Governor Proposes to Increase Share of Cost for AIDS Drug Assistance Program Enrollees
Background
Below we provide background information on the AIDS Drug Assistance Program (ADAP) that describes who is eligible for the program and recent enrollment trends.
AIDS Drug Assistance Program. The ADAP is administered by the Office of AIDS (OA) within the Department of Public Health. The ADAP helps to ensure that people living with Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) have access to HIV medication. The federal government has mandated that certain federal funds which support ADAP must be the payer of last resort; therefore, all ADAP applicants must be screened to determine if they have private insurance or are eligible for other government programs that provide HIV medications before they can be enrolled in ADAP. Eligibility for ADAP is currently recertified annually. Under a new federal requirement, by the end of the 2012 calendar year, an ADAP enrollee’s eligibility for the program will be recertified twice every year. Approximately 39,000 people received ADAP services during 2010-11. Generally, the average length of enrollment in ADAP was about seven months.
Current Eligibility Requirements and Cost Sharing. Individuals are generally eligible for ADAP if they have been diagnosed with HIV, are a California resident 18 years of age or older and have a federally adjusted gross income below $50,000. Enrollees in ADAP with adjusted gross incomes less than 400 percent of the Federal Poverty Level (FPL) have access to drugs on the ADAP formulary free of charge as long as they are prescribed by a licensed physician and lack private insurance that covers the medications or do not qualify for no-cost Medi-Cal. (For 2011-12, 400 percent of FPL for a single person is $43,560.) Enrollees with adjusted gross incomes between $43,560 and $50,000 may be eligible for partial assistance from ADAP to help pay the cost of their drugs. Enrollees with incomes in this range must pay a monthly copayment based on income, regardless of whether the enrollee has private health coverage or has other qualifying factors.
Thousands of ADAP Enrollees Are Shifting to Other Government Health Programs. The majority of enrollees who are shifting from ADAP to other government health programs are shifting into the Low Income Health Program (LIHP), which received federal approval on November 2, 2010 as part of the state’s Medi-Cal “Bridge to Reform” waiver. The LIHP is a voluntary program implemented at the county level and supported by county and federal funds that provides medical coverage for low-income adults aged 19 to 64 years old who are not otherwise eligible for Medi-Cal. Counties have some flexibility to cap income eligibility levels at 200 percent of FPL or at a lower FPL such as 133 percent. The LIHPs provide medical services such as primary care and pharmaceuticals, including HIV medications. The first ten counties to implement LIHPs include: Alameda, Contra Costa, Kern, Los Angeles, Orange, San Diego, San Francisco, San Mateo, Santa Clara, and Ventura. Nearly 80 percent of ADAP clients reside in these counties. The governor’s proposal estimates that 4,800 ADAP enrollees will shift from ADAP to LIHPs in 2011-12 and an additional 5,272 ADAP clients will shift to LIHPs in 2012-13. The OA is currently working with the Pharmacy Benefits Manager to explore options for informing eligible ADAP enrollees of their option to transition to LIHPs.
The shift from ADAP to LIHP accounts for most of the ADAP enrollees that are projected to move out of ADAP and into another government health program that provides HIV medication. However, the administration also projects ADAP enrollees will move out of ADAP and into the Pre-Existing Condition Insurance Plan (PCIP) and the Health Insurance Premium Payment (HIPP) program in the current year and the budget year. The PCIP is administered by the Managed Risk Medical Insurance Board and was created by the federal Affordable Care Act of 2010 to establish a federally funded high-risk insurance pool for persons who have difficulty purchasing insurance, usually because of a preexisting medical condition. Enrolling eligible ADAP patients in PCIP and HIPP enables ADAP enrollees to obtain, or maintain, health insurance and is cost-effective for ADAP. About 428 ADAP enrollees are expected to shift to PCIP in 2011-12 and about another 445 are expected to shift in 2012-13.
The OA’s HIPP program pays the private insurance premiums of ADAP enrollees who have comprehensive health insurance with prescription drug benefits and ADAP pays the drug deductibles and co-pays. About 990 ADAP clients are expected to shift to HIPP in 2011-12, and the total ADAP clients enrolled in HIPP is expected to grow to about 1,039 in 2012-13.
The ADAP Is Funded From Four Sources. The ADAP is funded from four sources as follows:
-
General Fund. The state General Fund is comprised of revenues from property and income taxes.
-
Federal Fund. The ADAP receives federal funding from the Health Resources and Services Administration through the Ryan White Program. The Ryan White Program was enacted in 1990 to provide care and support services to individuals and families affected by HIV/AIDS who have no other source of coverage or face coverage limits. The federal government requires that these funds be used as the payer of last resort.
-
Reimbursements. The ADAP will receivefunding through reimbursements from the Department of Health Care Services in 2010-11, 2011-12, and 2012-13 as a result of temporary additional federal resources.
-
Special Fund. The ADAP Special Fund supports the provision of ADAP services and is funded by rebates from manufacturers with products on the ADAP formulary. Rebates are generally received six to nine months after program expenditures occur and the annual total amount of the rebates fluctuates.
In any given year, OA attempts to minimize the need for General Fund support by maximizing the use of special funds, reimbursements, and federal funds.
Governor’s Proposal
The Governor’s budget plan proposes to reduce total funding for ADAP by $82 million from $477 million in 2011-12 to $395 million in 2012-13. The actual funding for 2010-11, revised funding for 2011-12, and the proposed funding for 2012-13 is shown by fund source in Figure 1.
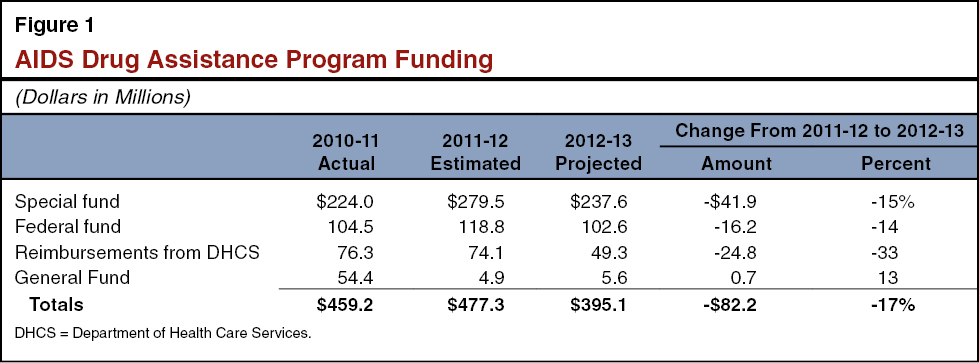
The changes in funding from 2011-12 to 2012-13, shown in Figure 1, reflect the Governor’s proposal to reduce costs and continue implementing a federal mandate to ensure ADAP is the payer of last resort. Specifically, the Governor proposes to impose a share of cost on enrollees with incomes below 400 percent of FPL and recognize avoided costs from ADAP enrollees shifting to other public health programs. Here we describe both the proposed savings and the estimated avoided costs in more detail.
Impose a Share of Cost on Enrollees With Incomes Below 400 Percent of FPL. In order to achieve General Fund savings of $14.5 million the administration proposes to increase the client share of costs to the maximum percentages allowable under federal law for most ADAP enrollees. The proposed share of cost would be based on the ADAP enrollee’s income and would only be charged to the individual when they are receiving medications through ADAP. Effective July 1, 2012, the costs for most ADAP enrollees would be increased as follows:
-
Enrollees with annual incomes less than 100 percent of FPL ($10,890 for a single person) would have no share of cost.
-
Enrollees with annual incomes between 101 percent and 200 percent of FPL ($10,891 to $21,780 for a single person) would a pay 5 percent share of cost, or between $45 to $91 each month they are enrolled in ADAP.
-
Enrollees with annual incomes between 201 percent and 300 percent of FPL ($21,781 to $32,670 for a single person) would pay 7 percent share of cost, or between $127 to $191 each month they are enrolled in ADAP.
-
Enrollees with annual incomes between 301 percent and 400 percent of FPL ($32,671 to $50,000 for a single person) would pay 10 percent share of cost, or between $272 and $417 each month they are enrolled in ADAP.
We note that the ADAP enrollees with private insurance will pay 2 percent of their income as a share of cost.
The Governor’s proposal to increase the share of cost borne by ADAP patients makes allowances for scenarios where it would not be cost-effective for ADAP to charge an enrollee the proposed share of cost by adjusting the share of cost for some enrollees and exempting others. For example, ADAP pays only the out-of-pocket costs for enrollees who have private insurance, yet still receives rebates on the full costs of these drugs. In order to avoid losing the rebate revenues for these patients, the share of cost for clients with private insurance was adjusted to ensure that it does not exceed the financial assistance provided by ADAP.
Governor’s Budget Plan Assumes Savings Resulting From Shift to LIHP, PCIP, and HIPP. The Governor’s budget plan assumes:
-
The shift of ADAP enrollees to LIHPs will save ADAP $19.9 million in 2011-12 and $106.8 million in 2012-13.
-
The shift of ADAP enrollees to PCIP will save ADAP $1.8 million in 2011-12 and $4.6 million in 2012-13.
-
The shift of ADAP enrollees to HIPP will save ADAP $1.9 million in 2011-12 and $4.4 million in 2012-13.
Savings From Share of Cost Proposal Are Related to LIHP Shift. The Governor’s proposed budget for ADAP assumes that the implementation of cost sharing in ADAP would speed up the transition of some ADAP enrollees to LIHPs, because some LIHP-eligible ADAP enrollees would be able to save money by making the transition.
Analyst Comments and Concerns
Amount of Savings From Shift to LIHP Is Uncertain. The Governor’s budget assumes that the implementation of cost sharing would lead to increased ADAP saving as it would speed up the transition of ADAP enrollees to LIHPs. If ADAP enrollees do not know that they have the option of transitioning to LIHPs sooner than their annual ADAP eligibility reexamination, or if the share of cost was not implemented, projected savings may be eroded. If ADAP enrollees eligible for LIHPs do transition at a slower rate than projected, the administration estimates that the assumed savings could be decreased by up to $1.9 million.
There May Be Serious Public Health Consequences. If implementing an increased share of cost results in some ADAP enrollees dropping out of ADAP because they cannot afford to pay the increased costs and they stop taking their HIV medications, there could be serious personal and public health consequences. Taking effective HIV medication prevents transmission of HIV as well as morbidity and mortality from AIDS. The administration’s estimate methodology does account for clients who have other insurance and drop out of ADAP because their monthly share of cost would exceed the payer’s monthly out-of-pocket medication costs. However, the estimate methodology does not account for clients who drop out of ADAP because they cannot afford to pay their ADAP share of costs and therefore stop taking HIV medications. The ADAP estimate states that there is no accurate way to estimate the latter.
Analyst’s Recommendations
We recommend approval of the administration’s proposal to increase the share of cost borne by ADAP clients due to the state’s fiscal condition, not on a policy basis. However, as an alternative to the Governor’s proposal, the Legislature could impose a lower level of cost sharing than the level proposed under the Governor’s plan. Increasing the share of cost, but at a lower level than proposed by the Governor, would generate less savings, (how much savings decrease would depend on the cost-sharing levels that are ultimately imposed) but would lessen the potential for negative personal and public health consequences.
We recommend that ADAP report in budget hearings on the feasibility of an exception process to allow ADAP enrollees who might otherwise stop taking HIV medication as a result of the Governor’s plan to have their cost-sharing obligation waived. Such an exception process could help to mitigate the personal and public health consequences associated with increasing the share of cost.