administered by MRMIB.
MRMIP. The MRMIP is a health insurance high–risk pool, established in January 1991, that provides health insurance for Californians unable to obtain coverage in the individual health insurance market because of their preexisting conditions. Californians qualifying for the program participate in the cost of their health insurance coverage by paying premiums. The state supplements the premiums paid by enrollees to cover the cost of care in MRMIP. Because of funding limitations, MRMIP sometimes has a waiting list. Caseload for MRMIP was 6,321 as of November 2013.
AIM. The AIM Program provides low–cost, health insurance coverage to uninsured middle–income pregnant women and to women who have private insurance with a maternity–only deductible or copayment greater than $500. Pregnant women whose family income is between 200 percent and 300 percent of the FPL are eligible for the program provided they meet certain eligibility requirements such as being not more than 30 weeks pregnant as of the application date and being ineligible for no–cost Medi–Cal. (Pregnant women with incomes below 200 percent of the FPL are generally eligible for the Medi–Cal Program.) The AIM Program provides coverage through participating health plans and covers eligible women through their pregnancy and 60 days postpartum. Caseload for AIM was 5,474 as of December 2013.
CHIM. Chapter 648, Statutes of 2001 (AB 495, Diaz), created the CHIM in the State Treasury. The fund allows for the intergovernmental transfer of local funds used for local County Children’s Health Initiative (CHI) purposes to draw down federal matching funds for children eligible for federal Children’s Health Insurance Program (CHIP) funding. The CHI provides low–cost health coverage to uninsured children through age 19 who are not eligible for TLICP—formerly HFP—or no–cost Medi–Cal, and whose household income falls within 251 percent to 300 percent of the FPL. The fund allows counties and county agencies to use local county funds as a match to draw down federal CHIP funds for CHIs. The counties use the federal matching funds to provide health insurance coverage to uninsured children through County Organized Health Systems of Local Initiatives.
HFP Was Shifted to DHCS. California’s CHIP was formerly administered by MRMIB and known as HFP. Chapter 28, Statutes of 2012 (AB 1494, Committee on Budget), was enacted by the Legislature to implement a modified version of the Governor’s proposal to shift all HFP enrollees into Medi–Cal. Between January 1, 2013 and November 1, 2013, about 850,000 HFP enrollees were shifted to Medi–Cal. The name of California’s CHIP was changed from HFP to TLICP. The 2013–14 Budget Act provides authority for the administration to shift MRMIB’s personnel from MRMIB to DHCS. While the shift of HFP enrollees to TLICP has been completed, the shift of the personnel who administered HFP, from MRMIB to DHCS, is still in progress.
Infants born to women enrolled in AIM (commonly referred to as AIM–linked infants) are automatically eligible for HFP, unless they are enrolled in employer–sponsored insurance or no–cost Medi–Cal. Effective November 1, 2013, AIM–linked infants began transitioning from HFP into the Medi–Cal delivery system. The AIM–linked infants program is being renamed the Medi–Cal Access Program.
Overall Budget Proposal. The budget plan proposes no funding for MRMIB in 2014–15, which is consistent with the administration’s proposal to eliminate MRMIB. Here we provide a summary of the amount of funding—broken out by state operations and local assistance—that would shift from MRMIB to DHCS under the proposal.
State Operations Funding Shifted to DHCS. Excluding the year–over–year effect of the HFP shift which we describe separately below, the budget proposes $2.9 million (all funds) in DHCS state operations funding in 2014–15 for the programs administered by MRMIB in 2013–14. As shown in Figure 12, the budget plan proposes no year–over–year change in state operations funding for these programs between 2013–14 and 2014–15.
Figure 12
Shift of State Operations Funding From MRMIB to DHCS
(Dollars in Millions)
|
Program
|
From MRMIB
(2013–14 Authorized)
|
|
To DHCS
(2014–15 Proposed)
|
|
Change From 2013–14 to 2014–15
|
|
General Fund
|
Total Funds
|
Positions
|
General Fund
|
Total Funds
|
Positions
|
Total Funds
|
Positions
|
|
Access for Infants and Mothers
|
—
|
$1.1
|
6.0
|
|
—
|
$1.1
|
6.0
|
|
—
|
—
|
|
Major Risk Medical Insurance Program
|
—
|
1.3
|
6.0
|
|
—
|
1.3
|
6.0
|
|
—
|
—
|
|
County Health Initiative Matching Fund
|
—
|
0.5
|
3.0
|
|
—
|
0.5
|
3.0
|
|
—
|
—
|
|
Subtotals, MRMIB Programs
|
—
|
($2.9)
|
(15.0)
|
|
—
|
($2.9)
|
(15.0)
|
|
—
|
—
|
|
Healthy Families Program
|
$1.0
|
3.2
|
14.0
|
|
$0.8
|
1.9
|
12.0
|
|
–$1.3
|
–2.0
|
|
Totals
|
$1.0
|
$6.1
|
29.0
|
|
$0.8
|
$4.8
|
27.0
|
|
–$1.3
|
–2.0
|
The 2013–14 Budget Act provides authority for the DOF to transfer positions and funds in order to complete the transfer of HFP from MRMIB to DHCS within 2013–14. However, MRMIB wants to maintain the 12 positions throughout 2013–14 for closeout activities related to the transfer of HFP, and the budget is therefore proposing to transfer the 12 positions and corresponding funding on July 1, 2014.
As shown in Figure 12, the proposal would shift $1.9 million ($800,000 General Fund) in state operations funding and 12 positions to complete the transfer of HFP to DHCS. This is a funding decrease of $1.2 million ($232,000 General Fund) or about 40 percent below the revised estimate of current–year spending.
Local Assistance Funding Shifted to DHCS. Excluding the year–over–year effect of the HFP shift which we describe separately below, the budget proposes DHCS local assistance funding of $173 million (all funds) in 2014–15 for programs administered by MRMIB in 2013–14. This is an increase of almost $11 million ($212,000 General Fund) over revised 2013–14 spending levels. Almost all of the proposed year–over–year increase is due to growth in spending in AIM.
The MRMIB’s 2013–14 budget includes $63 million all funds ($22 million General Fund) to fund the provision of services to HFP enrollees between July 1, 2013 and November 1, 2013 when the last HFP enrollees were shifted to the TLICP.
The Governor’s budget plan proposes to eliminate MRMIB and shift MRMIB’s remaining programs and administrative functions to DHCS. Under the administration’s proposal, 27 positions (including 12 positions for administration of HFP) and $4.8 million in state operations funding (including $1.9 million for administration of HFP) would be shifted from MRMIB to DHCS in 2014–15.
The administration’s rationale for the proposal is that it is inefficient to maintain infrastructure for MRMIB to administer three small programs serving approximately 14,000 subscribers. In the past, administration of HFP was the majority of the work undertaken by MRMIB and with the completion of the transition of the HFP population, MRMIB has been relieved of the bulk of its workload. Furthermore, the administration states that transitioning the remaining MRMIB programs to DHCS makes operational sense and further streamlines California’s publicly financed health programs.
Here we describe general principles of when a government reorganization, such as the proposed elimination of MRMIB, makes sense. Broadly, a reorganization should maintain or improve the efficiency, effectiveness, and accountability of an organization; be based on a policy rationale; and reflect legislative priorities. Later in this analysis we evaluate the Governor’s proposal based on these criteria.
Reorganization Should Maintain or Improve Efficiency. A reorganization should maintain or improve efficiency by eliminating overlapping or duplicative government functions and/or maximizing existing resources through better departmental coordination and allocation of administrative functions. From a fiscal perspective, improved efficiency may result in savings from eliminating duplicative government functions and achieving economies of scale.
Reorganization Should Maintain or Improve Effectiveness. A reorganization should contribute toward the fulfillment of the mission of the department or entity that will assume responsibility for administration of a program. One key measure of the effectiveness of a reorganization is whether it will result in the public receiving better government services.
Reorganization Should Maintain or Improve Accountability. A reorganization should result in a government structure where the Legislature and the public can identify the person or entity responsible for management of a program and hold that person or entity accountable for achieving defined goals and objectives. The reorganization plan should delineate the roles and responsibilities of each of the divisions within the new or expanded department or entity that will assume responsibility for transferred programs and administrative functions.
Reorganization Should Be Based Upon a Policy Rationale. A reorganization should be consistent with an underlying policy rationale to address a problem or inefficiency that has been clearly identified. For example, facilitating better integration of programs that provide similar benefits, such as health insurance benefits, is a policy rationale for shifting a program from one department to another.
Reorganization Should Reflect Legislative Priorities. A reorganization should be consistent with priorities that the Legislature has set for a program or government function.
Here we provide our assessment of whether the proposed elimination of MRMIB makes sense based upon the general principles already outlined in this analysis.
Proposal Would Not Immediately Improve Efficiency. No positions are eliminated as a result of the elimination of MRMIB and the transfer of MRMIP, AIM, and CHIM. Furthermore, no overlapping or duplicative functions would immediately be eliminated as a result of the transfer. The MRMIB staff would move from their current offices to new offices provided by DHCS. According to DHCS, the costs of moving the employees to their new offices is minor and absorbable within DHCS’s budget. Based upon discussions with DHCS, the administrative positions for MRMIP, AIM, and CHIM would continue to perform the same workload after they are transferred to DHCS. The DHCS indicates that after its managers had more experience administering these programs, it could potentially identify opportunities and implement changes to improve efficiency and eliminate duplicative functions.
Unclear Whether Transition Would Improve Effectiveness. The reorganization could contribute toward the fulfillment of DHCS’s mission. (DHCS’s mission is to provide low–income Californians with access to affordable, high–quality health care, including medical, dental, mental health, and substance use disorder services and long–term services and supports.) However, the administration has not provided any information to support the conclusion that the transitions would immediately result in the public receiving better government services. In discussions with DHCS, the department indicated that after its managers had more experience with the programs, it would potentially be able to identify ways to improve program effectiveness.
Reorganization Unlikely to Maintain or Improve Accountability. Programs administered by MRMIB receive significant oversight due to monthly public meetings where MRMIB’s staff report to the board about the programs it manages. These regular public meetings of the board and the monthly reporting of key program data provide a greater level of transparency than is typical of most state–administered health programs. After the transition, these monthly meetings would no longer occur.
The MRMIB’s staff prepare an estimate of expenditures, or estimate package, for AIM and CHIM that provide a significant amount of fiscal detail on these programs. The estimate packages are provided to the Legislature twice every year, on January 10 and again on May 14 as part of the Governor’s May Revision of the budget plan. It is unclear whether a comparable amount of fiscal information would be provided in estimate packages prepared by DHCS after the transition.
Some Components of Reorganization Are Based Upon a Policy Rationale. In discussions with DHCS, the department indicates that transferring AIM and CHIM from MRMIB to DHCS, would move two programs that interact with Medi–Cal into the same department where Medi–Cal is administered. This could facilitate better coordination between Medi–Cal administrators and AIM and CHIM administrators. This is a sound policy rationale because AIM and CHIM wrap around the Medi–Cal Program with the objective of providing health services to certain targeted low– to middle–income populations who are ineligible for Medi–Cal. Closer integration could potentially lead to a better coordinated continuum of care for persons eligible for these programs. However, it is unclear how the transition of MRMIP could result in better coordination of services for state health programs.
As discussed above, as budgeted, the proposal to eliminate MRMIB meets some but not all of the criteria against which proposed governmental reorganizations are typically judged. Therefore, to assist the Legislature’s evaluation of this proposal, we recommend the Legislature require DHCS to report at budget hearings on how the elimination of MRMIB and the transfer of the three programs it currently administers to DHCS would address the following criteria for a government reorganization.
- How Will the Proposed Reorganization Improve Efficiency? How would the proposed reorganization improve efficiency both in the next fiscal year and in following years? The DHCS should also report on how and when they will keep the Legislature informed of any efficiencies that are ultimately achieved.
- How Will the Proposed Reorganization Improve Effectiveness? How would the proposed reorganization improve the effectiveness of the programs transferred to DHCS? Specifically, will it result in the public receiving better services?
- How Will the Proposed Reorganization Improve Accountability? The department should report on whether it will continue to provide the same amount of fiscal information about the transition programs that is currently annually provided by MRMIB on January 10 and at the time of the May Revision.
- What Is the Policy Rationale for the Reorganization? The department should report on the administration’s policy rationale for proposing the reorganization.
Based on the information provided to us from the administration, there is some basis to go forward with the transition but the administration has not made a compelling case that there would be an immediate improvement in the efficiency or effectiveness of the programs that would transition from MRMIB to DHCS. Furthermore, we find that there would likely be a loss of fiscal transparency if the transition were to be approved. Therefore, the Legislature should mainly weigh whether the administration’s policy rationale is compelling and whether it aligns with legislative priorities when deciding whether or not to approve the Governor’s proposal.
The DSH provides inpatient mental health services at five state hospitals (Atascadero, Coalinga, Metropolitan, Napa, and Patton) and at three psychiatric programs located on the grounds of California Department of Corrections and Rehabilitation (CDCR) prisons (Vacaville, Salinas, and Stockton). The hospitals provide treatment to approximately 5,400 patients with a variety of mental health needs. Patients at the state hospitals fall into one of two categories: civil commitments or forensic commitments. Civil commitments are generally referred to the state hospitals for treatment by counties. Forensic commitments are typically committed by the courts and include individuals classified as incompetent to stand trial (IST), not guilty by reason of insanity, mentally disordered offenders (MDOs), or sexually violent predators. In addition, the three colocated DSH psychiatric programs treat inmates referred by CDCR. (These inmates are called Coleman commitments because their psychiatric care is the subject of a lawsuit known as Coleman v. Brown, which involves allegations that the state prison system provided constitutionally inadequate psychiatric care for inmates.)
Currently, over 90 percent of the patient population is forensic in nature and there has been a steady increase in waitlists for forensic commitments. In contrast, the population of civil commitments has remained relatively stable. As of January 2014, the department had nearly 500 patients awaiting placement.
The Governor’s budget proposes total expenditures of $1.6 billion ($1.5 billion from the General Fund) for DSH operations in 2014–15, which reflects a less than 1 percent increase from the revised 2013–14 funding level. The department’s budget includes increased funding for several proposals, including plans to operate 242 more beds than were budgeted in 2013–14, initiate a program to manage bed space on a statewide level, and develop a cost estimate for enhanced security units.
As mentioned above, DSH has seen an increase in waitlists for forensic patients. The largest waitlists are for IST and Coleman commitments. As of January 2014, there were 393 IST and 63 CDCR patients awaiting placement in DSH facilities. Such long waitlists are problematic because they could result in increased court costs and higher risk of DSH being found in contempt of court orders to admit patients. This is because DSH is required to admit patients within certain time frames and can be required to appear in court or be held in contempt when it fails to do so. In light of these concerns, the 2013–14 budget provided $22.1 million to increase treatment capacity for IST and MDOs by 155 beds.
The 2013–14 budget also included reductions in funded beds at DSH–Vacaville and DSH–Salinas Valley, based on the assumption that Coleman patients in these facilities would be relocated to the newly activated California Health Care Facility (CHCF) in Stockton, which is operated by CDCR. The transfer was scheduled for completion by December 2013, but has since been delayed because of difficulties hiring staff at CHCF.
As we discuss below, the Governor’s budget proposes additional funding to DSH to support additional beds for CDCR and IST patients. These proposals are accompanied by staffing increases based on the department’s patient to staff ratios.
Coleman Population Adjustments. In view of the waitlist for beds for forensic patients, as well as the delay in the complete activation of the mental health beds at CHCF, the Governor’s budget proposes to permanently maintain 137 beds for Coleman patients at DSH–Vacaville and DSH–Salinas Valley. (For 2013–14, the Governor’s budget proposes to redirect $13.3 million in savings related to the delayed activation of CHCF to support the 137 beds.) For 2014–15, the budget proposes a $26.3 million General Fund augmentation and 204 positions to support the beds at DSH–Vacaville and DSH–Salinas Valley. The 2014–15 budget would maintain the previously approved funding and positions to support the beds at CHCF.
IST Adjustments. In addition, the Governor’s budget includes a $27.8 million General Fund augmentation and 251 positions to activate 105 new beds for IST patients. Specifically, the budget proposes activating 105 beds at DSH–Coalinga, which would be filled with current MDO patients transferred from DSH–Napa, DSH–Patton, DSH–Metropolitan, and DSH–Atascadero. The beds made available from this transfer would then be filled with IST patients.
Gap Exists Between Budgeted Population and Census. In recent years, there has been a significant mismatch between the size of the population DSH is funded to serve and the number of patients actually in the hospitals. This is because while DSH has received funding increases in recent years to support additional beds, the department has not been able to activate the planned beds at the rate expected—resulting in much lower–than–expected growth in the patient population. As shown in Figure 13, DSH has consistently maintained a smaller population than beds for which it is budgeted to support. In total, DSH is currently budgeted for 616 more beds than it has patients. Specifically, the department is overbudgeted by 365 beds in state hospitals and 251 beds in the psychiatric programs. Despite this, the department has not reverted unused funds to the General Fund at the end of the year.
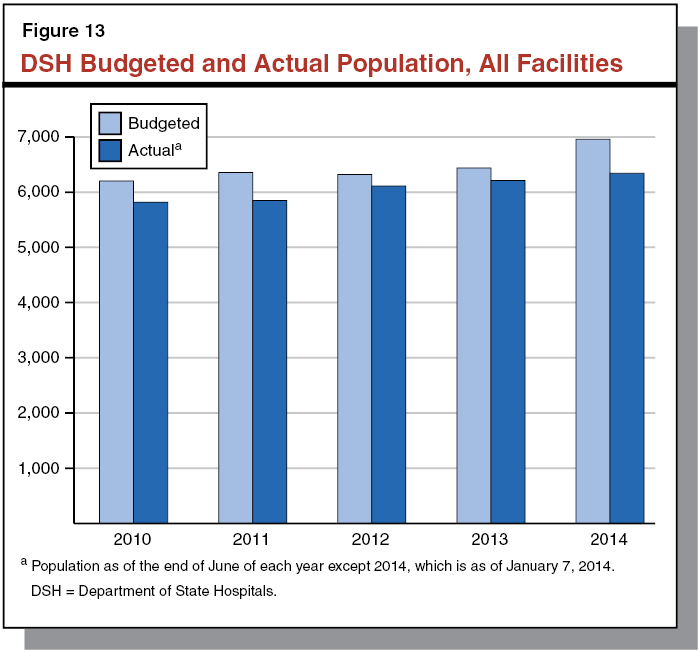
There are several reasons that may explain why there is a gap between the population DSH is budgeted to serve and the population it actually serves. First, DSH is not always able to utilize beds for which it has received funding. For example, DSH often has difficulty hiring clinical staff to support available bed space, and therefore cannot utilize available beds. Also, patients are committed to specific locations by referring agencies (such as courts), so some available beds may not be filled because patients are not being referred to those locations.
Second, according to DSH, it must receive funding to staff beds that will remain vacant for a portion of the year. For example, the department indicates that some beds are budgeted for certain commitment types—such as for IST patients—and those beds must be open for only those commitment types. Also, a certain percentage of beds must remain vacant for patients who are attending court hearings or transferring locations. While we acknowledge that it is necessary to maintain some number of vacant beds for this purpose, it is unclear from the information provided by DSH that the current number of vacant beds is appropriate. We note, for example, that the number of vacant beds—both at various DSH facilities and by commitment type—changes frequently with little evidence of corresponding changes in care. This suggests that DSH has been able to operate with fewer vacant beds than they currently have.
The gap between the budgeted and actual population is problematic for two reasons. First, it suggests that the department is overbudgeted to serve its current population. Second, it suggests that approving additional funds for the department will not necessarily result in an increase in population or a reduction in waitlists. Instead, additional funding may only result in funding for positions that DSH is unable to fill, not an increase in hospital capacity. For example, despite the Legislature approving funding to support 155 additional beds in the 2013–14 budget for IST and MDO populations, these populations have actually declined by 30 patients statewide.
Vacancy Rates Remain a Concern. The Governor’s budget assumes that additional staff can be quickly hired to support additional patients. However, it is uncertain whether the department will be able to hire staff within the expected time frame. Moreover, DSH currently has high vacancy rates at DSH–Vacaville and DSH–Salinas Valley, where it proposes to maintain beds for Coleman patients. The DSH has historically had difficulty filling positions. As shown in Figure 14, the vacancy rates at DSH–Vacaville and DSH–Salinas Valley are particularly high—34 percent and 33 percent, respectively. Given these vacancy rates, it is unlikely that the positions proposed in the budget for these facilities will be filled. We note that DSH does use some registry staff to provide care and offsets those registry costs with savings from having vacant positions. (Registry staff provide services on an hourly basis when civil servants are unavailable.) However, the department’s current use of registry staff does not seem to significantly reduce the gap between the budgeted and actual populations. Therefore, it seems unlikely that increased funding for staff—whether it results in filled vacancies or increased registry funding—would result in an increase in the population or reduction in patient waitlists.
Figure 14
DSH 2013–14 Vacancy Ratesa
|
Location
|
Budgeted Positions
|
Vacant Positions
|
Percent Vacant
|
|
Atascadero
|
1,827.8
|
254.4
|
14%
|
|
Coalinga
|
1,750.0
|
303.5
|
17
|
|
Metropolitan
|
1,218.0
|
178.4
|
15
|
|
Napa
|
1,965.0
|
160.5
|
8
|
|
Patton
|
2,032.9
|
181.6
|
9
|
|
Salinas Valley
|
315.7
|
103.5
|
33
|
|
Vacaville
|
472.7
|
159.6
|
34
|
|
Totals
|
9,582.1
|
1,332.5
|
14%
|
Implementation of Alternatives to Capacity Could Reduce Waitlists. Because of the dramatic increase in the waitlists for IST and Coleman patients, the department has initiated some steps in recent years to help manage the waitlists. For example, traditionally DSH has treated the IST population in state hospitals. In 2007–08, however, the Legislature approved a pilot project allowing counties to provide Restoration of Competence (ROC) services to IST patients in county jail. The pilot showed that those services could be provided at a significantly lower cost to the state. In 2012–13, the Legislature authorized DSH to continue this on an ongoing basis and the department is currently considering expanding this program. In addition, DSH is also involved in a workgroup established by the administration to identify reasons for the increase in IST patient commitments and possible solutions for managing the resulting increase in this population. The results of these efforts, and their impacts on patient waitlists, have not yet been realized. The pilot program and workgroup may result in patient waitlist reductions, which could reduce the department’s need for additional capacity and thus the need for the Governor’s proposed augmentations.
Current Staffing Ratios Not Based on Rigorous Analysis. Until 2013, DSH was under a consent decree pursuant to the federal Civil Rights for Institutionalized Persons Act, which is designed to protect individuals in public institutions such as mental hospitals. The consent decree was reached between the U.S. Department of Justice and DSH in 2006 to address identified deficiencies. The terms of the consent decree, however, had limited the state’s options with respect to adjusting DSH’s staffing. Given that the department is no longer under court oversight, it now has the ability to reassess whether its existing staffing levels are appropriate.
However, the department has not undertaken an independent analysis of its staffing needs since the termination of the consent decree. As such, it is not clear if the department employs reasonable staff to patient ratios given the types of patients it treats and the physical layout of its facilities. We note, for example, that an audit conducted by DOF in 2008–09 found that DSH’s staffing model did not accurately reflect its workload and that the department was not efficiently using some of its staff. Moreover, as mentioned earlier, the department does not have standards for the number of beds that should remain vacant to account for patients who are away at court or being transferred to other locations, as well as the number of staff positions necessary for such beds. Without such an analysis it is unclear whether DSH’s current staffing patterns are appropriate. It is possible that DSH has too much or too little staff, which would impact whether the Governor’s proposed augmentation is appropriate.
In view of the above concerns, we recommend that the Legislature reject the Governor’s proposal to provide additional funding for increased bed capacity at DSH–Vacaville, DSH–Salinas Valley, and at the various facilities due to receive additional IST bed capacity. We also recommend that the Legislature direct DSH to report at budget subcommittee hearings this spring on (1) why the patient population remains stable despite growing waitlists, (2) why there is a mismatch between their budgeted capacity and their patient population, (3) what steps the department is taking to address its high vacancy rate, and (4) the department’s progress on expanding ROC services in county jails and the findings of the IST working group. Such information could assist the Legislature in making a determination about the appropriate level of budget and staffing increases necessary to treat the DSH patient population. We further recommend that the Legislature direct DSH to develop a proposal to contract for an independent staffing analysis to determine appropriate staffing levels for each facility. These staffing ratios should be based on licensing requirements, clinical need, necessary bed vacancies, and other factors as deemed appropriate by the independent assessor.
Under certain circumstances, counties, courts, or CDCR can make commitments to either a specific hospital or psychiatric program or to the DSH system at large, without reference to a specific institution. Currently, the process for assigning an individual is largely focused on legal requirements rather than clinical need. Specifically, assignment to a specific location is at the discretion of the referring entity based on a patient’s legal commitment and security risk, statutory requirements of the locations, agreements with communities and CDCR, and DSH policy. Once in a DSH facility, a patient may be transferred to a different location. However, for that transfer to occur a patient must first be admitted and stabilized.
We find that the current system for commitments can result in unintended consequences. For example, some locations may be overutilized while others may be underutilized, which can lead to delays in placement. While DSH may transfer patients to address those capacity concerns, currently such transfers occur on an ad hoc basis. In addition, commitments that assign patients to specific locations may reduce DSH’s clinical effectiveness, because it prevents the department from assigning patients to the facility to which they are best suited. The ability to do so is important because specialty care for specific medical or mental health diagnoses varies by location. For example, DSH–Patton has a unit for individuals with certain chronic diseases and DSH–Metropolitan has a skilled nursing facility. Moreover, because each facility may be required to intake numerous patient types, each facility must maintain the ability to house each of these patient types. This increases costs because it prevents facilities from achieving the efficiencies possible from specialization and the economies of scale available from concentrating specific patient types in certain facilities.
The Governor’s budget for 2014–15 proposes $1.1 million in General Fund support and the establishment of ten limited–term positions for DSH to create a patient management and bed utilization unit. According to the administration, the proposed unit would serve several key purposes, including:
- Centralized Patient Placement and Waitlist Management. The new unit would centralize and coordinate patient placement at a statewide level. The Governor’s budget proposes having (1) courts, counties, and CDCR commit patients to DSH at large, rather than to specific institutions and (2) the patient management unit determine the specific location for placement. The unit would also centralize patient waitlists, which are currently maintained through several state and local systems.
- Centralized Population Information. The new unit would also create reports tracking bed vacancies, facility populations, patient diagnoses, commitment type, county of origin, length of stay, and recidivism rates.
Proposal Has Merit. . . As described above, the current disconnected system of patient placement has numerous drawbacks. The Governor’s proposal has the potential to address many of the issues. For example, the proposal might allow DSH to find placements for patients more quickly, which could reduce court orders requiring DSH to accept specific patients from waitlists. It could also improve the department’s ability to budget for each institution, because it would allow DSH to place patients in available bed space rather than having some facilities have empty space while others have patients waiting for entry. It could also reduce lengths of stay by placing patients in the most clinically appropriate setting.
We note, however, that there could be some additional costs associated with the patient management unit. For example, patients assigned to locations far from their county of commitment might incur additional travel costs for court visits. In addition, evaluating patients before placement could also slow the placement and transfer processes, resulting in longer lengths of stay. Despite this, the potential operational benefits of the proposal would likely outweigh such drawbacks.
. . . But Department Lacks Authority to Fully Realize Benefits of Management Unit. The DSH currently does not have the statutory authority to implement patient placement programs, and the Governor’s proposal does not include trailer bill language to provide the department with that authority. Though some courts and counties permit DSH to manage patient placement, the discretion to allow this remains with those entities, not the department. Even if DSH were to establish a patient management and bed utilization unit, it would be unable to fully realize the benefits of such a program because, without statutory changes, referring entities would remain the arbiters of patient placement.
Though the administration’s proposal could result in increased efficiency and potential cost savings, until statutory language exists permitting DSH to fully control the placement of the patients committed to its care, the benefits of the patient management unit cannot be fully realized. Therefore, we recommend the Legislature support the administration’s proposal to create a patient management and bed utilization unit and adopt trailer bill language clarifying that DSH has the authority to fully control patient placements.
Historically, DSH has provided treatment to those civil commitments without a history of violence. However, as noted above, the forensic population has been growing. Currently more than 90 percent of patients are committed through the criminal justice system. There are concerns that this shift has resulted in increased acts of aggression by patients toward other patients and staff. For example, since 2008, three murders have occurred in DSH facilities and the department has seen an increase in incidents that require first aid or hospitalization. Because DSH hospitals were built for civil commitments, the facilities do not have secure units to house aggressive patients on a short– or long–term basis. In addition, DSH facilities are currently licensed as acute psychiatric hospitals or intermediate care facilities, and licensing standards for those facilities preclude the use of secure units.
The Governor’s budget provides $1.5 million in General Fund support to DSH for the Department of General Services (DGS) to prepare an analysis, estimate, and infrastructure design for the development of approximately 44 enhanced treatment units (ETUs) in DSH hospitals. The rooms in these units would serve several purposes, including: providing temporary secure environments for violent patients and patients transferring to CDCR facilities, as short–term housing for patients with behavioral problems, and as longer–term housing for violence–prone patients. The units would be designed to have individual patient rooms and externally locking doors.
The Governor also proposes the development of a Forensic Needs Assessment Panel (FNAP) and Forensic Needs Assessment Team (FNAT). The FNAP could be comprised of clinical executives and review placement and treatment issues. The FNAT would include psychologists with experience in forensic assessment, and perform risk assessments of patients referred for enhanced treatment, evaluate ETU patients’ treatment plans, and follow the patient through placement in the ETU. The proposal also includes proposed criteria for ETU admission and evaluation, which include time frames for clinical evaluation, placement, and reconsideration of ETU placement. The proposed criteria also include standards for treatment and case management time frames, as well as unspecified increases in clinical oversight and treatment.
As noted above, current licensing standards do not permit the use of locked units in DSH hospitals. The administration indicates that it is pursuing various amendments and additions to acute psychiatric hospital regulations that would permit DSH hospitals to create units with individual rooms and external door locks. However, such language has not yet been provided to the Legislature.
As mentioned above, the administration has not provided language that would give DSH the authority it seeks. As such, the details of the project remain uncertain. For example, there is no information about the approved lengths of stay or types of locked facilities that would be permitted under statute. Without that clarity, DGS may not be able to create an accurate budget package or determine the most appropriate infrastructure design for these units. We are also concerned that the lack of specificity about the ETUs creates uncertainty about DSH’s ability to build the units. Under the administration’s proposal, it is unclear whether each hospital will be permitted to maintain ETUs or whether units will be required at each location. Additionally, it is unclear what design specifications may be required, such as room size, bathroom facilities, or type of door lock. Without such information, it is unclear how DGS will be able to conduct the proposed analysis. Because each hospital has a different physical plant design, some hospitals may not meet those specifications, or it may be prohibitively expensive to build the units.
In light of these concerns, we recommend that the Legislature reject the Governor’s proposed $1.5 million to obtain a DGS study of ETUs. While we do not have major concerns with the proposal to consider the development of ETUs in DSH hospitals, we are concerned that planning the units without having specific guidelines could result in unnecessary costs.