November 14, 2013
Pursuant to Elections Code Section 9005, we have reviewed the
proposed constitutional and statutory initiative (A.G. File No. 13‑00
22) relating to conditions for amending, repealing, replacing, or
rendering inoperative the Medi-Cal Hospital Reimbursement Improvement
Act of 2013—current law that concerns the imposition of fees on certain
private hospitals.
Background
Overview of Medi-Cal
Medi-Cal Administration and Coverage. The
federal Centers for Medicare and Medicaid Services (CMS) administers the
federal Medicaid Program. In California, this federal program is
administered by the state Department of Health Care Services (DHCS) as
the California Medical Assistance Program, and is known more commonly as
Medi-Cal. This program currently provides health care benefits to about
7.9 million low-income persons who meet certain eligibility requirements
for enrollment in the program (hereafter referred to as the currently
eligible population). Under the Patient Protection and Affordable Care
Act (ACA), also known as federal health care reform, the state will
expand Medi-Cal to cover over one million low-income adults who are
currently ineligible (hereafter referred to as the expansion
population), beginning January 1, 2014.
Medi-Cal Financing. The costs of the
Medicaid Program are generally shared between states and the federal
government based on a set formula. The federal government’s contribution
toward reimbursement for Medicaid expenditures is known as federal
financial participation (FFP). The percentage of Medicaid costs paid by
the federal government is known as the federal medical assistance
percentage (FMAP).
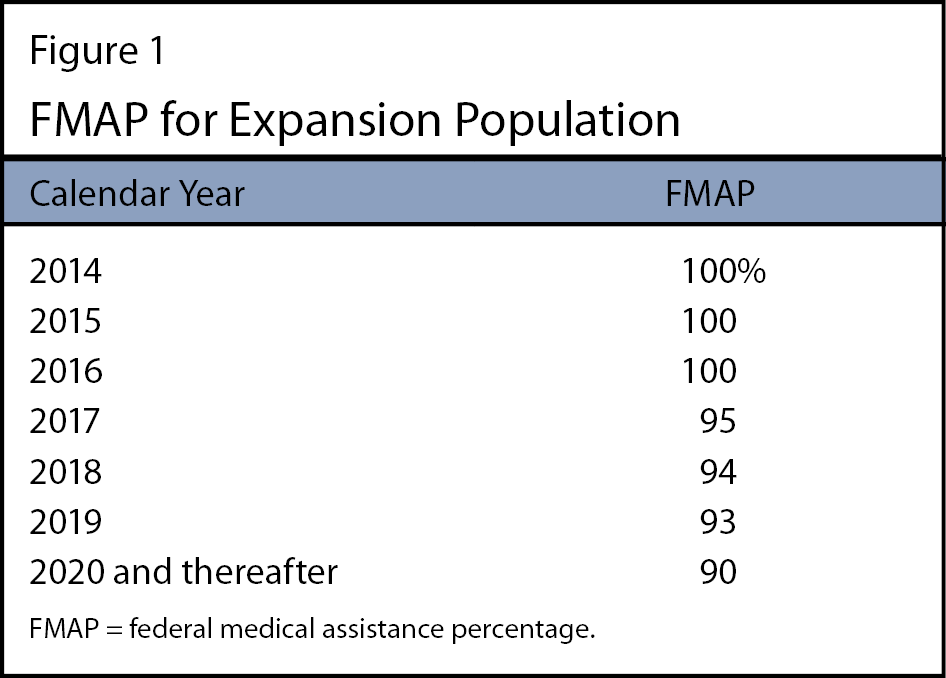
In general, the FMAP for Medi-Cal costs associated with the currently
eligible population has been set at 50 percent. (However, for certain
currently eligible subpopulations and certain administrative activities,
the state receives a higher FMAP percent.) As Figure 1 shows (see next
page), for three years beginning January 1, 2014, the FMAP for nearly
all Medi-Cal costs associated with the expansion population will be 100
percent. Beginning January 1, 2017, the FMAP associated with the
expansion population will decrease over a three-year period until
reaching 90 percent on January 1, 2020, where it will remain thereafter
under current federal law.
Federal Medicaid law permits states to finance the nonfederal share
of Medicaid costs through several sources, including (but not limited
to):
- State General Funds. State general
funds are revenues collected primarily through personal income,
sales, and corporate income taxes.
- Charges on Health Care Providers.
Federal Medicaid law permits states to (1) levy various types of
charges—including taxes, fees, or assessments—on health care
providers and (2) use the proceeds to draw down FFP to support their
Medicaid programs and/or offset some state costs. These charges must
meet certain requirements and be approved by CMS for revenues from
these charges to be eligible to draw down FFP. A number of different
types of providers can be subject to these charges, including
hospitals.
Medi-Cal Delivery Systems. Medi-Cal
provides health care through two main systems: fee-for-service (FFS) and
managed care. In the FFS system, a health care provider receives an
individual payment directly from DHCS for each medical service delivered
to a beneficiary. In the managed care system, DHCS contracts with
managed care plans to provide health care for Medi-Cal beneficiaries
enrolled in these plans. Managed care enrollees may obtain services from
providers—including hospitals—that accept payments from the plans. The
DHCS reimburses plans with a predetermined amount per enrollee, per
month (known as a capitation payment) regardless of the number of
services each enrollee actually receives.
Medi-Cal Hospital Financing
About 400 general acute care hospitals licensed by the state
currently receive at least one of three types of payments Medi-Cal makes
to pay for services for patients. As follows, these hospitals are
divided into three categories based on whether the hospital is privately
owned or publicly owned, and who operates the hospital.
- Private Hospitals. These are hospitals
owned and operated by private corporations.
- District Hospitals. These are public
hospitals owned and operated by municipalities and health care
districts.
- County Hospitals and University of California (UC)
Hospitals. These are public hospitals owned and
operated by counties or the UC system.
Below we describe the three types of payments—direct payments,
supplemental payments, and managed care payments—that Medi-Cal makes for
hospital services.
Direct Payments. Direct payments are
payments for services provided to Medi-Cal patients through FFS. The
nonfederal share of Medi-Cal direct payments to private and district
hospitals is funded from the state General Fund, while the nonfederal
share of direct payments to county and UC hospitals is self-funded.
Supplemental Payments. Supplemental
payments (considered a type of FFS payment) are made in addition to
direct payments. Medi-Cal generally makes supplemental payments to
hospitals periodically on a lump-sum basis, rather than individual
increases to reimbursement rates for specific services. There are
various types of supplemental payments related to hospital services
provided to Medi-Cal patients, including a category of payments to
private hospitals known as Disproportionate Share Hospital (DSH)
replacement payments that we discuss further later in this analysis.
Depending on the type of supplemental payment, the nonfederal share may
be comprised of General Fund support, revenues from charges levied on
hospitals, or other state and local funding sources.
Managed Care Payments. Managed care
payments are payments from managed care plans to providers for services
delivered to Medi-Cal patients enrolled in these plans. The capitation
payments that plans receive from DHCS are meant to cover the expected
costs to plans from making payments to providers, including hospitals.
The nonfederal share of capitation payments to managed care plans is
comprised of General Fund support, charges levied on hospitals, and
other state and local funding sources.
Federal Limits on FFS Hospital Payments.
Federal regulations specify that to be eligible for FFP, the total
amount of Medi-Cal FFS payments to private hospitals—that is, the sum of
all direct and supplemental payments for private hospital services—may
not exceed a maximum amount known as the upper payment limit (UPL).
(There are separate UPLs that apply to payments to hospitals owned and
operated by local governments such as counties, and hospitals owned and
operated by the state such as UC hospitals.) The UPL is a statewide
aggregate ceiling on FFS payments to all private hospitals. This means
there are no limits on FFS payments to individual private hospitals, as
long as total FFS payments to all private hospitals do not exceed the
UPL. In California, the UPL for hospital services has historically been
between 5 percent to 10 percent above the total costs incurred by
hospitals from providing these services, as defined under cost-reporting
procedures approved by CMS.
Federal Limits on Managed Care Hospital Payments.
The UPL does not apply to managed care payments for hospital
services. However, federal Medicaid law requires qualified actuaries to
certify capitation payments to managed care plans as being “actuarially
sound” before these payments may receive FFP. This certification
involves the actuaries’ assessment that capitation payments reflect
“reasonable, appropriate, and attainable” costs to plans from making
payments to providers, including hospitals. In practice, actuarial
soundness requirements directly limit the total amount of capitation
payments that DHCS may make to plans, and thus indirectly limit the
total amount of payments that plans may make to hospitals.
Hospital Quality Assurance Fee
Chapter 657, Statutes of 2013 (SB 239, Hernandez), enacts the
Medi-Cal Hospital Reimbursement Improvement Act of 2013 (hereafter
referred to as the Act). The Act imposes a charge known as a quality
assurance fee (hereafter referred to as the fee) on certain private
hospitals beginning January 1, 2014.
If approved by CMS and implemented, the fee imposed by the Act will
constitute the fourth consecutive hospital quality assurance fee program
implemented in California since 2009 (each of the prior three programs
had a statutory sunset date). The fee program authorized under the Act
is broadly similar in structure to the prior three fee programs. The Act
establishes a general structure for (1) how the fee is to be assessed
and (2) how the proceeds from the fee are to be spent. We describe both
components of this structure below.
Fee Assessment. Under the Act, the state
will assess the fee for each inpatient day at each private hospital. The
fee rate per inpatient day will vary depending on payer type, with the
highest rates assessed on Medi-Cal inpatient days and lower rates
assessed on days paid for by other payers, such as private insurance.
The fee rate ranges from $145 for each inpatient day covered by a
non-Medi-Cal payer to $618 per inpatient day covered by Medi-Cal.
Private hospitals will pay the fee in quarterly installments.
Use of Fee Moneys to Offset State Costs.
Under the Act, DHCS will administer and collect the fee from hospitals
and deposit the proceeds into the Hospital Quality Assurance Revenue
Fund. Moneys in this fund—the proceeds of the fee and any interest
earned on the proceeds—are available only for certain purposes. These
purposes include the following that serve to offset state costs (in
order of descending priority):
- Up to $1 million of the moneys annually will be allocated to
reimburse DHCS for the staffing and administrative costs related to
implementing the fee.
- A certain portion of the moneys (determined by a formula) will
offset General Fund costs for providing children’s health care
coverage, thereby achieving General Fund savings. Later we describe
how the allocation for this General Fund offset is to be determined
under the Act.
Use of Fee Moneys for Quality Assurance Payments.
After moneys in the fund are allocated to offset state costs,
the remaining moneys are available to support payment increases to
hospitals, collectively known as quality assurance payments (in order of
descending priority).
- A large portion of the moneys will provide the nonfederal share
of certain increases to capitation payments to managed care plans,
up to the maximum actuarially sound amount permitted by federal law.
The plans are required to pass along these capitation increases
entirely to private hospitals, county hospitals, and UC hospitals.
- A large portion of the moneys will provide the nonfederal share
of certain supplemental payments to private hospitals, bringing
total FFS payments to private hospitals as close as possible to the
UPL.
- Some of the moneys may be used to fund direct grants to public
hospitals. Any grant amounts retained by public hospitals are not
considered Medi-Cal payments, and thus are not eligible for FFP.
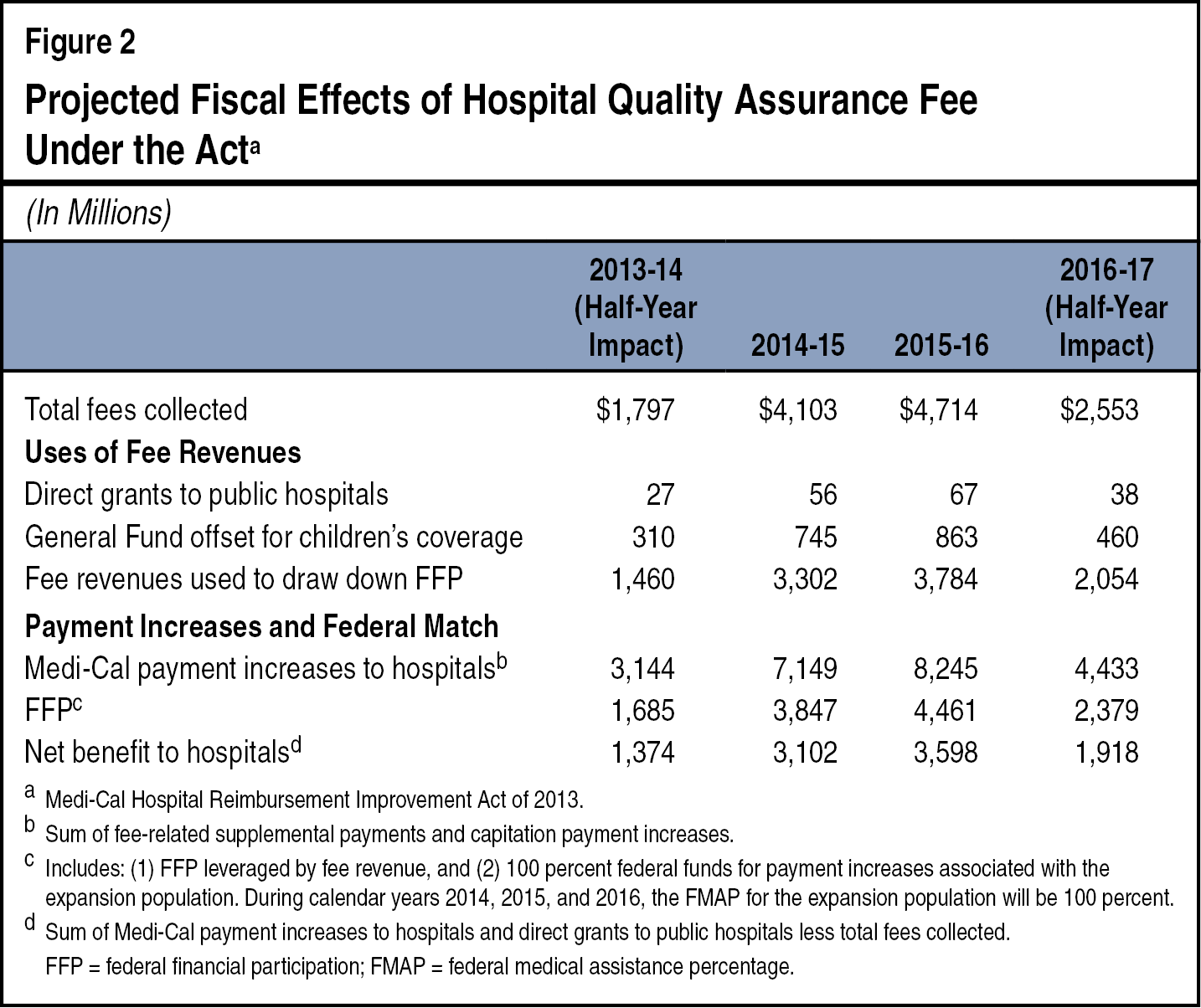
At the end of this background discussion, Figure 2 (see page 7)
displays our detailed projections of the annual amounts of fee moneys
used to offset state costs and support quality assurance payments to
hospitals under the Act.
Net Benefit and General Fund Offset for Children’s
Coverage. Under the Act, beginning July 1, 2014, the
annual amount of moneys used to offset General Fund costs for children’s
health care coverage will equal 24 percent of the “net benefit” to
hospitals, hereafter referred to as net benefit. (For the period between
January 1, 2014 and June 30, 2014, the amount of General Fund offset is
set at $155 million per quarter rather than a percentage of the net
benefit.) The Act defines net benefit as total fee revenue collected
from hospitals in each fiscal year, minus the sum of the following
quality assurance payments:
- Fee-funded supplemental payments and direct grants.
- Fee-related capitation increases for hospital payments.
Fee-related capitation increases consist of (1) fee-funded increases
related to hospital services for the currently eligible population and
(2) increases related to hospital services for the expansion population.
Due to the enhanced FMAP for the Medi-Cal expansion, the net benefit
from a capitation increase for the expansion population is generally
greater than the net benefit from an equal increase for the currently
eligible population. For example, a capitation increase of $100 million
for the currently eligible population would result in a net benefit of
roughly $50 million, since hospitals would provide the nonfederal share
for this increase through fee revenue. In contrast, the net benefit from
a capitation increase of $100 million for the expansion population would
be between $90 million and $100 million, depending on the FMAP in effect
for the year in question.
Fee Program Periods. The Act (1) specifies
the schedule of fee rates for the period between January 1, 2014 and
December 31, 2016, and (2) requires DHCS to periodically redevelop the
schedule of fee rates thereafter. Each schedule of fee rates will apply
to separate and consecutive “program periods,” each lasting no more than
three years. While the schedules may differ by program period, each
schedule will conform to the general structure for assessing the fee and
using the proceeds as specified in the Act. That is, for each program
period, DHCS will develop a schedule of fee rates that: (1) varies per
inpatient day by payer type, with higher rates assessed on Medi-Cal
days, and (2) enables the maximum amount of supplemental payments and
capitation increases for hospital payments that receive FFP.
The Act designates the period of January 1, 2014 through December 31,
2016 as the first program period, and the period of January 1, 2017
through June 30, 2019, as the second program period. Under the Act, DHCS
will determine the duration of subsequent program periods. During the
first program period, moneys in the Hospital Quality Assurance Revenue
Fund will be continuously appropriated without further legislative
action. In subsequent program periods, the Legislature will authorize
expenditures from the fund in the annual budget act.
FFS Maintenance-of-Effort (MOE) for Hospital Services.
The Act contains a provision to ensure that fee-related
moneys are used to supplement and not supplant existing funding for
hospital services provided to Medi-Cal patients. Specifically, the Act
stipulates that for hospital services provided to Medi-Cal patients
through FFS on or after January 1, 2014, the total amount of payments
supported by General Fund expenditures shall not be less than the total
amount that would have been paid for the same services on December 1,
2013. The Act specifically exempts DSH replacement payments from this
MOE requirement. We estimate that for the 2012‑13 fiscal year, the state
provided $2 billion in General Fund expenditures for the types of FFS
payments subject to the Act’s MOE requirement.
Conditions Rendering Fee Inoperative. The
Act includes several poison pill provisions specifying certain
conditions that would render the Act inoperative, including, but not
limited to:
- A judicial determination by the State Supreme Court or a State
Court of Appeal that revenues from the fee must be included for
purposes of calculating the Proposition 98 funding level required
for schools. We describe the Proposition 98 funding requirement
later in this analysis.
- A lawsuit related to the Act results in a General Fund cost of
at least 0.25 percent of General Fund expenditures authorized in the
most recent annual budget act (about $240 million in 2013‑14).
Absent conditions that would trigger the Act’s poison pill provisions
and render the Act inoperative, the Act becomes inoperative by its terms
as of January 1, 2017, due to a sunset provision. Therefore, under
current law, the fee will be in place only through the first program
period. (Moreover, authorization of the Hospital Quality Assurance
Revenue Fund expires on January 1, 2018.) However, as noted, the Act
prescribes a general structure for assessing the fee and using the
proceeds that would apply to subsequent program periods if legislation
were enacted to both extend the fee and maintain the fund.
Projected Fiscal Effects of the Act. Figure
2 provides our projections of (1) total fees collected as authorized by
the Act, (2) uses of the fee revenues under the Act, and (3) fiscal
effects on the state and hospitals of the Act.
Proposal
This measure would amend the State Constitution to (1) restrict the
Legislature’s ability to amend, repeal, or replace the Act by statute,
and (2) require voter approval to amend or replace the Act outside of
these restrictions. The measure would also amend by statute the Act’s
poison pill provisions and remove the Act’s sunset provision. The
measure would also remove the Act’s poison pill provision related to
Proposition 98, and amend the Constitution to specify that revenues from
the fee imposed by the Act and all interest earned thereon shall not be
considered as revenues subject to the Proposition 98 funding requirement
calculation. Below we describe the specific amendments that the measure
would place in the Constitution, and then describe the statutory
amendments that the measure would enact.
Constitutional Amendments
Requirements for Amending, Repealing, or Replacing the
Act. This measure amends the Constitution to require
two-thirds majorities in both houses of the Legislature to pass any
statute that repeals the Act in its entirety. In addition, any statute
that amends or replaces the Act requires voter approval in a statewide
election before taking effect, unless both of the following conditions
are met:
- The Legislature passes the statute with two-thirds majorities in
both houses.
- The statute (1) is necessary for securing federal approval to
implement the fee program, or (2) only changes the methodology used
for developing the fee or quality assurance payments.
We note that under current law, the Legislature may pass legislation
to broadly amend or repeal the Act with simple majorities in both
houses, although some amendments could require passage by two-thirds
majorities in both houses.
Fee Proceeds and Interest Exempt From Proposition 98
Calculation. Proposition 98, a constitutional amendment
adopted by voters in 1988 and amended in 1990, established a set of
formulas that are used to annually calculate a minimum state funding
level for K-12 education and the California Community Colleges. In many
cases, additional state General Fund revenues result in a higher
Proposition 98 funding requirement. This measure amends the Constitution
to specify that the proceeds of the fee and all interest earned on such
proceeds shall not be considered in calculating the Proposition 98
funding level required for schools.
Statutory Amendments
Changes to Poison Pill Provisions. The
measure amends the Act’s poison pill provisions in the following ways:
- The measure deletes the provision triggered by a state judicial
determination that revenues from the fee are subject to the
Proposition 98 calculation. As noted earlier in this analysis, the
measure amends the Constitution to specify that proceeds and
interest from the fee are not subject to the Proposition 98
calculation, thereby precluding such a judicial determination.
- The measure inserts a new poison pill provision that renders the
Act inoperative if the Legislature does not appropriate moneys in
the Hospital Quality Assurance Revenue Fund within 30 days following
enactment of the annual budget act.
- The measure amends the provision triggered by a General Fund
cost from a lawsuit related to the Act. Specifically, the measure
redefines the threshold cost to be an overall net cost to the
General Fund due to the Act remaining operative, rather than 0.25
percent of General Fund expenditures authorized in the budget act.
Removal of Sunset Provisions. The measure
deletes the Act’s sunset provision. The measure also nullifies the
current-law sunset of the Hospital Quality Assurance Revenue Fund, and
instead specifies that the fund shall remain operative as long as the
Act remains operative. These combined changes permanently extend the fee
program under the Act—starting with the second program period—absent one
of the following conditions being met.
- An event occurs that triggers one of the Act’s poison pill
provisions (as amended by the measure).
- Additional statute that amends, repeals, or replaces the Act is
adopted and takes effect in accordance with the measure’s
Constitutional requirements.
Fiscal Effects
Significant Ongoing Fiscal Benefits to
State and Local Governments in Future Years
Continuation of Fee-Related Fiscal Benefits.
Under current law, the Act becomes inoperative on January 1,
2017. As a result, both the imposition of the fee and its related fiscal
effects are currently scheduled to end with the first program period. By
removing the Act’s sunset provision, the measure provides the authority
for implementation of the fee to continue without interruption through
subsequent program periods. Implementation of the fee across program
periods would be governed by the Act’s general structure for assessing
the fee and using the proceeds. Thus, following the first six months of
2016‑17, the measure would maintain ongoing significant fiscal benefits
to state and local governments that otherwise would cease to exist under
current law.
Specifically, barring conditions that would trigger the Act’s poison
pill provisions, the measure would permanently extend the following
fiscal benefits to the state and local governments.
- General Fund offset for children’s coverage. Under the Act’s
current provisions (continued by this measure), annual state savings
would be equal to 24 percent of the fee’s net benefit.
- Direct grants, capitation increases, and other quality assurance
payments that benefit counties, the UC system, health care
districts, and other units of government that own and operate public
hospitals.
Estimated Level and Growth of Fiscal Benefits.
For each year, the exact amount of fiscal benefits to state and
local governments would depend on the total amount of fee revenue
collected, the amount of quality assurance payments made to hospitals,
and the resulting calculation of net benefit. As these factors are
currently unknown and their estimation subject to some uncertainty, to
project the measure’s fiscal impact, we rely on assumptions about the
annual growth in federally allowable quality assurance payments to
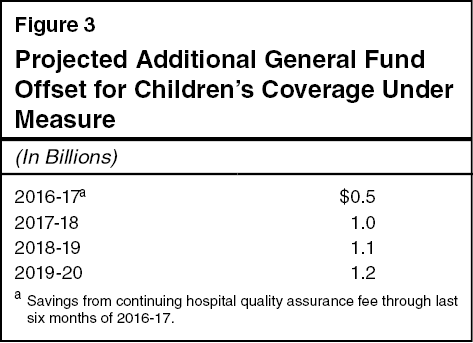
hospitals. Figure 3 (see next page) summarizes our multiyear projection
of the measure’s fiscal effect on the state General Fund by providing
fee revenues that offset state General Fund costs for children’s
coverage. We estimate that the General Fund offset for children’s
coverage would be around $500 million during the last six months of
2016‑17, reach more than $1 billion by 2019‑20, and grow between 5 to 10
percent annually thereafter. We also estimate that quality assurance
payments to state and local public hospitals would be around $90 million
during the last six months of 2016‑17, reach around $250 million by
2019‑20, and grow between 5 percent to 10 percent annually thereafter.
Below we discuss some considerations that affect our estimates.
Federal Sources of Uncertainty
We briefly highlight potential federal decisions that, if
implemented, could lead to significant deviations from our estimates of
the measure’s fiscal effects.
Allowable Rate of Provider Charges. Federal
regulations currently discourage states from levying provider charges
that exceed 6 percent of net patient revenue. Historically, hospital fee
programs in California have approached this threshold by assessing fees
as high as 5.5 percent of net patient revenue. We note that states have
previously litigated and successfully blocked regulations promulgated by
CMS that would have reduced the allowable rate of provider charges. If
the federal government were to successfully reduce permissible provider
charges—for example, to 3 percent rather than 6 percent of net patient
revenue—this could significantly lower estimated annual savings within
our multiyear projection. Such a change would also affect our estimate
of savings growth beyond 2019‑20.
Oversight of Quality Assurance Payments.
Federal cost containment strategies could also affect the amount of
quality assurance payments available under the fee. For example, changes
in federal Medicaid policy governing UPL calculations would affect
supplemental payments. As another example, CMS has expressed its
intention to tighten its oversight of capitation payment development in
Medicaid managed care and “look under the hood” of states’ actuarial
certification practices. Although it is difficult to quantify the
overall impact of these scenarios on quality assurance payments given
the varying forms such restrictions could take, they would generally
lead to lower net benefits to hospitals under the fee program, and thus
lower estimated savings to state and local governments from adopting the
measure.
Summary of Fiscal Effects
We estimate that the measure would result in the following major
fiscal impacts:
- State savings from increased revenues that offset state costs
for children’s health coverage of around $500 million beginning in
2016‑17 (half-year savings) to over $1 billion annually by 2019‑20,
likely growing between 5 percent to 10 percent annually thereafter.
- Increased revenues to support state and local public hospitals
of around $90 million beginning in 2016‑17 (half-year) to $250
million annually by 2019‑20, likely growing between 5 percent to 10
percent annually thereafter.
Return to Initiatives
Return to Legislative Analyst's Office Home Page