February 27, 2013
Overview of Health and Human Services Budget. The Governor’s budget proposes $20.3 billion from the General Fund for health programs—a 3.4 percent increase over 2012–13 estimated expenditures—and $8 billion from the General Fund for human services programs—a 7.9 percent increase over 2012–13 estimated expenditures. For the most part, the year–over–year budget changes reflect caseload changes, technical budget adjustments, and the implementation of previously enacted policy changes, as opposed to new policy proposals. On the health side, the budget reflects a net increase of $354 million from the General Fund for Medi–Cal, in part reflecting (1) increased enrollment among the currently eligible, but unenrolled, Medi–Cal population under the Patient Protection and Affordable Care Act (ACA) and (2) the shift of Healthy Families Program (HFP) enrollees to Medi–Cal that is currently underway. On the human services side, the budget reflects General Fund expenditure increases in all major programs, especially in the California Work Opportunity and Responsibility to Kids (CalWORKs) program—a $341 million, or 21.4 percent, increase that includes increased spending on employment services.
Fiscal Impact of Proposed Medi–Cal Expansion Not Reflected in Budget. While the Governor has proposed that the state adopt the optional Medi–Cal expansion under ACA, the budget does not reflect the fiscal effects from such expansion. Please see our February 2013 report, The 2013–14 Budget: Examining the State and County Roles in the Medi–Cal Expansion, for our analysis of the proposed expansion. The budget also does not reflect potential costs and savings related to other ACA provisions. These fiscal effects largely depend on pending policy decisions.
Medi–Cal—Uncertain Budgetary Savings. The Governor’s Medi–Cal budget proposal assumes General Fund savings from (1) prior–year budget actions that are currently being challenged in litigation or for which federal approval has not been obtained, (2) a new proposal to achieve managed care efficiencies, (3) the proposed reauthorization of the gross premium tax on managed care plans, and (4) the proposed extension of the hospital quality assurance fee. Accordingly, the level of savings assumed in the Governor’s proposal is subject to significant uncertainty and contingent on legislative action to reauthorize or extend taxes or fees.
HFP Transition to Medi–Cal Generally Proceeding as Planned, With Some Delays. We find that the administration has generally complied with various statutory requirements guiding the transition of HFP enrollees to Medi–Cal. The budget reflects erosion of the initially projected General Fund savings from the transition, in part due to implementation delays to address concerns about potential interruptions to continuity of care and other issues.
Developmental Centers (DCs) Need Improved Oversight. While several governmental and private entities perform oversight to ensure the health and safety of residents of the state’s DCs, there have continued to be allegations and findings of resident abuse and deficiencies in the management, training, and staffing of DCs. To strengthen oversight of the DCs, we recommend that the Legislature create an Office of the Inspector General (OIG), organizationally independent from the Department of Developmental Services (DDS), to oversee the DCs.
CalWORKs Budget Reflects Implementation of Recent Major Program Changes. Several recent changes to CalWORKs are being implemented currently or are scheduled to be implemented in 2013–14. These changes include the phase–out of exemptions from welfare–to–work (WTW) requirements and the introduction of a new 24–month limit on adult eligibility for CalWORKs benefits under state work participation rules that are more flexible than the federal rules that apply after 24 months. The budget reflects a number of strategies to help the state meet federally required work participation rates, and we think that the administration’s approach is a reasonable one. While we recommend that the Legislature augment CalWORKs employment services funding, we recommend that it determine the amount of such augmentation by considering the level of service it expects given its recent policy actions and the level of funding it deems appropriate in light of its priorities for the CalWORKs program.
In–Home Supportive Services (IHSS) Budget Proposal Has Risks. The Governor’s budget for IHSS assumes that the state will ultimately prevail in ongoing litigation regarding a 20 percent across–the–board reduction in IHSS service hours (triggered as a result of the 2011–12 budget package), allowing this budget savings solution to be implemented beginning on November 1, 2013. We think that the Governor’s budget assumption is subject to significant uncertainty. In light of the fiscal and policy concerns that we identify with respect to the 20 percent reduction, we recommend that the Legislature repeal the 20 percent reduction and instead continue a 3.6 percent across–the–board reduction that would otherwise sunset at the end of 2012–13. This action should have a better chance at achieving savings than the Governor’s proposal.
Background on Health Programs. Many of California’s major health programs are administered at the state level by several different departments. Some departments administer more than one health program. For example, the Department of Health Care Services (DHCS) administers Medi–Cal—California’s version of the federal Medicaid Program—as well as the California Children’s Services Program and other programs. The programs administered by state departments provide a variety of benefits to California’s citizens, including purchasing health care services for qualified low–income persons and performing various public health functions.
Most state health programs are administered at the state level by one of the following five departments: (1) DHCS, (2) Department of Public Health (DPH), (3) Managed Risk Medical Insurance Board (MRMIB), (4) DDS, and (5) Department of State Hospitals (DSH). The actual delivery of many health services often takes place at the local level and is carried out by local government entities, such as counties, and by private entities, such as commercial health plans. (Funding provided for these types of services delivered at the local level is known as “Local Assistance.”) However, there are significant exceptions to the local service delivery model. For example, DSH operates five state hospitals for the mentally ill and DDS operates four DCs that provide developmentally disabled individuals with 24–hour care. Both the state hospitals and the DCs are staffed with state employees who directly provide services to the residents of these state institutions.
Overview of Health Budget Proposal. The 2013–14 Governor’s Budget proposes $20.3 billion from the General Fund for health programs. This is an increase of $668 million—or about 3.4 percent—above the revised estimated 2012–13 spending level as shown in Figure 1. The net increase reflects increases in caseload and changes in utilization of services as well as the impact from major ongoing initiatives.
Figure 1
Major Health Programs and Departments—Budget Summary
General Fund (Dollars in Millions)
|
|
2011–12 Actual
|
2012–13 Estimated
|
2013–14 Proposed
|
Change From 2012–13
|
|
Amount
|
Percent
|
|
Medi–Cal—Local Assistance
|
$15,097
|
$14,897
|
$15,251
|
$354
|
2.4%
|
|
Department of Developmental Services
|
2,563
|
2,604
|
2,759
|
155
|
5.9
|
|
Department of State Hospitals
|
1,329
|
1,321
|
1,457
|
136
|
10.0
|
|
Healthy Families Program (HFP)—Local Assistancea
|
271
|
163
|
19
|
–144
|
–88.0
|
|
Department of Public Health
|
125
|
131
|
114
|
–17
|
–13.0
|
|
Department of Alcohol and Drug Programs (DADP)b
|
37
|
34
|
—
|
–34
|
—
|
|
Other Department of Health Care Services programs
|
59
|
136
|
130
|
–6
|
4.4
|
|
Emergency Medical Services Authority
|
7
|
7
|
7
|
—
|
—
|
|
All other health programs (including state support)
|
146
|
346
|
570
|
224
|
64.7
|
|
Totals
|
$19,634
|
$19,639
|
$20,307
|
$668
|
3.4%
|
Summary of Major Budget Proposals and Changes. As shown in Figure 1, the Governor’s proposed General Fund expenditures for 2013–14 reflect state–level organizational changes in the departments that will administer certain health programs. General Fund spending for HFP decreases from a revised estimate of $163 million in the current year to $19 million in the budget year, to account for the shift of HFP enrollees from HFP to Medi–Cal that is currently underway. There is a corresponding increase in the Medi–Cal budget to reflect this ongoing shift. Similarly, the General Fund spending for the Department of Alcohol and Drug Programs (DADP) decreases from a revised estimate of $34 million in 2012–13 to no expenditures in 2013–14 to reflect the department’s proposed elimination and transfer of all substance use disorder programs to DHCS. (The DADP’s Office of Problem Gambling would be transferred to DPH under the Governor’s plan.) We discuss the shift of HFP to DHCS and the proposed elimination of DADP in more detail later in this analysis.
The budget plan reflects the fiscal effects of recently adopted major policy initiatives, including the Coordinated Care Initiative (CCI) that was adopted as part of the 2012–13 budget package. Broadly, the CCI is intended to better coordinate the care of about 560,000 Medi–Cal beneficiaries who are also eligible for Medicare (known as dual eligibles) by shifting them from fee–for–service (FFS) to managed care beginning in 2013–14. The budget plan reflects both costs and savings associated with implementing the CCI. For information on CCI implementation, please see our report,
The 2013–14 Budget: Coordinated Care Initiative Update. The budget plan also reflects some, but not all, of the costs associated with the implementation of ACA also known as federal health care reform. For example, it includes a “placeholder” of $350 million General Fund for increased costs associated with additional enrollment among the currently eligible, but unenrolled Medi–Cal population as a result of changes to the eligibility determination process under ACA. However, the budget plan does not adjust for the fiscal impact to the state of the optional expansion of Medi–Cal eligibility that the Governor has committed to implement in January of 2014 and some other ACA implementation issues. For information on ACA implementation of the optional Medi–Cal expansion, please see our report,
The 2013–14 Budget: Examining the State and County Roles in Medi–Cal Expansion.
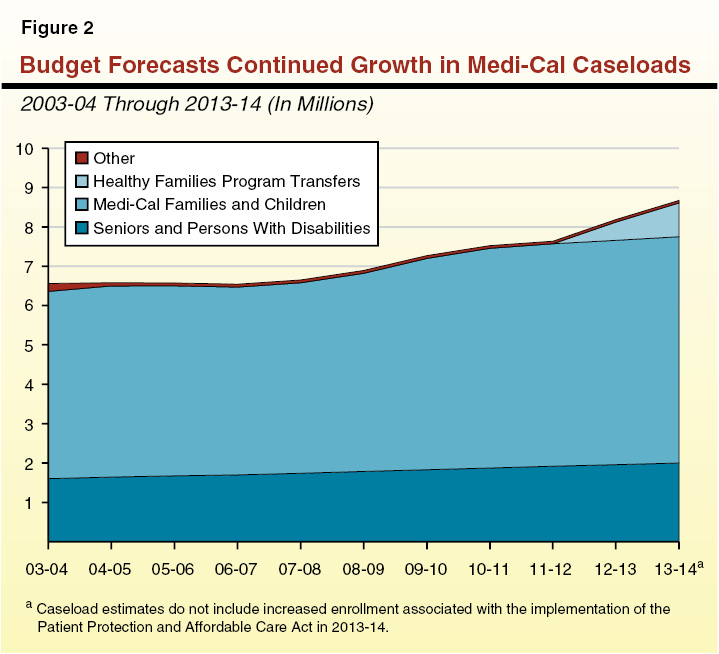
Caseload trends are one important factor influencing state health care expenditures. Below we highlight the caseload trends assumed in the Governor’s budget for Medi–Cal—by far the largest state–administered health program.
Medi–Cal Caseload. Figure 2 illustrates the budget’s projected caseload trends for Medi–Cal, divided into four groups: (1) families and children, (2) seniors and persons with disabilities (SPDs), (3) HFP transfers, and (4) others. The Governor’s budget plan assumes that the 2012–13 caseload for Medi–Cal will increase by about 153,000 compared to the number assumed in the 2012–13 Budget Act. The Governor’s budget plan also assumes a large increase in caseload will occur during 2013–14. Specifically, the overall caseload is expected to increase by about 486,000 average monthly eligibles (5.9 percent) to a total of about 8.7 million in 2013–14. This year–over–year increase can mainly be attributed to the HFP program transfers. The budget plan assumes that about 393,000 HFP enrollees will shift to Medi–Cal in 2013–14. This is in addition to the 465,000 HFP enrollees that the budget plan assumes will shift from HFP to Medi–Cal in 2012–13.
Background on Human Services Programs. California’s major human services programs provide a variety of benefits to its citizens. These include income maintenance for the aged, blind, or disabled; cash assistance and welfare–to–work services for low–income families with children; protecting children from abuse and neglect; providing home care workers who assist the aged and disabled in remaining in their own homes; collection of child support from noncustodial parents; and subsidized child care for low–income families.
Most social services are administered at the state level by DSS, the Department of Child Support Services, and the other Health and Human Services Agency (HHSA) departments. The actual delivery of many services takes place at the local level and is carried out by 58 separate county welfare departments. The major exception is Supplemental Security Income/State Supplementary Program (SSI/SSP), which is administered mainly by the U.S. Social Services Administration.
As a result of 2011 legislation, certain state program responsibilities and revenues in the human services area have been realigned to local governments (primarily counties). Specifically, beginning with the 2011–12 budget, the budget reflects shifts to counties of about $1.1 billion of General Fund costs in the CalWORKs program and about $1.6 billion in child welfare and adult protective services General Fund costs. As a result of these changes, the state’s role with respect to child welfare and adult protective services is largely one of oversight of county administration of these program areas.
Overview of Human Services Budget Proposal. The Governor’s budget proposes expenditures of $8 billion from the General Fund for human services programs in 2013–14. As shown in Figure 3, this reflects an increase of $585 million—or 7.9 percent—above revised General Fund expenditures in 2012–13.
Figure 3
Major Human Services Programs and Departments—Budget Summary
General Fund (Dollars in Millions)
|
|
2011–12 Actual
|
2012–13 Estimated
|
2013–14 Proposed
|
Change From
2012–13 to 2013–14
|
|
Amount
|
Percent
|
|
SSI/SSP
|
$2,721.6
|
$2,764.8
|
$2,817.4
|
$52.6
|
1.9%
|
|
CalWORKs
|
1,156.9
|
1,590.3a
|
1,930.8b
|
340.5
|
21.4
|
|
In–Home Supportive Services
|
1,725.9
|
1,723.2
|
1,808.2
|
85.0
|
4.9
|
|
County Administration and Automation
|
569.4
|
699.6
|
769.4
|
69.8
|
10.0
|
|
Department of Child Support Services
|
306.6
|
307.1
|
312.9
|
5.8
|
1.9
|
|
Department of Rehabilitation
|
54.5
|
55.3
|
56.6
|
1.3
|
2.4
|
|
Department of Aging
|
31.8
|
32.1
|
32.2
|
0.1
|
0.3
|
|
All other social services (including state support)
|
232.3
|
244.0
|
273.6
|
29.6
|
12.1
|
|
Totals
|
$6,799.0
|
$7,416.4
|
$8,001.1
|
$584.7
|
7.9%
|
Summary of Major Budget Proposals and Changes. As shown in Figure 3, the budget reflects a growth in General Fund expenditures across all major human services programs. The 21.4 percent increase ($341 million) in CalWORKs General Fund expenditures can largely be explained by two factors—a $143 million proposed augmentation for employment services (to some extent driven by policy reforms adopted in the 2012–13 budget package) and a $139 million year–over–year increase in the amount of federal Temporary Assistance for Needy Families (TANF) monies transferred to the California Student Aid Commission (CSAC). (The latter item increases the proposed CalWORKs General Fund expenditures by a like amount, but does not increase overall CalWORKs program expenditures.) We discuss both of these budget changes in further detail below.
The 10 percent increase ($70 million) in General Fund expenditures in the County Administration and Automation budget line item largely reflects a $44 million proposed augmentation for two welfare automation projects, also discussed further below.
Finally, the 4.9 percent net growth ($85 million) in IHSS General Fund expenditures reflects a multitude of budget adjustments—both on the cost and savings fronts—that do not signify new policy proposals of the Governor. For example, on the cost front, the budget includes General Fund increases in IHSS of (1) $59 million to restore funding due to the one–time nature in the 2012–13 enacted budget of a 3.6 percent across–the–board reduction in service hours and (2) about $49 million due to caseload growth. These and various other additional costs in IHSS are partially offset by the budget’s assumption that the 20 percent across–the–board reduction in service hours that was triggered by the 2011–12 budget package will begin to be implemented in November of 2013, generating partial–year savings of $113 million in 2013–14.
Varied Growth Through Recession. While caseload grew for most of the state’s human services programs during the recent recession, there was substantial variability in the growth rate across programs. (One key exception is the state’s foster care caseload, which has declined since 2001 and through the recession. In part, this reflects the creation of the Kinship Guardian Assistance Payment program in 2000 that facilitates a permanent placement option for relative foster children outside of the foster care system.) For example, over the 2007–08 to 2011–12 period, the CalFresh (formerly Food Stamps) and CalWORKs caseloads increased by a total of 97 percent and 27 percent, respectively, while the IHSS caseload—less susceptible to economic fluctuations—increased by a total of 8 percent. The SSI/SSP caseload grew modestly during this time period (a total of 3.4 percent)—in part reflecting recent grant reductions that in effect reduced the eligible population—and is projected to grow relatively modestly in 2013–14.
We now turn more specifically to caseload trends in the IHSS and CalWORKs programs and the budget’s assumptions regarding caseload for these two programs in 2013–14.
IHSS Caseload Projected to Decrease Modestly in 2013–14. The budget projects the average monthly caseload for IHSS to be 418,890 in 2013–14—a 1 percent decrease below the most recent estimate of the 2012–13 caseload. We discuss the administration’s projection in further detail below in the IHSS write–up in this report. For historical perspective, the IHSS caseload has remained relatively flat throughout most of the five–year period from 2009–10 to 2013–14, in part reflecting policy changes that constrained caseload growth.
Recent CalWORKs Caseload Decline Projected to Reverse During 2013–14. In the midst of the recent recession, the CalWORKs caseload rose substantially. The recent–year caseload peaked in June of 2011 at over 597,000 cases. Since that time, due to enacted policy changes and a slowly improving labor market, the caseload has been declining. The administration projects the average monthly caseload in 2012–13 to decline to 563,000 cases. In contrast, the average monthly caseload in 2013–14 is projected to increase by 1.5 percent to over 572,000, in part reflecting various policy changes in the enacted 2012–13 budget (discussed under the CalWORKs write–up elsewhere in this report) that should result in fewer case exits. In general, we find the administration’s caseload estimate for 2013–14 to be reasonable. In the long run, the caseload should continue to show a downward trend as the labor market continues to improve.
As part of his 2012–13 budget proposal, the Governor proposed shifting all enrollees in HFP—administered by MRMIB—to Medi–Cal—administered by DHCS—over a nine–month period beginning in October 2012. The administration stated that the proposal would have several benefits, including (1) generating General Fund savings, (2) improving continuity of care by reducing the number of children who transition between Medi–Cal and HFP on an ongoing basis, and (3) implementing some requirements of ACA early. (Under ACA, a portion of the HFP enrollees will become eligible for Medi–Cal on January 1, 2014.) (For more information on the Governor’s 2012–13 budget proposal for HFP, and extensive background information on HFP and Medi–Cal, please see our report,
The 2012–13 Budget: Analysis of the Governor’s Healthy Families Program Proposal.) In response, the Legislature enacted Chapter 28, Statutes of 2012 (AB 1494, Committee on Budget), to implement a modified version of the Governor’s proposal to shift all HFP enrollees into Medi–Cal (hereinafter referred to as the “transition”). Notably, the Legislature’s plan delayed the start of the transition to January 2013, included direction on how the transition is to be conducted, and provided for legislative oversight. This report provides a status update on the transition.
At the time this analysis was prepared, some children had shifted from HFP to Medi–Cal, while other children remained in HFP. Throughout this analysis, we will refer to all children who meet the eligibility requirements for the federal Children’s Health Insurance Program (CHIP) as the CHIP population, regardless of whether they are currently enrolled in HFP or Medi–Cal. We provide more information on CHIP in the background section of this analysis below.
Summary of Analysis. In this analysis, we begin by providing a brief overview of HFP. We then summarize key provisions of Chapter 28 including: (1) the timeframe for the transition, (2) reporting requirements to ensure network adequacy and continuity of care, and (3) requirements involving stakeholder involvement and written notices to HFP enrollees. We then describe the erosion of assumed General Fund savings in 2012–13 and 2013–14 due to delays in the implementation of the transition and other factors. We also analyze recent caseload trends and recommend that the administration be required to report at budget hearings on the causes of the recent decline in the CHIP population and its potential fiscal impact.
The HFP Is California’s CHIP. The CHIP provides health coverage to children in families that are low income, but with incomes too high to qualify for Medicaid. (In California, the federal Medicaid Program that provides health care services to qualified low–income persons is known as Medi–Cal.) Under the CHIP, for every dollar the state spends, the federal government provides roughly a two–dollar match.
As of December 31, 2012 (prior to the shift of some HFP enrollees to Medi–Cal, which began on January 1, 2013), HFP provided health insurance for 852,600 children up to age 19 in families with incomes above the thresholds needed to qualify for Medi–Cal, but below 250 percent of the federal poverty level (FPL). (The FPL is currently $22,050 in annual income for a family of four.) The MRMIB provides coverage by contracting with health plans that provide health, dental, and vision benefits to HFP enrollees. All HFP enrollees are enrolled in managed care plans. (Under managed care, health plans provide coverage and are reimbursed on a capitated basis. The health plans assume some financial risk, in that they may incur costs to deliver the necessary care that are more or less than the capitated rate. Most HFP plans are regulated by the Department of Managed Health Care (DMHC), which monitors financial solvency, evaluates provider network adequacy, conducts quality performance audits, and responds to beneficiary grievances.)
States Have Option to Combine Medicaid and CHIP Programs. A state may use federal CHIP funds to create a stand–alone program, such as HFP, or expand its Medicaid Program to include children in families with higher incomes. In both options, states receive the two–dollar federal match for every state dollar to provide coverage for the CHIP population.
Chapter 28 authorized the transition and divided it into four phases. Additionally, it contained several provisions to ensure legislative oversight, continuity of care, network adequacy, and stakeholder involvement. We describe these provisions in more detail here.
The Health Coverage Transition Will Take Place in Four Phases. When the 2012–13 Budget Act was enacted, the CHIP population was projected to be almost 880,000 by the time of the transition. This population was scheduled to be shifted to Medi–Cal managed care in four phases.
- Phase One. The first phase is authorized to begin no earlier than January 1, 2013 and includes children enrolled in HFP managed care plans that also contract with Medi–Cal. Generally, the children who are most likely to be able to stay with their current primary care provider will transition to Medi–Cal first. When the 2012–13 Budget Act was enacted, this phase was expected to include about 415,000 children.
- Phase Two. The second phase is authorized to begin no earlier than April 1, 2013 and includes children enrolled in HFP managed care plans that subcontract with a Medi–Cal managed care plan. When the 2012–13 Budget Act was enacted, this phase was expected to include about 249,000 children.
- Phase Three. The third phase is authorized to begin no earlier than August 1, 2013 and includes children enrolled in HFP managed care plans that do not contract with Medi–Cal or subcontract with a Medi–Cal plan. When the 2012–13 Budget Act was enacted, this phase was expected to include about 173,000 children.
- Phase Four. The fourth phase is authorized to begin no earlier than September 1, 2013 and includes children enrolled in HFP health care plans who live in a county where Medi–Cal managed care is not available. They will be transitioned into Medi–Cal FFS, unless a Medi–Cal managed care plan becomes available. (In Medi–Cal FFS, a health care provider receives a payment from DHCS for each medical service provided to a Medi–Cal beneficiary. Beneficiaries generally may obtain services from any provider who has agreed to accept Medi–Cal patients.) When the 2012–13 Budget Act was enacted, this phase was expected to include about 42,800 children.
Written approval from the federal Centers for Medicare and Medicaid Services (CMS) is required prior to implementing each phase of the transition. (As discussed below, CMS approval for phase one implementation was obtained prior to January 1, 2013.) After the transition is complete, the administration must apply for federal approval to administer the CHIP program as an integrated program with Medi–Cal. For more information on the how the federal government is monitoring the transition, see the nearby box.
As part of the federal approval process, the Department of Health Care Services has worked with Centers for Medicare and Medicaid Services to develop a framework for monitoring the transition. This monitoring will include collecting data on children who have transitioned from the Healthy Families Program to Medi–Cal. The monitoring framework has several objectives, including:
- Maintaining access to health care, dental care, behavioral and mental health services, and alcohol and substance use services.
- Providing continuity of care for children who are transitioning.
- Ensuring that the Children’s Health Insurance Program populations applying for Medi–Cal will be enrolled quickly and accurately into Medi–Cal.
Metrics will be collected on a monthly, quarterly, or annual basis to measure whether these objectives are achieved.
Dental Coverage Will Be Transitioned Concurrently With Health Coverage. Under Chapter 28, the HFP enrollees will transition their dental coverage at the same time that their medical coverage transitions. The transition will occur differently for those HFP enrollees located in Los Angeles and Sacramento counties and those HFP enrollees located elsewhere.
- HFP Enrollees Outside of Los Angeles and Sacramento Counties Shift to Denti–Cal. The HFP enrollees living outside of Los Angeles and Sacramento counties will receive dental care through Denti–Cal, Medi–Cal’s FFS dental program.
- HFP Enrollees in Los Angeles County Shift to Dental Managed Care andDenti–Cal. About 215,700 HFP enrollees live in Los Angeles County. If the enrollee is enrolled in an HFP dental plan that is also a Medi–Cal dental managed care plan, they will be enrolled in that plan. If their HFP dental plan is not a Medi–Cal dental managed care plan, they will be able to choose a new dental managed care plan or choose to be enrolled in Denti–Cal.
- HFP Enrollees in Sacramento County Shift to Dental Managed Care. About 27,500 HFP enrollees live in Sacramento County. If an HFP enrollee is enrolled in an HFP dental managed care plan that is also a Medi–Cal dental managed care plan, they will be enrolled in that plan. If their HFP dental plan is not a Medi–Cal dental managed care plan, they shall select a Medi–Cal dental managed care plan. If they do not choose a Medi–Cal dental managed care plan, they shall be assigned one which contracts with their current provider.
The Administration Is Required to Submit Several Reports to the Legislature. Under Chapter 28, several reports are required to be submitted to the Legislature throughout the implementation of the transition. These reports include:
- Strategic Transition Plan. The California HHSA is required to work with MRMIB, DMHC, DHCS, and stakeholders to develop a strategic plan for the transition and submit it to the Legislature by October 1, 2012. The intent of the strategic plan is to serve as an overall guide for the development of a plan for each phase of the transition and to ensure clarity and consistency in approach to enrollee continuity of care. The strategic plan is required to address several key transition issues, including: (1) administrative readiness at the state and local levels, (2) stakeholder engagement, (3) monitoring managed care health plan performance, (4) implementation timelines and key milestones, and (5) the transfer of the HFP Advisory Board to DHCS.
- Implementation Plans Are Required for Each Phase. Implementation plans are required 90 days prior to each phase of the transition. The plans are to be developed to ensure state and county system readiness, an adequate network of providers in each health plan, and continuity of care, with the goal of ensuring that there is no disruption of service and there is continued access to coverage for all transitioning enrollees.
- Network Adequacy Assessment Is Required. An assessment of network adequacy is required to be completed 60 days before the first shift of HFP enrollees to Medi–Cal.
- Monthly Status Reports Due Beginning February 15, 2013. Monthly status reports on the transition must be submitted to the Legislature beginning no later than February 15, 2013. These reports must include information relating to access to care, continuity of care, changes to provider networks, and eligibility performance standards. A final comprehensive report is due within 90 days of the conclusion of the transition.
Certain Performance Measures Must Be Integrated Into Medi–Cal Managed Care. Chapter 28 requires certain health plan performance measures be in place before children can be shifted from HFP to Medi–Cal. For example, Chapter 28 requires the integration of managed care performance measures with the HFP performance standards—which include the child–only Healthcare Effectiveness Data and Information Set.
Stakeholder Involvement and Written Notices to HFP Enrollees. Under Chapter 28, the DHCS is required to provide a process for ongoing stakeholder involvement and consultation and make information on the transition publicly available. The DHCS and MRMIB are required to work collaboratively to develop notices for HFP enrollees shifting to Medi–Cal. These written notices are required to be sent at least 60 days prior to the transition of individuals.
2012–13 HFP Budget Included an Unallocated Reduction. The 2012–13 Budget Act includes a $183 million unallocated General Fund reduction to HFP. A proposed extension of a tax imposed on managed care organizations (MCOs) used to offset General Fund costs would have provided an equivalent amount of money for the support of HFP in 2012–13, but it was not enacted into law. (For more information on the MCO tax, see the “Medi–Cal” section of this report.) The unallocated reduction of $183 million General Fund was revised downwards to $131 million in the Governor’s 2013–14 budget proposal due to changes in caseload and other factors.
2012–13 Shortfall in HFP Budget. On January 7, 2013, the Department of Finance (DOF) sent a letter to the Joint Legislative Budget Committee (JLBC) notifying the JLBC that MRMIB would expend all of its available resources for HFP in January 2013. To address this shortfall, MRMIB requested $15 million from Item 9840 of the 2012–13 Budget Act. (The Legislature appropriated $20 million General Fund in this item to be available to fund unanticipated expenses, subject to certain conditions specified in the 2012–13 Budget Act.) The DOF’s letter stated that MRMIB will seek legislation this year to cover the remainder of its shortfall in HFP as of January and the remainder of the fiscal year—estimated to total about $116 million. The Governor has proposed an MCO tax as part of the 2013–14 budget, and if such a tax were implemented, it could potentially offset the General Fund expense to fund the HFP shortfall in 2012–13. We note that failure to fund HFP would likely violate federal maintenance–of–effort (MOE) requirements, putting at risk billions of dollars in federal funding for CHIP and Medi–Cal.
When the 2012–13 Budget Act was enacted, it assumed General Fund savings of $13.1 million in 2012–13 as a result of the transition, and at that time the administration projected about a $58 million savings in 2013–14 and about $73 million in full–year General Fund savings annually thereafter. The administration has revised its estimates of the savings that will be achieved through implementation of the transition. Under the revised estimates, $129,000 in savings will be achieved in 2012–13, $43 million in 2013–14, and $38 million annually thereafter. These are the net result of several different adjustments, including changes in caseload, per member per month costs, and administrative costs.
We note that the administration’s revised estimate of the 2012–13 General Fund savings from the transition is based on a CHIP caseload of about 871,000 enrollees. However, as we describe in the next section of this analysis, the most recent caseload information suggests actual CHIP caseload will be lower than 871,000—by about 10,000 to 20,000 fewer enrollees. As a consequence, the estimates of the fiscal impacts of the transition will need to be further revised.
We find that the administration has generally complied with the requirements laid out in Chapter 28 as described above. The administration has submitted the required strategic plan, implementation plans, and network adequacy assessment reports. Written notices informing enrollees of the transition have been developed and sent to families. The DHCS has provided a process for ongoing stakeholder involvement and consultation and has made information, such as the required reports, publicly available.
The HFP transition is generally proceeding as planned, but with some delays. The DHCS worked with CMS to develop a framework for monitoring the transition and obtained federal approval of phase one of the transition on December 31, 2012. (Federal written approval is required prior to the implementation of each phase.) However, as we describe below, phase one was delayed for certain HFP enrollees due to concerns about network adequacy and continuity of care.
Prior to implementation of phase one of the transition, DHCS and DMHC completed network adequacy assessments and implementation plans for enrollees transitioning in phase one and phase two. During those assessments, potential interruptions to continuity of care for some transitioning HFP enrollees were identified.
- Particular Health Plan Had Low Provider Overlap Between HFP and Medi–Cal Networks, Raising Network Adequacy Issues. The first transition issue involved a particular health plan in phase one that had a low percentage of provider overlap between the HFP and the Medi–Cal networks and was unable to report how many primary care physicians would continue to see HFP enrollees after they shifted to Medi–Cal. To allow for an adequate network assessment, the transition of about 90,700 HFP enrollees enrolled in this plan was delayed. The DMHC and DHCS have indicated that HFP enrollees who are not able to remain with their current primary care provider under this plan may be given the choice to select a new plan or provider, rather than being reassigned automatically to this plan.
- Enrollees of a Particular Health Plan Shifted From Phase One to Phase Two Transition. The second transition issue involved a particular health plan that, while originally considered a “phase one” plan, was later recategorized as a “phase two” plan because it does not have a direct contractual relationship with Medi–Cal (instead, it subcontracts with a plan that contracts with Medi–Cal). Accordingly, about 14,600 HFP enrollees enrolled in this plan will transition to Medi–Cal at a later date than initially assumed.
- Some Enrollees Were Not Assigned Primary Care Physicians. The third transition issue involved HFP enrollees (mainly in rural areas with few doctors) who were not assigned to a primary care provider, although some of these HFP enrollees do have an ongoing relationship with a physician or other provider. If no primary care provider is assigned to an enrollee, claims data will be used to assign that enrollee to a provider that they have previously seen. The inability to identify a primary care provider for roughly 3,000 HFP enrollees enrolled in a particular plan in one county initially raised concerns about the administration’s ability to minimize disruptions to continuity of care. The administration has since determined that the network of Medi–Cal providers is adequate to receive transitioning HFP enrollees. The administration has determined that these enrollees can be transitioned on March 1, 2013, the second subphase of phase one.
Following the network adequacy assessments that we described above, the children who had been scheduled to transition in the first phase were further subdivided into three groups to reflect missing data from some plans and the concern that some HFP enrollees in phase one may not be able to remain with their primary care provider. Accordingly, the transition schedule was adjusted and the first two phases of the transition are now occurring as follows (CHIP caseload numbers have been updated since the 2012–13 Budget Act was enacted).
- Phase one, which includes approximately 402,000 children, has now been further broken up into three subphases, as follows:
- The first subphase began January 1, 2013. About 197,000 children in eight counties have transitioned to Medi–Cal.
- The second subphase will begin March 1, 2013. About 95,000 children in 15 counties will transition to Medi–Cal.
- The third subphase will begin April 1, 2013. About 110,000 children currently enrolled in a certain health plan in seven counties will transition to Medi–Cal.
- Phase two will begin on April 1, 2013 and include approximately 261,100 children that reside in 15 counties.
- There are no changes planned to phases three and four at this point. (Network adequacy assessments and implementation plans have not yet been completed for these later phases.)
Some Children Who Enrolled in HFP in November Will Transition in Later Phases. Some HFP enrollees who enrolled in HFP in November and December of 2012, and who would otherwise have been transitioned in phase one, enrolled too late to receive timely notices advising them of the transition. Staff at DHCS state that they do “look backs” to determine when sufficient time will have elapsed between notification and the transition to ensure that state and federal requirements regarding notification are met.
In June 2012, at the time the 2012–13 Budget Act was enacted, HFP had about 873,000 enrollees. As shown in Figure 4, the total number of enrollees has decreased steadily between May and December of 2012. By December 2012 (prior to the transition), HFP had 852,600 enrollees. It is not clear why caseload has declined. Monthly new enrollment in HFP since May 2012 has generally been below the monthly new enrollment seen in 2011.
Figure 4
Healthy Families Program Caseload Has Decreased Steadily in Recent Months
|
Total Number of
Enrollees in 2012
|
|
Change From
Prior Month
|
|
Month
|
Caseloada
|
Amount
|
Percent
|
|
May
|
874,890
|
|
966
|
0.1%
|
|
June
|
872,968
|
|
–1,922
|
–0.2
|
|
Julyb
|
868,709
|
|
–4,259
|
–0.5
|
|
August
|
863,033
|
|
–5,676
|
–0.7
|
|
September
|
859,909
|
|
–3,124
|
–0.4
|
|
Octoberb
|
858,500
|
|
–1,410
|
–0.2
|
|
November
|
857,090
|
|
–1,410
|
–0.2
|
|
December
|
852,592
|
|
–4,498
|
–0.5
|
Given the unanticipated decline in the CHIP caseload—which dropped from 874,900 in May 2012 to 852,600 in December of 2012—we recommend that DHCS and MRMIB report at budget hearings on the causes for the unanticipated decline in caseload. Additionally, we recommend that DHCS and DOF report at budget hearings on its updated projections of 2012–13 and 2013–14 General Fund savings and full–year General Fund savings beginning in 2014–15 from the transition, including a discussion of what is driving differences between these updated projections and what was assumed when the 2012–13 Budget Act was enacted.
As part of his 2012–13 budget plan, the Governor proposed to eliminate DADP by July 1, 2012 and shift its programs and administrative functions to other departments. The administration provided the following rationale for its proposal: (1) co–locating substance use disorder services with physical health programs administered by DHCS is a step toward integrating services to create a continuum of care and (2) the transfer of the programs to other state departments will better align a program’s mission with that of the department receiving the new program(s). The Legislature rejected the Governor’s proposal to eliminate DADP by July 1, 2012, delaying any potential elimination of DADP until July 1, 2013, in order to allow for additional stakeholder input and the development of a transition plan for shifting DADP programs and functions to other HHSA departments.
In this analysis, we provide a brief overview of DADP and then describe the Governor’s 2013–14 proposal for the elimination of DADP and the transfer of its programs and administrative functions to other departments (hereinafter referred to as the transition). We provide a description of the requirements imposed on the transition process by Chapter 36, Statutes of 2012 (SB 1014, Committee on Budget and Fiscal Review), and find that the administration has generally complied with these requirements. We recommend that DADP, DHCS, and DPH be required to report at budget hearings on various aspects of the transition of DADP programs and functions to other departments in order to ensure continued legislative oversight.
The DADP directs and coordinates the state’s efforts to prevent or minimize the effects of alcohol–related problems, narcotic addiction, drug abuse, and gambling. As the state’s alcohol and drug addiction authority, the department is responsible for ensuring the collaboration of other state departments, local public and private agencies, providers, advocacy groups, and program beneficiaries in maintaining and improving the statewide service delivery system. The DADP operates data systems to collect statewide data on drug treatment and prevention, and performs functions and administers programs in the following areas: (1) substance abuse and prevention services; (2) substance abuse treatment and recovery services; (3) licensing adult alcoholism, drug abuse recovery, and other treatment facilities; (4) drug courts and parolee services; and (5) problem gambling.
The Governor’s revised estimated total spending for DADP in 2012–13 is $322 million ($34 million General Fund). The Governor’s budget entirely eliminates funding for DADP in 2013–14 and shifts its functions, programs, and positions to other departments as follows.
- Various Programs Shift From DADP to DHCS. The budget shifts almost $314 million in all funds ($34 million General Fund) and 225.5 positions from DADP to DHCS to reflect the shift of the following programs and functions: (1) federal grants administration, (2) licensing activities, (3) Driving Under the Influence Program, (4) narcotic treatment programs, and (5) parolee services programs.
- Office of Problem Gambling Shifts From DADP to DPH. The budget shifts $3.7 million (all funds) and four positions from DADP to DPH to reflect the transfer of the Office of Problem Gambling from DADP to DPH. The DPH also requests $5 million in special funds expenditure authority and two, two–year limited–term positions to continue implementation and data collection of the Problem Gambling Treatment Services Pilot Program.
The budget assumes that the year–over–year net fiscal effect of the shift of DADP’s functions, programs, and positions as proposed by the Governor is neutral. Under the Governor’s proposal, costs resulting from the transition, such as the transfer of information technology (IT) systems and relocation of staff, will be absorbed within the existing resources of DADP, DHCS, and DPH.
Instead of adopting the Governor’s proposal in his 2012–13 budget to eliminate DADP by July 1, 2012, the Legislature enacted Chapter 36 to plan for implementation of the transition by July 1, 2013. However, the ultimate placement of DADP’s programmatic and administrative functions is contingent upon enactment of the 2013–14 Budget Act and implementing legislation. Chapter 36 requires HHSA—in consultation with stakeholders and affected departments—to develop a plan to be submitted as part of the Governor’s 2013–14 budget package. (The plan has been submitted by the administration.) The plan is intended to ensure that the transfer will achieve several goals, such as improving access to alcohol and drug treatment and ensuring appropriate state and county accountability through oversight and outcome measurement strategies.
Under Chapter 36, the transition plan prepared by HHSA shall include the following:
- Rationale. A detailed rationale for the transfer of administrative and programmatic functions from DADP to other departments.
- An Analysis of Transition Costs and Activities. A cost and benefit analysis for each transfer of a program or function from DADP to another department and for the proposal as a whole, showing fiscal and programmatic impacts of the changes.
- Continuity of Service Assessment. A detailed assessment of how the transfer of DADP functions and programs will affect continuity of service for providers, consumers, local government counterparts, and other major stakeholders.
- Coordination Across Departments. If the plan proposes to transfer functions from DADP to more than one department, then the plan should include details on how a smooth transition across departments will be ensured and how ongoing program and policy functions will be coordinated across departments.
- A Stakeholder Outreach Process. A detailed description of the process to include stakeholders in the development of the plan.
Overall, we find that the administration has acted in good faith to comply with the requirements set forth in Chapter 36 regarding stakeholder outreach and the submission of a transition plan. A total of three stakeholder workgroup meetings were convened in September and October of 2012 in order to obtain input from parties that would be affected by the elimination of DADP. In January 2013, HHSA submitted the transition plan to the Legislature as part of the Governor’s 2013–14 budget plan. We have reviewed the plan and find that it broadly meets the requirements set forth in Chapter 36.
In order to ensure continued legislative oversight over the elimination of DADP and the shift of its programs and functions to other HHSA departments, we recommend that DADP, DHCS, and DPH report at budget hearings on how the transition is proceeding. Specifically, the departments should report on how the transition will achieve the following goals set forth in Chapter 36 to:
- Improve access to alcohol and drug treatment services for consumers, including a focus on recovery and rehabilitative services.
- Effectively integrate the implementation and financing of services.
- Ensure appropriate state and county accountability through oversight and outcome measurement strategies.
- Provide focused, high–level leadership within state government for alcohol and drug treatment services.
In California, the federal Medicaid Program is administered by DHCS as the California Medical Assistance Program (Medi–Cal). As a joint federal–state program, federal funds are available to the state for the provision of health care services for low–income pregnant women, families with children, and for SPDs. California receives a 50 percent Federal Medical Assistance Percentage—meaning the federal government pays one–half of most Medi–Cal costs. Medi–Cal is by far the largest state–administered health services program in terms of annual caseload and expenditures.
There are two main Medi–Cal systems administered by DHCS for the delivery of medical services: FFS and managed care. In a FFS system, a health care provider receives an individual payment for each medical service delivered to a beneficiary. Beneficiaries generally may obtain services from any provider who has agreed to accept Medi–Cal payments. In managed care, DHCS contracts with managed care plans, also known as health maintenance organizations, to provide health care coverage for Medi–Cal beneficiaries. Managed care enrollees may obtain services from providers who accept payments from the health plan, also known as a plan’s “provider network.” The health plans are reimbursed on a “capitated” basis with a predetermined amount per person, per month regardless of the number of services an individual receives. Unlike FFS providers, the health plans assume financial risk, in that it may cost them more or less money than the capitated amount paid to them to deliver the necessary care.
The budget proposes $15.3 billion General Fund in 2013–14 for local assistance under the Medi–Cal Program, including the provision of health care services and county administration costs. This is a $354 million net increase, or 2.4 percent, over estimated 2012–13 expenditures. Generally, the level of expenditures and changes in year–over–year spending are driven by various factors, including:
- The total enrollment of beneficiaries in the program and per–person cost of providing health care services, which is affected by both the price and level of utilization for individual services.
- Policy changes that affect the level of spending for health care services, such as changes to the amount of payment to providers and managed care plans.
- Technical changes that result from the timing of receipt or payment of funds.
Later in this write–up, our analysis focuses on the fiscal impact on the Medi–Cal budget of prior and proposed policy changes, many of which are intended to create General Fund savings.
Caseload. The budget projects a monthly average of 5.8 million Medi–Cal beneficiaries will be enrolled in managed care during 2013–14 (67 percent of this total), while a monthly average of 2.9 million (33 percent) will be enrolled in FFS. Together, these projections—totaling 8.7 million beneficiaries—represent a 6 percent increase over the 2012–13 average total monthly caseload of 8.2 million beneficiaries. As mentioned in the “Overview” section of this report, most of the growth in caseload is due to the shift of HFP subscribers to Medi–Cal. (Please see our earlier write–up in the “Crosscutting Issues” section of this report for a detailed update on the HFP transition to Medi–Cal.)
We have reviewed the above baseline caseload projections—absent any changes associated with ACA, also known as federal health care reform—and do not recommend any adjustments at this time. If we receive additional information that causes us to change our assessment, we will provide the Legislature with an updated analysis at the time of the May Revision.
It is important to note that the budget’s caseload projections exclude two major populations expected to significantly increase enrollment in Medi–Cal under the ACA.
- Currently Eligible but Not Enrolled Population. Individuals who (1) are currently eligible but not enrolled in Medi–Cal and (2) take up Medi–Cal coverage due to provisions related to eligibility, enrollment, retention, and other changes under the ACA.
- Newly Eligible Population. Individuals who become newly eligible for Medi–Cal, if the state adopts the option under the ACA to expand coverage to low–income adults who are not currently eligible for Medi–Cal.
There is significant uncertainty about the magnitude of these ACA–related caseload changes. To a large degree, additional enrollment among the currently eligible depends on behavioral responses that are difficult to predict, such as responses to the individual mandate and simplified enrollment processes. In addition, major state policy decisions about how to implement the expansion, such as whether to adopt a state– or county–based expansion, would have very different effects on the state’s Medi–Cal caseload. When the administration provides updated Medi–Cal caseload estimates that incorporate these ACA–related changes, we will provide the Legislature with an updated assessment.
Special Session Will Address Medi–Cal–Related Issues. The Governor recently called for an extraordinary special session of the Legislature on health care to address ACA implementation issues, including conforming to federal eligibility and enrollment rules and other issues that may affect Medi–Cal take–up among individuals who are currently eligible but not enrolled. Later in this write–up, we discuss the budget’s $350 million General Fund placeholder for costs associated with this population.
Governor Proposes to Adopt Optional Expansion. The administration has stated its commitment to opting in to the optional expansion and the budget outlines a state– and county–based approach to expansion, but does not provide an estimate of the fiscal impact on the state for either approach. For a detailed analysis of fiscal and policy issues surrounding the optional expansion, please see our report, The 2013–14 Budget: Examining the State and County Roles in the Medi–Cal Expansion.
The CCI. The budget also proposes changes to the implementation plan for the CCI, a significant policy initiative that cuts across Medi–Cal, IHSS, and other health and human services program areas.
In the remainder of this write–up, we analyze and provide our assessment of (1) risks to savings assumed under prior budget actions, (2) new fiscal and policy proposals in the Medi–Cal budget, (3) fiscal effects associated with ACA implementation, and (4) the administration’s requests for additional resources.
The Medi–Cal budget includes some key assumptions about the ongoing General Fund savings associated with recently enacted budget actions. Below, we describe two assumptions and the level of associated General Fund risk assumed in the Governor’s Medi–Cal budget.
Provider Payment Reductions of Up to 10 Percent. In 2011, budget–related legislation authorized a reduction in certain Medi–Cal provider payments by up to 10 percent. Several months later, a U.S. District Court issued preliminary injunctions preventing DHCS from implementing most of the provider payment reductions. In December 2012, a Ninth Circuit Court of Appeals panel reversed the district court’s decisions and vacated the preliminary injunctions. However, on January 28, 2013, the plaintiffs petitioned the court for a rehearing and the state is currently prohibited from implementing the reductions.
The Medi–Cal budget assumes the injunctions will be lifted in March 2013 and the state can begin to implement the payment reductions for managed care in April 2013 and FFS in June 2013. It also assumes that, beginning September 2013, the state will begin to retroactively recoup a portion of payments made to FFS providers during the period in which the reductions were enjoined. The budget assumes $152 million General Fund savings in 2012–13 and $573 million in 2013–14 from implementing the provider payment reductions.
Analyst’s Assessment. Given the uncertainty regarding the timing and outcomes of legal proceedings, there is some risk that part or all of these savings will not be achieved as assumed in the Governor’s budget. We recommend that DHCS report at budget hearings on the status of the litigation so the Legislature can assess the likelihood of achieving these savings.
Medi–Cal Copayments. The 2011–12 budget authorized mandatory copayments for Medi–Cal beneficiaries on physician visits ($5), dental visits ($5), prescription drugs ($3 or $5), emergency room visits ($50), and hospital inpatient visits ($100 per day). The state was unable to obtain approval from the federal CMS to implement the mandatory copayments at the levels authorized in the 2011–12 budget. The 2012–13 budget assumed $20 million in General Fund savings from a revised proposal to implement lower copayment amounts for certain prescription drugs ($3.10 per filled prescription) and nonemergency use of emergency rooms ($15 per visit) for beneficiaries in managed care.
As part of the 2013–14 budget, the administration has revised its plan to implement copayments for Medi–Cal beneficiaries. The administration now proposes to implement only the $15 copayment for managed care enrollees who utilize the emergency room for nonemergency services. It is no longer proposing to implement copayments for certain prescription drugs. The budget assumes the copayment for nonemergency use of emergency rooms would be implemented in January 2013—saving $8 million General Fund in 2012–13 and $17 million General Fund in 2013–14.
Analyst’s Assessment. At the time of this analysis, we did not have any issues to raise with the administration’s revised copayment proposal for nonemergency care provided in the emergency room. However, we note that the revised copayment proposal has not been approved by the federal government. Since the budget assumed a January 2013 date of implementation, there is already some erosion to the 2012–13 savings assumed in the budget.
In addition, we note that recently proposed federal rules allow copayments of up to $8 for nonemergency use of emergency rooms for enrollees with income up to 150 percent of FPL. Since the $15 copayment is more than the $8 allowed under federal rules, the proposal requires federal approval of a waiver amendment rather than a state plan amendment (SPA). Generally, it is easier for the state to obtain federal approval for a SPA than for a waiver. The Legislature may want to consider directing DHCS to seek federal approval of a SPA for a nonemergency copayment of $8—an amount that would reduce General Fund savings, but that may have a greater likelihood of receiving federal approval—if it does not receive approval for the waiver amendment.
Governor’s Proposal. The administration indicates its desire to improve the quality and efficiency of the Medi–Cal delivery system. The proposed budget assumes savings of $135 million General Fund in 2013–14 by incorporating “efficiency adjustments” into managed care plan rates. At the time of this analysis, the administration had not provided detail about how these efficiency adjustments would be incorporated into managed care rates and how the estimated savings would be achieved. The administration indicates that these savings could be achieved under existing state law such that no statutory changes would be needed.
Analyst’s Assessment. Generally, we agree with the administration’s goal of structuring payments in a way that incentivize lower health care spending and improved health outcomes. However, at this time, the details of how the administration would achieve these outcomes are unclear. We recommend against the Legislature assuming the savings associated with this proposal, unless the administration can provide additional detail about this proposal, including:
- How it plans to incorporate efficiency adjustments into managed care plan rates.
- How the changes will reduce General Fund costs.
- How the changes would potentially impact the quality of care and access to care for Medi–Cal enrollees.
Governor’s Proposal. In recent years, the state’s gross premiums tax on insurers was expanded to include Medi–Cal managed care plans. A portion of the tax revenue from Medi–Cal managed care plans was matched with federal funds and used to increase the rates at which Medi–Cal managed care plans are reimbursed to offset the cost of the tax. The remaining revenue was used to offset state General Fund costs. The tax expired on June 30, 2012. The budget proposes permanently reauthorizing the gross premiums tax on Medi–Cal managed care plans, resulting in General Fund savings of $131 million in 2012–13 and $227 million in 2013–14.
Analyst’s Assessment. At the time this analysis was prepared, we did not have any issues to raise with the administration’s proposal to permanently reauthorize the gross premiums tax on Medi–Cal managed care plans. Generally, we support the concept of leveraging additional federal funding to offset state General Fund costs. If we receive additional information on this proposal that causes us to change our assessment, we will provide the Legislature with an updated analysis.
Background on the Hospital Quality Assurance Fee. The hospital quality assurance fee (hereinafter referred to as the fee) finances the state’s share of some increases to Medi–Cal payments to private hospitals. The state assesses the fee for each inpatient day at each private hospital. The fee varies depending on payer type, with the highest fees assessed on Medi–Cal inpatient days and lower fees assessed on days paid for by other payers, such as private insurance. Private hospitals pay the fee in quarterly installments, and the state uses most of the proceeds to draw down federal matching funds. The combination of fee revenue and federal matching funds allows the state to increase Medi–Cal FFS and managed care payments to private hospitals without incurring additional General Fund costs. Each quarter, the state also retains a portion of the fee revenue and uses it to offset General Fund costs for providing children’s health coverage, thereby achieving General Fund savings.
Governor’s Proposal. Under current law, the fee expires on December 31, 2013. The administration has proposed a three–year extension of the fee through December 31, 2016. The Medi–Cal budget assumes $310 million in savings during the last six months of 2013–14 from using the fee revenue to offset General Fund costs for children’s health care coverage. The administration has indicated that it will pursue extension of the fee through legislation that will be introduced in the policy committee rather than budget–related legislation. At the time of this analysis, draft legislation to implement the fee extension had not been provided by the administration.
Analyst’s Assessment. Because the administration has not introduced legislation to extend the fee at the time of this analysis, we were unable to assess the likelihood of whether the $310 million of General Fund savings assumed in the budget would be achieved under the administration’s proposal. The administration’s assumed savings are based on the amount of General Fund savings under the current fee arrangement during the first six months of 2013–14. These savings were achieved through a series of budget and policy actions.
- Under Chapter 286, Statutes of 2011 (SB 335, Hernandez), the fee’s authorizing statute, the state retained $97 million in quarterly fee revenue to offset General Fund costs for children’s health care coverage.
- Under the 2012–13 Budget Act, the Legislature adopted $117 million in savings from reductions (over six months) to fee–funded managed care payments and direct grants to public hospitals.
The administration has not identified whether the actions described above, or some other actions, would be adopted under the proposed fee extension to achieve $310 million in General Fund savings. We note that the assumed savings implies $155 million in quarterly General Fund savings from the new fee revenue—60 percent greater than the quarterly amount originally authorized under Chapter 286. When evaluating legislation to extend the fee, the Legislature will need to consider various policy issues, including:
- The schedule of fee rates for each inpatient day, by payer type.
- The process for using fee revenue to achieve General Fund savings and its varying impact on different categories of hospitals, such as public and private hospitals.
As the Legislature determines the appropriate amount of General Fund savings to adopt under an extended fee, it should weigh the total expected fee revenue and the net benefit to hospitals over the proposed extension period. For example, enrollment in Medi–Cal is expected to increase under the ACA. If more Medi–Cal beneficiaries receive inpatient care at private hospitals as a result, the amount of fee revenue available for both payments increases and General Fund savings may grow correspondingly.
Generally, we support the concept of leveraging provider fees in lieu of General Fund to increase Medi–Cal payments to providers without additional costs to the state. We recommend the Legislature enact an extension of the hospital quality assurance fee for this purpose. We also advise a limited–term fee extension, since this provides flexibility for the Legislature to restructure the fee in response to future changes that may occur in important areas, such as (1) Medi–Cal inpatient utilization and (2) federal requirements on states’ use of provider fees. However, since the administration has not submitted draft legislation at the time of this analysis, we were unable to comment on the details of administration’s proposal. The fee is a complex financing mechanism whose design has both fiscal and policy implications for the Medi–Cal Program. Therefore, we believe the policy committees are the appropriate venue for the Legislature to deliberate over important policy decisions related to the implementation of the fee—including the projected amount of fee revenue over a three–year extension and the portion of revenue used to fund hospital payment increases—before adopting the savings amount assumed in the Governor’s budget.
Governor’s Proposal. Currently, Medi–Cal managed care enrollees may change plans on a monthly basis. The budget proposes to allow certain Medi–Cal managed care beneficiaries to change health plans only during specified periods of the year. Certain populations would be exempt from this requirement, such as SPDs. New Medi–Cal enrollees would have an initial 90–day period during which they could change plans. Existing enrollees would be allowed to change plans during an annual 60–day “open enrollment” period. The administration estimates General Fund savings of $1 million in 2013–14 from implementing the open enrollment period.
Analyst’s Assessment. At the time this analysis was prepared, we did not have any issues to raise with the administration’s proposal. Open enrollment periods are a common requirement for individuals with private insurance coverage. If we receive additional information on these proposals that causes us to change our assessment, we will provide the Legislature with an updated analysis.
Governor’s Proposal. The Medi–Cal budget includes a $350 million General Fund placeholder for costs associated with increased enrollment of individuals who are currently eligible for Medi–Cal, but not enrolled in the program, until a more refined estimate can be developed. The ACA contains several provisions that will likely increase enrollment among individuals who are currently eligible for Medi–Cal, including simplified eligibility and enrollment procedures, enhanced outreach activities, and the individual mandate to obtain health coverage. The state will be responsible for 50 percent of the costs associated with the increased enrollment of individuals who are currently eligible.
Analyst’s Assessment. The short– and long–term costs from additional enrollment among the currently eligible Medi–Cal population under the ACA are subject to significant uncertainty. Some of the major areas of uncertainty include: (1) the size of the eligible, but not enrolled population, (2) the percent of the eligible population that will enroll (take–up rate), and (3) the cost of providing services to each additional enrollee. Figure 5 shows a range of estimated costs for these additional enrollees under three different scenarios. Under a moderate–cost scenario that we think is most likely, we estimate that the health care costs associated with this population would be $104 million in 2013–14—significantly less than the $350 million included in the Governor’s budget. Using different, but still plausible, assumptions, we estimate state costs could potentially be as low as $30 million or as high as $254 million in 2013–14. Therefore, even under a set of assumptions that would result in relatively high state costs, our near–term cost estimates are almost $100 million lower than the placeholder in the Governor’s budget. However, we estimate annual costs may be over $350 million within a few years—potentially ranging from the low hundreds of millions to nearly a billion dollars annually.
Figure 5
Range of Estimated Annual Medi–Cal Costs for Health Care Services to Currently Eligible but Unenrolled Population Under the ACAa
(In Millions)
|
State Fiscal Year
|
Low–Cost Assumptions
|
|
Moderate–Cost Assumptions
|
|
High–Cost Assumptions
|
|
Total Cost
|
Federal Fundsb
|
State Funds
|
Total Cost
|
Federal Fundsb
|
State Funds
|
Total Cost
|
Federal Fundsb
|
State Funds
|
|
2013–14
|
$65
|
$35
|
$30
|
|
$222
|
$118
|
$104
|
|
$540
|
$286
|
$254
|
|
2014–15
|
180
|
98
|
83
|
|
618
|
328
|
290
|
|
1,517
|
804
|
714
|
|
2015–16
|
222
|
120
|
102
|
|
765
|
407
|
359
|
|
1,897
|
1,005
|
893
|
|
2016–17
|
245
|
145
|
101
|
|
849
|
482
|
367
|
|
2,127
|
1,198
|
929
|
|
2017–18
|
259
|
157
|
103
|
|
901
|
522
|
379
|
|
2,279
|
1,309
|
970
|
|
2018–19
|
274
|
165
|
109
|
|
958
|
554
|
404
|
|
2,447
|
1,404
|
1,043
|
|
2019–20
|
289
|
174
|
115
|
|
1,015
|
587
|
429
|
|
2,620
|
1,501
|
1,119
|
|
2020–21
|
305
|
184
|
122
|
|
1,080
|
623
|
457
|
|
2,814
|
1,610
|
1,204
|
|
2021–22
|
323
|
194
|
129
|
|
1,150
|
663
|
487
|
|
3,027
|
1,731
|
1,297
|
|
2022–23
|
341
|
205
|
136
|
|
1,222
|
703
|
518
|
|
3,248
|
1,855
|
1,393
|
|
Key Assumptions
|
|
|
|
|
|
|
|
|
|
|
|
Eligible population in 2014
|
2.4 million
|
|
|
|
2.5 million
|
|
|
|
3.1 million
|
|
|
Average take–up ratesc
|
8%
|
|
|
|
20%
|
|
|
|
33%
|
|
|
Annual average cost per new enrollee in 2014
|
$1,169
|
|
|
|
$1,440
|
|
|
|
$1,694
|
|
Fiscal Estimates Are Incomplete. There are several potential costs and savings related to ACA implementation that are not included in the Governor’s budget. As discussed above, the budget does not assume any state savings or costs associated with the optional Medi–Cal expansion that the administration has stated it is committed to adopting. In addition, the budget does not assume savings from reduced enrollment in certain state health programs—such as the Family Planning, Access, Care, and Treatment Program and the Breast and Cervical Cancer Treatment Program—that may result from the additional health coverage options made available under the ACA, or administrative costs or savings associated with changes in the standards and processes used to determine Medi–Cal eligibility. To a large degree, these fiscal effects depend on important policy decisions that remain to be made. The Legislature will need to account for these and other ACA–related fiscal effects in the 2013–14 spending plan.
Key ACA Policy Decisions Remain. In addition to decisions about whether or not to adopt the optional expansion and whether to adopt a state– or county–based approach, the state has several other major ACA–related policy decisions that have yet to be made—many of which have potential fiscal effects in 2013–14. Some of the key decisions facing the Legislature include:
- Selecting the benefits that would be provided to the Medi–Cal expansion population if a state–based approach to the optional expansion were adopted.
- Determining how to implement the new Medi–Cal eligibility standards and enrollment processes as required by the ACA.
- Evaluating whether to modify or eliminate existing state health programs that provide services to persons who would become newly eligible for Medi–Cal or other health coverage in 2014.
- Whether or not to establish a Basic Health Program, a “Bridge Program” between Medi–Cal and the California Health Benefit Exchange (as proposed by the Governor), or some other program, with the intent to make coverage more affordable for populations with incomes too high to qualify for Medi–Cal.
These and other important ACA policy decisions may be informed by additional federal guidance that is expected in the coming months. As the Legislature considers these policy decisions, it will also need to consider any related fiscal effects as it constructs the state’s 2013–14 budget.
Governor’s Proposal. The Governor’s budget requests an increase of 333.5 positions for DHCS and $42.8 million ($4.3 million General Fund) in related state operations funding. The majority of the requested positions are related to the planned elimination of DADP and the related transfer of DADP programs to DHCS (238.5 positions and $28.7 million in state operations). (For more information on the elimination of DADP and the shift of its functions and programs to DHCS and the DPH, see our analysis on DADP in the “Crosscutting Issues” section of this report.) The remaining 95 positions are requested to support a variety of functions and programs administered by DHCS, including Medi–Cal waiver projects, CCI, the California Medicaid Management Information System replacement project, hospital financing, and other department workload activities. Of these 95 positions, the majority (76) are existing limited–term positions that the administration is requesting to extend on a limited–term basis.
Overall Analyst’s Assessment of Staffing Requests. We have reviewed the Governor’s requests for additional staffing for DHCS and, with the exception of one proposal described below, we find the Governor’s requests reasonable. If we receive additional information on the Governor’s proposals that causes us to change our assessment, we will provide the Legislature with an updated analysis.
Recommend Modification to Assisted Living Waiver Program Staffing Request. The budget requests $235,000 ($117,000 General Fund) and two positions—including a Health Program Manager (HPM) position—to continue workload related to the Assisted Living Waiver program and extend the program through February 2019. We find that there has been insufficient workload justification to support continuing the HPM position. Specifically, we find that the workload data provided by DHCS related to the HPM position appear overstated. We therefore recommend rejecting the request for the HPM position, resulting in $124,000 in savings ($62,000 General Fund).
Overview of DDS. Developmental disabilities include, but are not limited to, cerebral palsy, autism, epilepsy, and related conditions. The Lanterman Developmental Disabilities Services Act of 1969 forms the basis of the state’s commitment to provide developmentally disabled individuals with a variety of services, which are overseen by DDS. Unlike most other public social services or medical services programs, services are generally provided to the developmentally disabled without any requirements that recipients demonstrate that they or their families do not have the financial means to pay for the services themselves.
The Lanterman Act establishes the state’s responsibility for ensuring that persons with developmental disabilities, regardless of age, have access to services that sufficiently meet their needs and goals in the least restrictive setting. The department administers two main programs in implementing the Lanterman Act:
- Community Services Program. Community–based services are coordinated through 21 nonprofit organizations called regional centers (RCs), which provide diagnosis, assess eligibility, develop individual program plans for each consumer, and help consumers coordinate and access the services they need. The RCs purchase services from vendors for about 257,000 consumers in the current year. These services include day programs, transportation, residential care provided by community care facilities, and support services that assist individuals to live in the community. The RCs purchase more than 100 different services on behalf of consumers. As the payer of last resort, RCs generally only pay for services if an individual does not have private insurance or they cannot refer an individual to so–called “generic” services that are provided to the public at large at the local level by counties, cities, school districts, or other agencies.
- DC Program. The DDS operates four 24–hour facilities known as DCs—Fairview in Orange County, Lanterman in Los Angeles County, Porterville in Tulare County, and Sonoma in Sonoma County—and one smaller leased facility (Canyon Springs in Riverside County) which provide 24–hour care and supervision to approximately 1,600 residents in 2012–13. All of the facilities provide residential and day programs as well as health care and assistance with daily activities, training, education, and employment.
More than 99 percent of DDS consumers receive services under the Community Services Program and live with their parents or other relatives, in their own houses or apartments, or in group homes designed to meet their needs. Less than 1 percent live in DCs.
Overall Budget Proposal. The budget proposes $4.9 billion (all funds) for support of DDS programs in 2013–14, which is a 3.6 percent increase over estimated current–year expenditures. General Fund expenditures for 2013–14 are proposed at $2.8 billion, an increase of almost $156 million, or 6 percent, above the revised estimate of current–year expenditures. The increase in total expenditures largely reflects increases in caseload and utilization and the restoration of funding due to the sunset of a provider payment reduction.
Community Services Budget Proposal. The budget proposes $4.3 billion from all funds ($2.5 billion General Fund) for the support of the Community Services Program in 2013–14. This represents almost a $160 million General Fund increase, or 6 percent, over the revised estimate of the current–year spending. The increase is a net result of caseload growth and other program changes. Of the total $4.3 billion in funding proposed for RC programs in 2013–14, about $537 million is for RC operations and $3.5 billion is for the purchase of services. The 2013–14 Community Services program budget plan includes the following major proposals and other budget changes.
- Restoration of Funding Due to the Sunset of the Provider Payment Reduction. Increase of $46.7 million all funds ($31.9 million General Fund) to restore funding due to the sunset of the 1.25 percent provider payment reduction in RC operations and RC purchase of services. (The Legislature restored funding for 3 percentage points of the previous full 4.25 percent reduction in 2012–13.)
- Sunset of Proposition 10 Support. Increase of $40 million from the General Fund, reflecting the assumed sunset of $40 million in support from Proposition 10 monies (First Five Commission) that were used in lieu of General Fund in 2012–13.
- Caseload and Utilization. Increase of $177.5 million in all funds ($89.2 million General Fund) due to updated caseload information.
- Annual Family Program Fee. The budget continues the Annual Family Program Fee, which continues to offset General Fund costs by $7.2 million.
DCs Budget Proposal. The budget proposes $539 million from all fund sources ($279 million General Fund) for the support of DCs in 2013–14. This represents a net decrease of almost $4.6 million General Fund, 1.6 percent below the revised estimate of current–year expenditures. The DC budget plan includes the following proposals and other budget changes.
- Caseload and Utilization. Decrease of $25.4 million in all funds ($14.4 million General Fund) to reflect updated caseload information. This decrease is largely due to the anticipated shift of 223 residents from DCs into the community and the systemwide reduction of 352.5 positions. Lanterman DC makes up almost half of the residential decline as 110 community placements are anticipated in 2013–14.
- Sonoma DC Staffing. Increase of $2.4 million in all funds ($1.3 million General Fund) to support staffing needs at Sonoma DC in response to licensing actions, taken by DPH and certification actions taken by DPH on behalf of the federal CMS.
The DC budget also includes employee compensation augmentations due to adjustments in state employee retirement, health benefits rates, and employee compensation.
Headquarters Budget Proposal. The budget proposes $39.2 million from all funds ($24.9 million General Fund) for support of headquarters. Almost two–thirds of headquarters funding is for support of the Community Services Program with the remainder for support of the DC program.
The Governor’s budget reflects adjustments due to overall changes in caseload and utilization, the need for additional oversight in Sonoma DC, and the sunset of various General Fund savings measures implemented in previous fiscal years in the RC budget. While we find the caseload estimates to be reasonable, we recommend the department testify at hearings on its progress with finding community housing for Lanterman DC residents, as discussed below. Additionally, while we have no concerns with most of the proposed budget changes mentioned above, we are withholding recommendation on the request for additional Sonoma DC staffing. This is for reasons discussed in our analysis that follows on the need for improved oversight of DCs. In that analysis, we make a number of policy recommendations, including the recommendation that an independent OIG be created to oversee the DCs.
RC Caseload Has Steadily Grown in Recent Years. Between 2006–07 and 2012–13, the RC caseload grew from 212,225 to about 266,100—an average annual growth rate of 3.4 percent. The caseload trend is shown in Figure 6.
Figure 6
Regional Center Caseload Growth Trends
|
|
Average Annual Caseload
|
|
Increase From
Prior Year
|
|
Amount
|
Percent
|
|
2006–07
|
212,225
|
|
8,402
|
4.1%
|
|
2007–08
|
222,413
|
|
10,188
|
4.8
|
|
2008–09
|
231,451
|
|
9,038
|
4.1
|
|
2009–10
|
233,981
|
|
2,530
|
1.1
|
|
2010–11
|
242,977
|
|
8,996
|
3.8
|
|
2011–12
|
248,200
|
|
5,223
|
2.1
|
|
2012–13a
|
256,872
|
|
8,672
|
3.5
|
|
2013–14a
|
266,100
|
|
9,228
|
3.6
|
|
Averages
|
239,277
|
|
7,785
|
3.4%
|
Several key factors appear to be contributing to ongoing growth in the RC caseload. Medical professionals are identifying persons with a developmental disability at an early age and referring more persons to DDS programs. Improved medical care and technology has increased life expectancies for individuals with developmental disabilities. In addition, the increase in RC caseload reflects growth in California’s population.
Recent Data Suggest RC Caseload Estimate Is on Target. The Governor’s budget plan projects an RC caseload of 256,872 in 2012–13 and 266,100 in 2013–14—for a year–over–year increase of 9,228 consumers or about 3.6 percent. Based upon our review of recent RC caseload data, we find the administration’s caseload estimate to be reasonable and do not recommend any adjustments at this time.
DC Caseload Has Steadily Declined in Recent Years. Between 2001–02 and 2011–12, the DC population declined from 3,632 to 1,682—an average annual decrease of over 7 percent. This is consistent with federal and state policy to provide services to developmentally disabled individuals in the community rather than in an institutional setting. The decrease in the DC population between 2001–02 and 2011–12 reflects the closure of Agnews DC in 2009, the ongoing closure of Lanterman DC, and the corresponding shift of many consumers from DCs to community–based living arrangements.
Recent Data Suggest DC Caseload Estimate Is on Target. The Governor’s budget plan projects a DC caseload of 1,552 in 2012–13 and 1,304 in 2013–14—for a year–over–year decrease of 248 consumers or 16 percent. Based upon our review of recent DC caseload data, we find the administration’s caseload estimate to be reasonable and do not recommend any adjustments at this time. However, we note that the ability of the department to achieve its projected year–over–year decrease in DC caseload is based largely on the assumption that there will be sufficient community–based living arrangements that are appropriate to meet the needs of consumers shifting out of Lanterman DC and into the community. A lack of appropriate community–based living arrangements could slow the ongoing closure of Lanterman DC.
Analyst’s Recommendation. We recommend the department report at budget hearings on the availability of appropriate community–based placements for Lanterman DC residents. Specifically, the department should provide a timeline for when it will complete the development of sufficient community–based residences to shift the remaining Lanterman DC residents into the community.
Summary of Findings and Recommendations. The DPH licenses health facilities and certifies them on behalf of the federal CMS; facilities must be certified to receive federal Medicaid funding. In December of 2012, DPH announced it was taking significant action to protect Sonoma DC residents due to deficient practices at the DC that have harmed some residents. In January of 2013, DDS informed CMS that, due to ongoing deficiencies at Sonoma DC, it was withdrawing from federal certification four of Sonoma DCs ten Intermediate Care Facilities for the Developmentally Disabled (ICF–DD) living units. By voluntarily withdrawing four of the ten units, Sonoma DC will be able to maintain certification and receive federal funding for the remaining six.
In this analysis, we describe the existing entities that provide oversight of the DCs and a history of identified problems at the DCs regarding consumer health and safety. We provide a summary of the recent actions taken by DPH and summarize the fiscal implications of these actions to the state including the loss of federal funding. (A majority of DC residents are on Medi–Cal. Generally, for Medi–Cal enrollees living in DCs, the state bears roughly half the costs and the federal government bears the remainder.) We conclude by recommending the Legislature redirect funding from the department and use these funds to establish an independent OIG. We further recommend that the OIG have broad authority to exercise oversight over the DCs. Given the vulnerable nature of the population served by the DCs, the various civil rights legislation and related court decisions that apply to protect this population, and the ongoing nature of the health and safety problems that have plagued the DCs for more than a decade, we believe such additional oversight in the form of an OIG is warranted.
The DDS Performs Primary Oversight of DCs. The DDS has a general oversight role with DCs in that it hires all DC executive level staff, helps manage DC budgets, and creates rules and guidelines for how DC–related criminal investigations are to be handled. For example, the DDS set forth a new set of reporting guidelines to handle abuse allegations in 2002 and recently updated them in 2012.
Existing law establishes the Office of Protective Services (OPS) within DDS. Current statute gives peace officer status to those police officers in the DCs and authorizes them to enforce the rules and regulations of the DCs. The OPS officers are responsible for the investigation of thefts, trespassing, and suspicious person’s reports; responding to emergency calls; serving legal documents; and enforcing restraining orders on the grounds of the DCs. The OPS officers receive training at the same Peace Officers Standards and Training academies that municipal police and sheriff’s departments use.
Other Entities. Various other governmental and private entities perform DC oversight functions in order to ensure the health and safety of DC residents.
- The DPH. In order to operate as a healthcare facility, DCs must be licensed and certified by DPH. Being certified means the facility has met certain standards set forth by the federal government to participate in the Medicaid program and receive federal Medicaid funding. Separate units in the DCs are licensed and certified as Skilled Nursing Facilities (SNFs), ICF–DD, and General Acute Care hospitals.
- United States Department of Justice (USDOJ). Under the Civil Rights of Institutionalized Persons Act (CRIPA), USDOJ routinely conducts investigations in institutions that provide services for persons who are disabled or mentally ill.
- Disability Rights of California (DRC). The DRC—a nonprofit organization operating in the state—has traditionally taken the role of advocating on behalf of the developmentally disabled by ensuring their legal rights are protected. However, DRC also has federal authority to audit incidents at the DCs and has done so in the past.
- State Council on Developmental Disabilities (SCDD). The SCDD was established by state and federal law as an independent agency whose purpose is to ensure that people with developmental disabilities receive the services they need. The SCDD produces a report called the State Plan, in which it states its intent and goals to improve the access and services for disabled individuals. In its recent State Plan, SCDD set a goal to be more involved in the planning and closure process of DCs and to work with state and federal entities in order to protect the rights of residents of DCs.
The recent actions taken by DPH are the most recent in a series of actions that have been taken by various oversight entities over the past 15 years in response to findings of inadequate care, abuse, and neglect of DC consumers.
The DCs Sanctioned for Inadequate Care and Insufficient Staffing. In 1998–99, several DCs faced sanctions as a result of surveys by the then Department of Health Services and the federal Health Care Financing Administration. The surveys cited the DCs for numerous examples of inadequate care and understaffed residential and treatment units. In response, the state developed a four–year plan to increase staffing levels to help address federal concerns and to restore lost federal funding. In total, the four–year plan added approximately 1,700 positions at a cost of about $107 million ($55 million General Fund).
The OPS Subject of Press Allegations. In 2000, a series of news articles attributed unsolved cases at the DCs to lack of appropriate OPS investigative protocols. The articles reported that investigators were underqualified and inadequately trained. In response to the articles, the state Attorney General’s office was instructed by the Legislature to investigate. However, due to budget cuts, the AG’s office has cut back on the number of its investigators, leaving minimal oversight of the OPS.
The USDOJ Raises Concerns. In 2004, DDS was investigated by USDOJ under CRIPA. It first looked into the practices at Lanterman, and subsequently at Agnews and Sonoma DCs. The USDOJ identified civil rights violations at Lanterman and similar violations at Agnews and Sonoma DCs. For example, USDOJ found that Lanterman failed to protect its residents from neglect and physical harm—a problem compounded by Lanterman’s inadequate reporting and investigation system. As a result of the investigation, the U.S. Attorney General reported to the Governor its concerns that residents at Lanterman DC suffer harm and risk due to the facility’s inability to keep them safe and provide them with adequate behavioral and mental health and medical services. The report attributed this failure to the inability of OPS to conduct adequate incident reporting and investigative functions. The report cited that in a 13–month period, almost 50 percent, or 760 cases, of the incidents recorded were listed as having an unknown origin, indicating a lack of proper investigation into possible criminal and civil cases.
DRC Report Alleges Poor Investigative Practices. In 2005, DRC published a report that made claims of residents with lacerations in the Sonoma DC. The report was in response to five incidents that occurred over a five–year period at Sonoma DC. The report pointed out that investigations were hindered by delays in reporting the incidents and by the destruction of physical evidence. The DRC stated its concerns that OPS’ investigators did not have the qualifications and training necessary to investigate such sensitive cases.
California Watch Reports Suspicious Investigative Practices. In 2012, a series of reports by California Watch (an independent, nonprofit online investigative reporting center) reported suspicious investigative practices that were conducted in response to major crime investigations, including of suspicious deaths, at a number of DCs. The series brought into question the training and qualifications of OPS’ investigators and their ability to handle DC cases.
Future Intervention by USDOJ a Possibility. The DDS’ 2013–14 budget plan states the possibility of federal intervention from USDOJ for potential CRIPA investigations. Although USDOJ has not brought any legal actions against DDS to bring the DCs into compliance with CRIPA, it has done so in respect of other California state institutions. For example, several of the state’s mental hospitals recently operated under a CRIPA consent decree for several years. The 2012–13 budget plan included approximately $65 million related to the state mental hospital workload associated with this consent decree.
Report by California Bureau of State Audits (BSA) on OPS Is Pending. At the time this analysis was written, BSA was conducting an investigation into the investigative practices of OPS and training requirements for officers and management staff. The audit is expected to be released in May of 2013.
In December of 2012, DPH announced that it was taking action to protect the health and safety of residents at the Sonoma DC in response to finding the center is failing to correct problems, comply with state regulations, or satisfy federal standards set by the CMS. The DPH’s actions initiated the process to revoke federal approval for the services provided by Sonoma DCs ICF–DD and decertify it from participation in the federal Medicaid Program. (Broadly, an ICF–DD is a state–licensed nursing care facility that cares for developmentally disabled individuals who do not require the level of care provided at a hospital or SNF.
The Sonoma DC ICF–DD consists of ten occupied residential units that serve 290 residents. On January 18, 2013, DDS informed the CMS that due to ongoing deficiencies at the Sonoma DC ICF–DD, the department would voluntarily withdraw four residential units from federal certification in order to allow the DC to maintain certification and receive federal funding for the remaining residences. The four units that DDS is withdrawing from federal certification serve 112 residents. According to DDS, there are deficiencies in the management, training, and staffing in the Sonoma ICF–DD units generally. However, the problems are more significant in the units that are being withdrawn and addressing the problems in these four units will take additional time.
Decertification Has Fiscal Implications. The Governor’s budget plan does not take into account the potential for loss of federal funds due to decertification. The DPH has cited a number of patient care issues that potentially violate licensing and certification regulations. The department will lose approximately $1.4 million per month in federal funding for loss of certification of four ICF–DD living units. In order to continue to operate the four decertified units, the state will have to backfill the lost federal funding with General Fund monies.
The DDS Responds to Allegations. In 2012, the DDS made attempts to change the culture at Sonoma by removing both the Executive Director and the Clinical Director at Sonoma and implementing a nationwide search for a new Executive Director. Additionally, several staff members were terminated or disciplined and the OPS has hired an interim commander from the California Highway Patrol in order to help the department foster the skills necessary for an effective law enforcement agency. Finally, the department has hired an outside consultant who will monitor Sonoma and report to DDS any areas of concern. The budget requests two positions and $1.3 million General Fund for additional oversight of the units.
As we described above, several governmental and private entities perform oversight to ensure the health and safety of DC residents. However, over the past decade, there have continued to be allegations and findings of resident abuse and deficiencies in the management, training, and staffing of DCs. An option for the Legislature to consider that would strengthen oversight of the DCs is the establishment of an independent OIG that would have broad authority to oversee the DCs. We first describe the functions of an OIG. We then discuss why the particular circumstances in which DCs find themselves make an OIG a reasonable oversight option for the Legislature to consider.
General Functions of an OIG. An OIG safeguards the public’s interests by providing oversight and ongoing monitoring of a specified government agency or program. Its mission is typically to detect and deter waste, fraud, abuse, and misconduct, and to promote integrity, economy, efficiency, and effectiveness in an agency or program. This is usually accomplished by conducting independent investigations, audits, inspections, and special reviews of personnel and programs. To be effective, an OIG must have the authority and autonomy to initiate and complete investigations, audits, and reviews without interference from other entities. The state currently has an OIG that oversees the California Department of Corrections and Rehabilitation (CDCR). For more information on the CDCR OIG, see the nearby box.
The Office of Inspector General (OIG) for the California Department of Corrections and Rehabilitation (CDCR), which was created in statute, hires investigators with a variety of backgrounds. When the OIG for CDCR was first implemented in 2009–10, some of the positions had peace officer status, which is required to conduct certain types of investigations. The OIG for CDCR is subject to the same budgetary constraints as other state agencies, with funding for it appropriated by the Legislature through the annual budget process. The Inspector General for CDCR is appointed by the Governor and confirmed by the Senate, for a six–year term and may not be removed from office during that term except for good cause. The mission of the OIG is to safeguard the integrity of the state’s correctional system by inspecting, investigating, and auditing CDCR to uncover criminal conduct, administrative wrongdoing, poor management practices, waste, fraud, and other abuses by staff, supervisors, or management. The OIG provides analysis and policy recommendations to the Governor, Legislature, correctional administrators, and the public based upon its findings in these types of inquiries.
The OIG has generally proven effective in monitoring the operations of CDCR and has alerted the Legislature and the public to a number of issues and concerns with CDCR’s operations, including its treatment of inmates in state prisons. The state has been able to use OIG audits of inmate medical care to document the progress CDCR has made in complying with federal court orders. This documentation will likely help the state eventually regain control over inmate medical care.
What Is Unique About DCs to Warrant an OIG? Developmental Center consumers are a particularly vulnerable population subject to potential abuse due to their disabilities. An OIG for the DCs would help ensure the civil rights afforded this population—as enforced through various pieces of legislation, such as the Lanterman Act and the Americans with Disabilities Act, and related court decisions—are respected in the operation of the DCs. Additionally, an OIG presence would signal to the federal government the state’s concerns about keeping DC consumers protected.
Recommend Creation of OIG for the DCs. We recommend the Legislature adopt an additional layer of oversight and accountability over DCs by creating an OIG for the DCs. This would signal to CMS and USDOJ that the state is making a serious good–faith effort to solve the longstanding issues at the DCs and is not in need of additional federal oversight. Similar to the OIG over CDCR, this OIG would have authority to conduct a formal review of complaints, investigate possible wrongdoing against consumers, and work with local law enforcement to prosecute individuals. We recommend that the Inspector General for DCs be appointed by the Governor, subject to approval by the Senate, and both its director and staff should be organizationally independent from the department in order to maintain complete autonomy from DDS. The OIG would submit biannual reports to the Governor, the Legislature, and the public to convey its findings on the effectiveness of treatment for consumers, as well as a status report on abuse and the handling of abuse cases in the DCs. In summary, the mission of the OIG would be to safeguard the integrity of the state’s DC system.
Existing DDS Funds Could Be Redirected to Establish OIG. We estimate between $500,000 and $1 million would be needed to fund an OIG. We recommend that the new OIG be financed from funds redirected from the DDS’ existing budget. We note, in September 2012, the department had a 39 percent vacancy rate in OPS. The department could potentially redirect funding that is slated for some of those vacant positions with minimal impact to the current operations of the DCs. We recommend the Legislature require the department to report at budget hearings with a plan on where the funds could be redirected in a way that minimizes programmatic impacts. In particular, the department should report on whether funds could be redirected from either the DDS headquarters or the OPS budgets.
The DDS Could Be Underbudgeted in Current and Budget Years. We also recommend the Legislature, in its review and approval of the DDS budget, take into account that the DCs are possibly underbudgeted by as much as $8.4 million General Fund in 2012–13, and $16.8 million General Fund in 2013–14. This could be the case if DDS is unable to achieve substantial improvement in meeting federal certification requirements for Sonoma DC. The Legislature should require DDS to report at budget hearings on the corrective actions it is taking to address the issues identified by DPH and the timeline for completion of these corrective actions. Such actions should serve to reduce the potential for a continuing or expanded federal decertification and its attendant adverse fiscal impacts.
Withhold Recommendation on Sonoma DC Staffing Request. We withhold recommendation on the budget request for $2.4 million ($1.3 million General Fund) and authority to establish two positions to support staffing needs at Sonoma DC in 2013–14. At the time this analysis was written, we had not received documentation of the department’s comprehensive Performance Improvement Plan in light of the recent actions by DDS to withdraw four ICF–DD units from certification. We believe it is important to review the department’s request for additional resources as part of a comprehensive, written plan to achieve recertification and address the issues identified by DPH at Sonoma DC. Such a plan should include key objectives and a timeline for achieving those objectives.
Overview of DSH. The state’s five state hospitals—Atascadero, Coalinga, Metropolitan, Napa, and Patton—provide treatment to a combined patient population of over 5,500. Patients at the state hospitals fall into two broad categories: (1) forensic commitments, who have been committed by the courts as inmate transfers, mentally disordered offenders, not guilty by reason of insanity, incompetent to stand trial (IST), or sexually violent predators; and (2) civil commitments, who are generally referred to the state hospitals for treatment by the counties. Additionally, two psychiatric programs located on the grounds of state prisons at Vacaville and Salinas Valley have a combined inmate patient population of less than 700. In the last decade, state hospitals have seen a shift in their population—with the forensic population increasing steadily and the civil commitments in decline. The DSH reports the forensic population is now 92 percent of the statewide hospital system caseload.
Overall Budget Proposal. The Governor’s budget proposes $1.6 billion ($1.5 billion General Fund) for DSH in 2013–14, a net increase of $136.4 million General Fund from the revised 2012–13 expenditures for state hospitals. The major spending proposals include:
- Stockton Health Care Facility. The budget proposes an increase of $101 million General Fund for costs from the activation of the Stockton Healthcare Facility. This facility is not a state hospital, but a state prison that will have a designated area for treatment of mentally ill inmates who will be staffed by DSH personnel. Specifically, the budget requests $67.5 million General Fund and 540 positions for DSH to staff 514 beds scheduled for operation by July 2013. The budget also requests $33 million General Fund to recognize the full–year costs in 2013–14 of ramp–up activities that are taking place in 2012–13 (such as hiring and training staff) to ready the facility for operation.
- Personal Duress Alarms. The budget requests an increase of $16.6 million General Fund and four positions to support the continued installation of personal duress alarms in three of the state hospitals and to continue the installation process in the remaining two hospitals.
- IT Projects. The budget requests an increase of $6.5 million General Fund to implement two IT projects that would improve the efficiency of hospital management. The projects include: (1) $5.4 million and four positions for an automated staff scheduling and support tool that would allow DSH to centralize staffing data and (2) $1.1 million to consolidate eight existing independent hospital directories into one single directory.
Budget Requests Funding for Various Capital Outlay Projects. The budget requests an increase of $2.1 million General Fund in 2013–14 to update safety and security measures in the state hospitals. The projects include:
- Upgrade of Security Perimeter Fencing. The budget requests $560,000 to begin to update the fencing surrounding Patton State Hospital. The administration estimates that total additional expenditures of $14.5 million General Fund will be required in future years to complete the project.
- Courtyard Gates and Security Fencing. The budget requests $863,000 to begin improving security at Napa State Hospital by updating the gates surrounding the hospital. The administration estimates that total additional expenditures of $2.2 million General Fund will be required in future years to complete the project.
- Fire Alarm System Upgrade. The budget plan requests $633,000 to begin upgrading the fire alarm systems at Metropolitan State Hospital. The administration estimates that additional expenditures of $8.3 million General Fund will be required in future years to complete the project.
We note that by approving funding for the initial stages of the proposed capital outlay projects, the Legislature would create a General Fund pressure in future years to fund the costs of later phases of the projects, estimated at a total of $25 million General Fund.
The Governor’s budget reflects adjustments due to the startup of the Stockton Healthcare Facility, two new IT projects, and capital outlay projects for state hospitals. Overall, we find the requests to be reasonable. In particular, we find that the capital outlay requests and the request for personal duress alarms serve to improve hospital safety for patients and staff. The IT requests will improve the department’s management, such as by monitoring staff overtime.
Stockton Health Care Facility Proposal. The DSH is in the process of recruiting candidates to fill the 540 positions requested for 2013–14 to staff the Stockton Health Care Facility. The department is also planning for the voluntary transfer of some staff from both Vacaville and Salinas Valley psychiatric facilities to the new Stockton facility. We will be monitoring the recruitment and hiring process and will recommend budget adjustments at the time of the May Revision if progress towards filling the 540 positions is behind schedule.
Administration’s Caseload Projections and Trends. The Governor’s budget does not request an adjustment in either the current year or budget year from the caseload level assumed in the 2012–13 Budget Act. While this seems reasonable, we will continue to monitor caseload at the state hospitals and provide the Legislature with an updated recommendation at the time of the May Revision.
Over the next several years, the department predicts a steady increase in its population due to growing waitlists for treatment at a state hospital. Although caseload has risen for civil commitments in recent months, recently adopted statute requires counties to fully pay for civil commitments, resulting in annual savings of over $20 million for the department. A combination of key factors will affect future costs for the population served by DSH including: (1) the elimination of mental health beds at both Vacaville and Salinas Valley facilities, (2) the limited availability of licensed beds and restrictions on the use of some of those beds in state hospitals that prohibits DSH from filling them, and (3) the aging population of current patients in state hospitals, which will increase the cost of care in the future.
IST Commitments See Large Increase. Of note is the large increase in the IST population of over 150 individuals in 2012–13. By definition, those who are IST do not understand the criminal charges against them, and mental health professionals have determined that due to an individual’s insufficient mental ability, the individual is unable to help in his or her own defense. Therefore, the state commits felony charged IST individuals to a state hospital in order for competency to be restored. Traditionally, DSH has treated this population in the state hospitals. In 2007–08, the Legislature approved a pilot project allowing counties to provide treatment for ISTs in county jail, at a significantly lower cost to the state than competency treatment in a state hospital. In 2012–13, the Legislature authorized the DSH to continue this project.
Analyst’s Recommendation. Given the large recent increase in IST commitments in the state hospitals, the department should report at hearings on the progress in implementing the IST restoration treatment pilot program conducted at county jails. The department should report on the savings that have accrued to the state as a result of the program and make recommendations regarding whether the program should be expanded on a statewide basis.
Overview of DPH. The DPH administers and oversees a wide variety of programs with the goal of optimizing the health and well–being of Californians. The DPH is organized into several offices and centers, including the Center for Chronic Disease Prevention and Health Promotion, the Center for Infectious Diseases, the Center for Family Health, the Center for Environmental Health, and the Center for Health Care Quality. The department’s programs address a broad range of health issues, including maternal and child health, cancer and other chronic diseases, communicable disease control, environmental and drinking water quality, and inspection of health facilities. Many public health programs and services are delivered at the local level, while the state provides funding, oversight, and overall strategic leadership for improving public health. The state also directly administers certain public health programs, such as licensing and certification of health facilities.
Overall Budget Proposal. The budget proposes $3.4 billion (all funds) for support of DPH programs in 2013–14, which is a net decrease of $104 million, or 3 percent, below revised 2012–13 expenditures. General Fund expenditures for 2013–14 are proposed at $114 million, a net decrease of $16 million, or 12 percent, below the revised estimate of 2012–13 expenditures. For the budget as a whole, the Governor proposes $698 million for state operations and about $2.7 billion for local assistance.
The net General Fund decrease is mainly attributable to a $16.9 million reduction in General Fund support for the AIDS Drug Assistance Program (ADAP). This reduced General Fund spending level for ADAP reflects: (1) the shift of ADAP clients into the county–administered Low Income Health Programs (which provide health insurance to low–income adults), and (2) the anticipated shift of ADAP clients to other payers due to the implementation of ACA, also known as federal health care reform.
The Governor’s budget for DPH reflects technical budget adjustments due to changes in caseload and costs for some programs, such as ADAP and the Women Infants and Children Program. It also reflects the transfer of the Office of Problem Gambling from DADP to DPH. (For more information on this transfer, please see our analysis of the proposed elimination of DADP in the “Crosscutting Issues” section of this report.)
Nine Proposals Would Increase DPH’s Budget and/or Position Authority. The Governor’s budget includes nine proposals that would either increase DPH’s budget and position authority or continue existing budget and position authority that would otherwise expire at the end of 2012–13. (None of the budget proposals would change General Fund support for DPH in 2012–13 or 2013–14.) In total, these proposals increase DPH’s budget by $89 million (all funds), provide DPH with 24 new positions (11 positions proposed to be converted from contract positions to full–time, permanent positions), and extend 77 existing limited–term positions.
Analyst’s Overall Assessment. Overall, we find the Governor’s budget proposal generally to be reasonable. However, later in this analysis, we raise issues regarding three proposals that would increase DPH’s budget and/or position authority. We have analyzed the following six budget proposals and have not identified any issues. However, if we receive additional information that causes us to reassess our findings, we will apprise the Legislature. The six proposals are as follows:
- Convert 11 Division of Environmental and Occupational Disease Control (DEODC) Contract Positions. Convert 11 contract positions within the DEODC to full–time, permanent state positions to eliminate reliance on contracting for essential program services. Assumes savings of $48,000 (special funds).
- Increase Resources for the Export Document Program. Increase DPH’s budget by $287,000 (special funds) and authorize three additional permanent positions in the Center for Environmental Health’s Export Document Program in order to respond to requests for issuance of export documents within five working days of receipt of the request from California processors of foods, drugs, medical devices, and cosmetics.
- Increase Resources for the Stop Tobacco Access to Kids Enforcement (STAKE) Act. Increase DPH’s budget by $129,000 (special funds) and add one position to meet the expected increase in appeals for STAKE Act violations due to the implementation of Chapter 335, Statutes of 2012 (AB 1301, Hill).
- Maintain Resources for Public Health Emergency Preparedness Responsibilities. Increase DPH’s budget by $9.4 million (federal funds) and extend 76.8 limited–term positions for four years (to align with federal grant period) to support public health emergency preparedness activities.
- Transfer the Office of Problem Gambling to DPH. Increase expenditure authority by $3.7 million ($3.5 million special funds, $120,000 reimbursements) and shift four positions from DADP to DPH to reflect the transfer of the Office of Problem Gambling to DPH.
- Maintain Resources for the Problem Gambling Treatment Services Pilot Program. Increase expenditure authority by $5 million (special funds) and extend two, two–year limited–term positions in order to continue implementation and data collection for the Problem Gambling Treatment Services Pilot Program. (The program is currently administered by DADP.)
Below, we provide a summary of the three proposals that we take issue with, and give our findings and recommendations for each proposal.
Background. Recycled water is wastewater which has been treated and is suitable for various uses. Depending on the degree of treatment, recycled water may be suitable for many uses, including: domestic uses, such as tap water; agricultural uses, such as irrigation; recreational uses, such as swimming pools; or industrial uses, such as water used for cooling in manufacturing processes.
The Governor’s Proposal. The DPH requests three one–year limited–term positions and $700,000 in reimbursement authority to support an interagency agreement with the State Water Resources Control Board (SWRCB) to develop and adopt water recycling regulations as required by Chapter 700, Statutes of 2010 (SB 918, Pavley). Chapter 700 requires DPH to take several actions including:
- Adopting uniform water recycling criteria for the use of recycled water to replenish or augment a groundwater basin or aquifer that is designated as a public water supply (this water is then treated before being delivered to consumers) on or before December 31, 2013.
- Convening and administering an expert panel to advise DPH on the development of uniform water recycling criteria for (1) the use of recycled water to replenish a surface water reservoir that serves as a public water supply and (2) the feasibility of developing uniform water recycling criteria for the introduction of recycled water directly into the public water supply or into the untreated water supply immediately upstream of a water treatment plant (hereinafter referred to as “direct use of recycled water”).
- Developing uniform water recycling criteria for surface water augmentation to be submitted to an expert panel. If the panel finds that the criteria adequately protect public health, the department is required to adopt the criteria on or before December 31, 2016.
- Providing a report to the Legislature by December 31, 2016, on the feasibility of developing uniform water recycling criteria for the direct use of recycled water.
- Providing a written report submitted to the Legislature as part of the annual budget process each year from 2011 through 2016. The report shall provide information on the department’s progress towards developing and adopting uniform water recycling criteria for surface water augmentation and its investigation of the feasibility of developing water–recycling criteria for the direct use of recycled water. This report will be developed in consultation with SWRCB.
Chapter 700 authorized funds from the Waste Discharge Permit Fund (administered by SWRCB) to be made available to DPH and authorizes DPH to accept funds from any source (upon appropriation by the Legislature). The SWRCB has stated that $1.4 million from the Waste Discharge Permit Fund is available starting July 1, 2012 to begin implementation of Chapter 700, of which $700,000 was appropriated in the 2012–13 Budget Act.
Currently, DPH is in the process of finalizing an interagency agreement with SWRCB to complete the regulations on the use of recycled water for groundwater recharge. The DPH released draft regulations in November 2011 and is preparing responses to the comments received on those draft regulations. The DPH anticipates releasing revised draft regulations in spring of 2013.
The DPH Reports It Has Insufficient Resources to Fully Implement Chapter 700. The DPH has stated that as a result of “a lack of funding for this work and competing statutorily required priorities for limited staff,” no progress has been made towards developing and adopting uniform water recycling criteria for surface water augmentation or investigating the feasibility of the direct use of recycled water. Accordingly, no progress reports have been submitted to the Legislature. (If additional funding is identified that could be used for Chapter 700 implementation, DPH has stated that it will request additional appropriation authority.)
Analyst’s Recommendation. We do not take issue with the Governor’s request for three limited– term positions and $700,000 in reimbursement authority because we find that they are justified on a workload basis to meet the requirements of Chapter 700. However, we recommend that the Legislature require DPH to report at budget hearings on which competing statutory priorities are delaying implementation of Chapter 700. This information will allow the Legislature to assess whether DPH’s prioritization of workload reflects the Legislature’s priorities. We also recommend the Legislature require DPH to report at budget hearings on the additional resources that would be necessary to fully meet the statutory requirements of Chapter 700.
Background. In 2002, the voters approved Proposition 50—the Water Security, Clean Drinking Water, Coastal and Beach Protection Act of 2002—a $3.4 billion water bond measure. Proposition 50 provided $485 million to DPH to address water quality issues, through the provision of grants to local water projects that address water security, reduce reliance on the Colorado River, provide source water protection, provide treatment for disinfection byproducts, study demonstration treatments, and monitor water quality. To date, the DPH has executed 52 funding agreements for Proposition 50 projects, which have totaled $189 million.
The Governor’s Proposal. The Governor’s budget requests $22 million from Proposition 50 bond funds for local assistance in 2013–14. The administration is proposing budget bill language to revert, effective June 30, 2013, all unspent Proposition 50 funds from prior appropriations through 2009–10. The administration is also requesting provisional budget bill language that would allow DOF to increase the Proposition 50 expenditure authority above $22 million to an amount equal to projects which DPH can fund by June 30, 2014, if the funds are expended for a purpose that is consistent with Proposition 50 and the $22 million appropriation has already been fully encumbered. (Based on the projects currently being reviewed for approval, DPH expects that more than $22 million in local assistance will be needed to fund projects in 2013–14.)
The provisional budget bill language also states that if DOF determines that DPH has demonstrated that it can fund additional Proposition 50 projects (above the amount appropriated), “the department shall so report to the Legislature.”
Analyst’s Recommendation. We recommend that DPH report at budget hearings on the progress of implementing Proposition 50 to date. We have no issue to raise with the provisional budget bill language that would revert unspent funds. We do recommend that the Legislature reject the administration’s proposed provisional budget bill language that would allow DOF to increase expenditure authority above $22 million. The administration should request the level of funding it believes necessary to fund shovel–ready projects in 2013–14. Historically, this is how funding to implement Proposition 50 has been appropriated.
Background. In 2006, the voters approved Proposition 84—the Safe Drinking Water, Water Quality and Supply, Flood Control, River and Coastal Protection Act of 2006—a $5.4 billion water bond measure. Proposition 84 provided $300 million to DPH to address drinking water quality by providing funding for grants to local water projects that address contaminated drinking water. The DPH has spent and encumbered approximately $173 million of the $300 million available, leaving $127 million to be appropriated. The DPH is expecting to have all the funds encumbered by June 30, 2015. (The previous appropriation for Proposition 84 projects was previously approved for a five–year time period.)
Governor’s Proposal. The Governor’s budget requests $48 million from Proposition 84 bond funds for local assistance in 2013–14. The DPH expects to be able to expend more than the $48 million requested in 2013–14 and is proposing provisional budget bill language that would (1) allow the amount appropriated to be available for expenditure until June 30, 2016, and (2) authorize DOF to increase the appropriation equal to the amount of projects that DPH can fund by June 30, 2014, if the funds are expended for a purpose consistent with Proposition 84 and if all the funds appropriated have been fully encumbered.
The proposed provisional budget bill language also states that if DOF determines that DPH has demonstrated that it can fund additional Proposition 84 projects, “the department shall so report to the Legislature.”
Analyst’s Recommendation. We recommend that DPH report at budget hearings on the progress of implementing Proposition 84 to date. We further recommend the Legislature reject the administration’s proposed provisional budget bill language. The administration should request the level of funding it believes necessary to fund shovel–ready projects in 2013–14. Historically, this is how funding to implement Proposition 84 has been appropriated.
The CalWORKs program was created in 1997 in response to the 1996 federal welfare reform legislation, which created the federal TANF program. CalWORKs provides cash grants and WTW services for families whose income is inadequate to meet their basic needs. Grant amounts vary across the state and are adjusted for family size, income, and other factors. As an example, a family of three in a high–cost county that has no earned income receives a monthly grant of $638 per month (approximately 40 percent of federal poverty guidelines). A family in these circumstances would generally also be eligible for food assistance through the CalFresh program (formerly known as Food Stamps) in the amount of $520 and health coverage through Medi–Cal. As a condition of receiving aid, CalWORKs families that include able–bodied adults are required to participate in work activities and are entitled to receive supportive services, including subsidized child care and job development assistance.
CalWORKs is funded through a combination of California’s TANF block grant allocation ($3.7 billion annually), the state General Fund, and county funds. The state is required to provide minimum MOE level of funding from the General Fund and county funds for assistance to families eligible for CalWORKs in order to receive the TANF block grant. In recent years, the MOE has been $2.9 billion. While CalWORKs makes up the majority of TANF and MOE spending, it is important to note that the TANF block grant is used to fund a variety of programs in addition to CalWORKs, and some General Fund expenditures outside CalWORKs are counted toward the MOE requirement.
As shown in Figure 7, the CalWORKs program received $5.2 billion in total funding in the 2012–13 budget. The Governor’s 2013–14 budget departs from proposals of recent years and reflects modest expenditure growth in CalWORKs, with total funding up 4 percent to $5.4 billion. General Fund spending in CalWORKs is proposed to increase by $340 million over revised 2012–13 estimates. The Governor’s budget reflects (1) the continuing implementation of various policy changes enacted in prior years that have both positive and negative impacts on program spending; (2) a $943 million funding swap with the CSAC (a $139 million increase over a similar funding swap in 2012–13), which has no net impact on General Fund spending in the state budget overall; and (3) a $143 million augmentation to CalWORKs employment services.
Figure 7
CalWORKs Budget Summary
All Funds (Dollars in Millions)
|
|
2011–12 Appropriated
|
2012–13 Appropriated
|
2013–14 Proposed
|
Change From 2012–13
|
|
Amounta
|
Percent
|
|
Cash grants
|
$3,278
|
$3,158
|
$3,176
|
$19
|
1%
|
|
Employment services
|
946
|
914
|
1,085
|
170
|
19
|
|
Stage 1 child care
|
435
|
416
|
417
|
—b
|
—b
|
|
Administration
|
631
|
576
|
574
|
–2
|
—b
|
|
Other
|
97
|
157
|
159
|
3
|
2
|
|
Totals
|
$5,387
|
$5,221
|
$5,411
|
$190
|
4%
|
Recent Caseload Decline Projected to Reverse During the Budget Year. The CalWORKs caseload rose substantially during the recent recession, peaking in June 2011 at over 597,000 cases. Since that time, the caseload has been declining due to enacted policy changes and a slowly improving labor market. The average monthly caseload in 2012–13 is projected to be 563,000 cases. In contrast, the average monthly caseload in 2013–14 is projected to increase by 1.5 percent to over 572,000. Several factors are expected to contribute to this projected growth, including the scheduled increase in the amount of earned income that is exempted when calculating a family’s monthly grant (known as the “earned–income disregard”), annual income reporting for child–only cases, and semiannual income reporting for the remainder of the CalWORKs caseload. Each of these policies results in fewer case exits and should increase the caseload in 2013–14. In general, we find the administration’s caseload estimate to be reasonable. In the long run, we expect the caseload to return to a downward trend as the labor market and earning prospects for the CalWORKs families continue to improve.
Governor’s Budget Reflects Minor Erosion of Recent CalWORKs Savings. The 2012–13 enacted budget assumed $470 million in General Fund savings from the CalWORKs program, with $423 million in savings in 2013–14. These savings are driven largely by the temporary extension and creation of new work exemptions that result in decreased employment services and child care funding requirements. Updated information indicates that actual savings in 2012–13 are likely to be $24 million lower than planned due to unforeseen challenges with implementing annual reporting for child–only CalWORKs cases. Specifically, federal guidance clarified that it may be necessary to use an administratively more costly set of reporting rules, known as “change reporting,” for CalFresh benefits provided to CalWORKs child–only cases.
The Governor’s budget assumes that savings in 2013–14 from 2012–13 budgetary actions will be approximately $120 million less than assumed when the 2012–13 Budget Act was enacted. This further erosion is primarily the result of action the Legislature took subsequent to the enactment of the 2012–13 Budget Act to restore $80 million in reduced funding for CalWORKs administration and services that was previously assumed in the budget using unspent prior–year TANF funds. This augmentation was intended to address unmet county needs associated with providing WTW services to CalWORKs recipients who are exempt from participation but choose to volunteer. The use of unspent TANF funds allowed for the augmentation to have no General Fund impact in 2012–13. However, to continue funding employment services at the same level, the Governor’s budget reflects an increase in General Fund to replace the one–time TANF funds.
The following sections will (1) discuss the state’s progress in implementing recent CalWORKs program changes, (2) review the status of the state’s TANF work participation rate and the impact that the TANF–CSAC funding swap and other policies are expected to have on the rate, and (3) evaluate the Governor’s employment services augmentation proposal.
Several changes to the CalWORKs program enacted in recent years are being implemented currently or are scheduled to be implemented in 2013–14. The following section briefly describes some of the more significant changes, their current status, and the fiscal impact of the changes assumed in the Governor’s budget.
Phase–Out of Short–Term Young Child Exemptions. Beginning in 2009–10 and continuing through 2011–12, the Legislature achieved budgetary savings by broadening the circumstances under which counties could exempt CalWORKs recipients from participating in WTW activities. Savings were achieved by not providing WTW services to the exempted population. The 2012–13 budget extended the exemptions an additional six months. As of January 1, 2013, the exemptions are discontinued and formerly exempt adults that do not qualify for an additional exemption (an estimated 15,000 cases) will be required to resume or begin participation in WTW activities. The process of reaching out to formerly exempt households to bring them back into WTW participation, informally known as “reengagement,” is required by statute to take place gradually over 24 months and conclude by the end of 2014. As formerly exempt populations reengage in WTW activities, additional funding will be needed to provide the services required by law. Costs for reengagement are estimated at $13 million (General Fund) in 2012–13. The Governor’s budget proposes an additional $98 million (General Fund) to perform the bulk of reengagement efforts during 2013–14. These amounts appear reasonable and are consistent with our understanding of the pace and cost of reengagement.
WTW 24–Month Time Clock. The 2012–13 budget package also made two fundamental, ongoing changes to the CalWORKs program. First, the state rules that govern work participation for cases with able–bodied adults (known as work–eligible cases) were altered to provide a more flexible set of approved activities and lower required hours. Second, a new 24–month limit on adult eligibility for CalWORKs benefits under state work participation rules (known as the WTW 24–month time clock) was introduced. Once 24 months of participation under state work participation rules are exhausted, adult participants are required to comply with federal work participation rules, which are less flexible than the state rules and place a heavier emphasis on employment, as opposed to education, training, or barrier–removal activities (such as mental health or substance abuse treatment). Work–eligible cases that fail to meet the applicable work participation rules (state or federal) at any time will have their monthly grant reduced by the adult portion (generally about $120). Months under the 24–month clock need not be consecutive, meaning that cases that meet federal requirements in a given month will not have that month counted against their 24–month limit. Additionally, counties may allow up to 20 percent of their cases that have passed the 24–month limit to continue to participate under state rules.
Under current law, the WTW 24–month time clock is operative as of January 2013. While all work–eligible cases are potentially subject to the clock, the number of cases moving toward the 24–month limit in any given month will be lower. This is because some cases, including those that are compliant with federal work rules, exempt from work participation, or sanctioned, will not have a month counted against their 24–month limit. Full implementation of the WTW 24–month time clock should eventually result in General Fund savings from decreased grants to cases with adults that fail to meet federal work requirements after their 24 months are exhausted, beginning in January 2015 (24 months after the time limit first took effect). Accordingly, the Governor’s 2013–14 budget assumes no direct costs or savings from the time limit’s implementation. However, the administration has proposed that an additional $143 million (General Fund) be spent to increase the level of employment services provided to WTW participants, in order to help a greater number of work–eligible cases find sustainable employment prior to the 24–month limit. This proposal is discussed separately later in this analysis.
Earned–Income Disregard Restoration. The earned–income disregard, which lessens the grant reduction that a CalWORKs household experiences when its earned income grows, was reduced in the 2011–12 budget. The 2012–13 budget restored the earned–income disregard to its former higher level, effective October 1, 2013. The immediate impacts of this restoration are that (1) CalWORKs households with earned income will receive higher grants and (2) the amount of income at which a CalWORKs household would exit the caseload has increased, resulting in fewer case closures. The Governor’s budget estimates that the CalWORKs caseload will increase by approximately 4,300 cases in the 2013–14 fiscal year due to this change, with a corresponding cost of $38.5 million (General Fund).
Semiannual Reporting. Chapter 501, Statutes of 2011 (AB 6, Fuentes), requires that the state transition from quarterly to semiannual income reporting for CalWORKs and CalFresh recipients beginning in April 2013, with full implementation no later than October 1, 2013. Due to unforeseen challenges in obtaining federal waivers to implement this change, it is anticipated that counties will meet the October 1 deadline but will not implement semiannual reporting in advance of that date as originally planned. The administration now estimates that implementation of the change will entail $10.7 million ($4.4 million General Fund) in up–front automation costs in 2012–13. The Governor’s budget assumes a net cost of approximately $500,000 ($400,000 General Fund) to fully implement the change in 2013–14, reflecting a partial year of administrative savings and one–time training costs.
Work Incentive Nutritional Supplement (WINS) Program. The WINS program was originally authorized in the 2008–09 budget, but implementation has been subsequently delayed to January 1, 2014. The program will provide a $10 additional food benefit to CalFresh recipients that meet federal TANF work requirements but are not in the CalWORKs caseload. A primary purpose of this program is to increase the state’s TANF work participation rate (discussed below). The DSS estimates that approximately 215,000 CalFresh households will initially qualify and that approximately 140,000 of these will continue to participate during 2013–14. These households will generally be required to submit work verification on a semiannual basis as a condition of receiving the additional benefit. This represents a minor added reporting burden over what would be required for participation in CalFresh alone, and could discourage some eligible households from participating. However, we find the administration’s participation estimates reasonable. The Governor’s budget includes $10.4 million (General Fund) in 2013–14 for WINS automation, administration, and benefits.
While the state is free to establish its own work participation rules, federal law requires that the state report the percentage of work–eligible TANF cases that participate in federally approved work activities for the required number of hours. This percentage is known as WPR. A state’s WPR must be at least 50 percent for all work–eligible TANF households (referred to as the “all–families WPR”) and at least 90 percent for work–eligible two–parent TANF households in order to avoid federal financial penalties. In general, penalties for WPR noncompliance start at up to a 5 percent reduction of the state’s TANF block grant (translating to about a $187 million reduction in California) and grow by 2 percentage points each following year, up to a maximum of 21 percent. Under federal regulations, any reductions in the TANF block grant that come as a result of a penalty must be backfilled with state expenditures.
The state’s WPR requirements may be reduced through a “caseload reduction credit,” which is obtained when the caseload declines below its federal fiscal year (FFY) 2004–05 level. The state may earn additional caseload reduction credit when it spends its own resources on MOE–qualifying expenditures above the MOE requirement, also known as “excess MOE.” Since the creation of CalWORKs, the state has had a large caseload reduction credit and consequently has had a low adjusted WPR requirement. However, changes in federal rules altered the calculation of caseload reductions such that the state’s credit was substantially reduced in FFY 2006–07. Any remaining caseload reduction credit would have been lost as caseloads grew during the recent recession; however, Congress granted an exception that temporarily allowed the state to continue to receive the level of its FFY 2007–08 credit through FFY 2010–11.
State’s WPR Shortfall to Continue. Figure 8 shows the state’s all–families and two–parent WPR requirements, available caseload reduction credits, and the state’s adjusted WPR requirements, for FFYs 2006–07 through 2011–12. The figure also shows the state’s WPR performance for FFYs 2006–07 through 2008–09—the most recent three years for which the federal government has officially verified the state’s WPR. Partly as a result of changes to federal law and the effects of the recession, California has been out of compliance with the overall WPR requirement since FFY 2006–07 for years with available official data. With the FFY 2007–08 caseload reduction credit in place, California’s all–families WPR fell just short of the adjusted requirement in FFYs 2007–08 and 2008–09. The all–families WPR may have increased or decreased in FFYs 2009–10 and 2010–11, but official results have not been published by the federal government. The state has benefitted from a 90 percent caseload reduction credit for two–parent families (resulting in a 0 percent adjusted requirement) and maintained official compliance with the two–parent requirement through FFY 2008–09. Compliance with the two–parent requirement is assumed in FFYs 2009–10 and 2010–11. However, as the temporary extension of the FFY 2007–08 all–families and two–parent caseload reduction credits ended with FFY 2010–11, the state’s caseload reduction credits will likely be zero beginning in FFY 2011–12. This would result in the state’s noncompliance with both the all–families and two–parent requirements beginning in FFY 2011–12.
Figure 8
TANF Work Participation Rate (WPR) Requirement Status
Federal Fiscal Year (FFY)
|
|
2006–07
|
2007–08
|
2008–09
|
Estimated
|
|
2009–10
|
2010–11
|
2011–12
|
|
All–Families Required Rate
|
50.0%
|
50.0%
|
50.0%
|
50.0%
|
50.0%
|
50.0%
|
|
Caseload reduction credita
|
17.7
|
21.0
|
21.0
|
21.0
|
21.0
|
—
|
|
Adjusted Requirement
|
(32.3%)
|
(29.0%)
|
(29.0%)
|
(29.0%)
|
(29.0%)
|
(50.0%)
|
|
Actual participation rate
|
22.3%
|
25.1%
|
26.8%
|
—b
|
—b
|
—b
|
|
Shortfall(–)/Surplus
|
–10.0%
|
–3.9%
|
–2.2%
|
|
|
|
|
Two–Parent Required Rate
|
90.0%
|
90.0%
|
90.0%
|
90.0%
|
90.0%
|
90.0%
|
|
Caseload reduction credita
|
90.0
|
90.0
|
90.0
|
90.0
|
90.0
|
—
|
|
Adjusted Requirement
|
(—)
|
(—)
|
(—)
|
(—)
|
(—)
|
(90.0%)
|
|
Actual participation rate
|
31.7%
|
26.5%
|
28.6%
|
—b
|
—b
|
—b
|
|
Shortfall(–)/Surplus
|
31.7%
|
26.5%
|
28.6%
|
|
|
|
Penalties Have Been Assessed . . . The state has been notified by the federal government that penalties of $47 million and $113 million were assessed for FFYs 2007–08 and 2008–09, respectively, for failure to meet the all–families WPR. Penalties for FFY 2009–10 and beyond are unknown, but possible, given that the poor condition of the labor market, increasing caseload levels, and the state’s eventual lack of caseload reduction credit negatively impact its ability to meet the WPR requirements. However, federal law provides the circumstances under which penalties can be reduced or eliminated completely. First, if a state is compliant with the overall (all–families) WPR requirement but not the two–parent requirement, the penalty amount is lowered to reflect only the proportion of the two–parent families in the total caseload. This could be significant for California because two–parent cases make up a relatively small portion of the CalWORKs caseload. States may also claim reasonable cause in situations where the noncompliance can be shown to be the result of a natural disaster or other calamity. A finding of reasonable cause would result in the penalty being waived. If reasonable cause cannot be demonstrated, states generally may enter into corrective compliance plans, which can delay or eliminate penalties as the state demonstrates progress toward compliance.
. . . But Not Enforced. The DSS has submitted documentation claiming reasonable cause relating to penalties already assessed, but to date has not been advised by the federal government as to whether reasonable cause will be granted. As a result, the state’s TANF block grant has not yet been reduced and it is unknown whether a corrective compliance plan will be needed. The extended lack of guidance from federal officials makes it unclear whether the penalties already assessed will be enforced, or whether the state will face additional penalties in the future.
Recent and Proposed Actions Designed to Have Positive Impact on State’s WPR. Despite the uncertainty surrounding the enforcement of WPR–related federal penalties, significant risk to the General Fund remains. Accordingly, the state is currently in the process of taking action to increase the WPR and mitigate the potential for enforced penalties in the future. These actions are made possible in part through the TANF–CSAC funding swap. The history and implications of the this funding swap are described in the nearby box. The major WPR–related actions are as follows:
- Creation of Excess MOE. The Governor’s budget—if enacted as proposed—would result in an estimated $475 million in General Fund spending counted toward the MOE above the amount required to receive the TANF block grant. Federal law allows for excess MOE to create additional caseload reduction credit, which lowers the state’s WPR requirement, and thus the risk of federal penalties from noncompliance. However, as additional caseload reduction credit will not be available to the state until the CalWORKs caseload declines to FFY 2004–05 levels, the WPR–related benefit of creating excess MOE will not likely come into play until several years down the road.
- Solely State–Funded Program. Federal law requires that all work–eligible cases whose benefits are funded with TANF funds or state MOE dollars be included in the state’s WPR calculation. (The CalWORKs caseload includes some cases that are not subject to WTW participation under state law but are considered work–eligible under federal law and are therefore included in the WPR. Most notably, this includes “safety net” cases in which only children are aided because adult members have reached their maximum 48–month time limit on aid.) However, cases that are funded solely with state resources that are not counted toward the MOE may be excluded from the WPR calculation. Funding cases with non–MOE state resources constitutes what is known as a “solely state–funded” program. The Governor’s CalWORKs budget includes $372 million of what the administration has designated as non–MOE General Fund spending to provide grants to approximately 70,000 safety net and other cases that are not meeting federal work requirements. The solely state–funded program is expected to be implemented sometime in early 2013. The program is estimated to increase the state’s all–families WPR by an estimated 6 percentage points when fully implemented in FFY 2013–14. The impact on the FFY 2012–13 WPR will be less due to a partial year of operation. The estimated impact on the two–parent WPR is unknown.
- WINS Program. The statutorily created WINS program will provide an MOE–funded benefit to households not already in the CalWORKs caseload that are meeting federal work requirements. By bringing these compliant households into the calculation of the state’s WPR, the state’s WPR will increase. Specifically, the WINS program could improve the all–families WPR by 15 percentage to 20 percentage points when fully implemented in FFY 2014–15. The impact on the FFY 2013–14 rate will be less due a partial year of operation. The impact on the two–parent WPR is unknown.
Swap Has No Net Impact on CalWORKs Funding Levels or Overall General Fund Spending. The 2012–13 enacted budget redirected $804 million in Temporary Assistance for Needy Families (TANF) block grant funds from the California Work Opportunity and Responsibility to Kids (CalWORKs) program to the California Student Aid Commission (CSAC) to be used for expenditures in the Cal Grants program that are allowable under federal rules that govern the use of TANF funds. Reduced TANF funds in CalWORKs were replaced dollar for dollar with General Fund monies from CSAC, resulting in no net impact on funding levels for Cal Grants and CalWORKs or General Fund spending overall.
Swap Results in General Fund Spending in CalWORKs Above MOE Requirement. General Fund funding in CalWORKs was subsequently reduced in the 2012–13 enacted budget by $470 million. Absent the funding swap, this would have brought the state below its required maintenance–of–effort (MOE) funding level and jeopardized the federal TANF block grant. However, because the size of the funding swap substantially exceeded the General Fund reductions in CalWORKs, the CalWORKs program was left with General Fund spending above the MOE requirement.
Governor Proposes to Increase Swap. Under the Governor’s budget, the TANF–CSAC funding swap would increase to a total of $943 million in 2013–14, with no associated reductions in CalWORKs or Cal Grants. This increase reflects the full funding of all expenditures in Cal Grants eligible to be funded with the TANF block grant. The amount of eligible expenditures in Cal Grants is expected to increase in 2013–14 and the swap is proposed to be increased accordingly. As before, the swap would have no net impact on total funding in either program or on General Fund spending overall. The larger swap would, however, result in additional General Fund spending in CalWORKs above the MOE, accounting for more than one–third of the proposed $340 million increase in General Fund spending in CalWORKs over 2012–13 levels.
Spending Above MOE Has Important Implications. Having higher General Fund expenditures in CalWORKs than is required by the MOE provides potential benefits to the state. First, should the state choose to do so, General Fund and county spending above the MOE could be counted as excess MOE to obtain an additional reduction in the required work participation rate (WPR), thereby lowering the risk of federal penalties. Second, General Fund and county spending above the MOE could, at the state’s choosing, not be counted towards the MOE requirement. This opens the door to CalWORKs spending on purposes that are not allowed under TANF rules but that benefit the state. For example, the state can fund CalWORKs benefits for individuals that it wishes to exclude from the state’s WPR in a so–called “solely state–funded program,” as discussed in more detail in the body of the CalWORKs analysis. Finally, should the need arise in the future, the state has greater flexibility to enact policy changes—including those that would reduce General Fund spending in the CalWORKs program—without coming up against the constraint of the MOE requirement.
California May Be Partially Compliant by FFY 2014–15. Given available data and based on reasonable assumptions, we project that the combined effect of the policies described above could be to increase California’s all–families WPR to above the 50 percent requirement beginning in FFY 2014–15. This estimate is subject to significant uncertainty, however, particularly given the numerous policy changes enacted over the last several years. For example, it is unclear what, if any, effect additional flexibility in state work participation rules adopted in the 2012–13 budget might have on the WPR. The state’s future two–parent WPR is also uncertain. Beginning in FFY 2011–12, the state will face the full 90 percent two–parent WPR requirement. Compliance with this requirement will be very difficult, and the impact of the WINS and solely state–funded programs on the two–parent WPR is unknown.
Given Uncertainty, Administration’s Approach Is Appropriate. In summary, California appears compliant with the two–parent requirement in FFY 2009–10 and 2010–11, due to the continuing FFY 2007–08 caseload reduction credit that adjusts the required WPR to zero in those years. It is unclear whether the all–families WPR improved enough for the state to be compliant over the same period. In FFYs 2011–12, 2012–13, and 2013–14, California will likely be out of compliance with both the all–families and two–parent requirements, due to the expiration of the FFY 2007–08 caseload reduction credit. As discussed above, beginning in FFY 2014–15, California may be compliant with the all–families requirement, but likely will not be compliant with the much higher two–parent requirement. In each year that the state is noncompliant, the federal government may, or may not, choose to assess and enforce a penalty (in addition to those already assessed for FFYs 2007–08 and 2008–09). However, even if the state is notified that penalties will be enforced, the state could still exercise its option to enter a corrective compliance plan to avoid paying the penalties. The WPR strategies described above will have a substantial impact on improving California’s compliance with the federal TANF WPR requirement. Given the continued uncertainty surrounding penalty enforcement, it is appropriate to move forward with strategies already identified. Additional steps can be taken as the federal government’s position on penalty enforcement becomes more certain.
Single Allocation Funds County Administration and Provision of Services in CalWORKs Program. Counties receive an annual block grant, known as the single allocation, to cover costs of administering the CalWORKs program and providing services to recipients on behalf of the state. The single allocation is made up of separately budgeted categories, including administration, employment services, and child care. Amounts are budgeted by DSS for each category in aggregate, rather than for each county individually. The total budgeted amount is then allocated among the counties according to formulas developed cooperatively by the state and the County Welfare Directors Association, as required by state law. Amounts budgeted in the different categories are increased or decreased throughout the fiscal year as updated caseload information becomes available. Counties use employment services funding to provide case management and employment counseling to WTW participants and to create numerous job development opportunities, including job search training, job skills assessments, work experience placements, basic skills training, vocational education, and others.
Counties Can, and Do, Spend Flexibly Across Single Allocation Categories. While the administration, child care, and employment services components of the single allocation are budgeted separately, state law allows counties to spend flexibly among these categories as their individual needs and circumstances require. This flexibility recognizes that the state’s budgeting and allocation methodologies generally will not perfectly align with needs at the individual county level. This flexibility also means that budgeted augmentations or reductions in a given category could potentially be shifted to another category in practice. In the past, counties have at times collectively spent less than was allocated for employment services and more than was allocated in other categories, primarily administration. However, significant redirection of funds between categories has been more the exception than the rule. In general, aggregate county expenditures in each category have been relatively similar to allocations, especially in recent years.
Governor Proposes to Augment Employment Services Funding to Enable Prior–Year Policy Changes. As noted previously, the 2012–13 budget resulted in extensive changes to the CalWORKs program by broadening flexibility in state work participation rules and introducing a 24–month limit on adult eligibility under these more flexible rules. The Governor’s 2013–14 CalWORKs budget proposes to augment employment services funding in the single allocation by $143 million. (This proposed amount is in addition to planned increases in employment services spending due to reengagement of previously work–exempt cases.) This increase is intended to enable counties to provide a higher level of employment services in the form of more intensive case management and increased focus on barrier removal activities, in order to assist more families to find sustainable employment prior to reaching the new 24–month limit.
Prior–Year Policy Changes Emphasize Earlier and More Comprehensive Engagement in WTW. Research suggests that a majority of TANF recipients face at least some barriers to sustainable employment. These barriers can include low educational attainment, low English proficiency, lack of work experience, responsibility of caring for disabled parents or children, learning disabilities, poor mental health, domestic violence, substance abuse, criminal records, and others. While the CalWORKs program has been designed to provide services to address many of these barriers, in practice it can be difficult to correctly diagnose which barriers a given case may have and then adequately identify and provide services to remediate them. CalWORKs cases with undiagnosed and unaddressed barriers may fail to comply with program rules, be sanctioned, and subsequently become disconnected from WTW services.
The decision to increase flexibility in state work rules and the introduction of the WTW 24–month time clock reflect a balance between (1) the state’s need to move work–eligible cases toward compliance with federal work rules (in order to meet the federal WPR requirements placed on the state) and (2) a recognition that some cases will require significant barrier remediation before they will be prepared to engage in sustainable employment for the long term. By allowing for greater access to barrier removal services, such as mental health and substance abuse treatment, domestic violence counseling, and education and training opportunities, the hope is that a greater number of work–eligible cases will be prepared to find and keep employment, meet federal work participation requirements before they exhaust their 24–month time limit, and ultimately reach self–sufficiency. The effectiveness of this approach depends on the counties’ ability to more effectively identify barriers to employment, connect recipients with appropriate services and activities available under state rules, and keep recipients engaged in WTW so that progress can be made more rapidly.
Governor’s Proposal Is Consistent With State Policy and Has Merit. It is likely that counties will require additional resources in order to increase the level of employment services provided in a manner consistent with state policy, as reflected by the Legislature’s policy and budget actions. The Governor’s proposal to augment employment services logically follows from policy decisions made in the 2012–13 budget and we believe increased employment services funding can make these policy changes more beneficial to CalWORKs recipients. However, the Legislature should consider whether the level of augmentation proposed is appropriate to provide the level of service intended, as discussed below.
Level of Employment Services Funding Per Case Has Varied Over Time. Since 2001–02, the basic methodology used in the development of the Governor’s budget to plan for upcoming employment services expenditures has been to adjust the prior–year appropriation for changes in caseload, maintaining an implicit level of funding per case. However, numerous policy changes and budget actions have affected the employment services funding base in the intervening years, resulting in variation in the implicit funding per case.
Employment Services Augmentation Based on Updated Budgeting Methodology. The methodology used by DSS to arrive at the $143 million augmentation amount differs from historical practice in two main ways.
- First, the new methodology simplifies the employment services budget and is explicitly based on a defined level of funding, or cost, per case (approximately $361 per month). This cost per case is essentially the average budget allocation per case over 2006–07, 2007–08, and 2008–09, based on budget act appropriations for employment services in those years. In effect, this approach rebenches the employment services funding to prerecession levels. Moving to the new cost–per–case methodology accounts for $96 million of the proposed increase. We believe that the cost–per–case methodology improves on past practice because it is simpler and more straightforward. We also find the administration’s approach of rebenching employment services funding to be reasonable because it would allow counties to provide job development opportunities at a level consistent with what was intended by budget appropriations prior to the recession and the associated policy changes and funding reductions.
- Second, the administration proposes to increase the new cost per case by an additional $21 per month, based on the assumption that county employment services workers will spend more time on each case than they do currently. This is intended to allow for more intensive case management and counseling, and to reach out to cases that are not currently participating due to sanctions. Increasing the cost per case accounts for $47 million of the proposed increase. We believe that increased funding for case management is consistent with past policy and find the administration’s methodology reasonable in that it relies on justifiable workload assumptions.
Choice of Adequate Funding Level Depends on Desired Level of Service. As discussed, the administration’s proposal uses a cost per case that assumes that the adequate level of service is equal to what was intended in budget act appropriations from 2006–07 through 2008–09, and then adds additional funding for enhanced case management. While we find that the administration’s approach in determining the size of the augmentation is reasonable, we note that other approaches may be equally reasonable. The appropriate level of funding for employment services depends on what expectations the Legislature has for service levels under the WTW 24–month time clock.
For example, if a hypothetical cost per case had been determined using actual (prerecession) expenditures rather than appropriated allocations, it would have been lower by about $43 per month than that used by the administration under its new methodology. If this hypothetical expenditure–based cost per case were used in the new methodology, we estimate that the proposed employment services augmentation in 2013–14 would be lower by $97 million. While we find that the administration’s budgeting methodology and the hypothetical alternative just discussed would result in different levels of service, we find that both would be consistent with the policy of focusing resources on employment services.
Legislature May Consider Other Policy Priorities in Determining Appropriate Employment Services Funding Level. The CalWORKs program has the dual statutory objectives of (1) providing a minimum level of subsistence to California families with children and (2) assisting these families to find self–sustaining employment. The adoption of the WTW 24–month time clock and increased flexibility in state work rules in 2012–13, as well as the employment services augmentation proposed for the 2013–14, focus on the second of these two objectives. We note that, as always, the Legislature may have a different set of policy priorities than the administration that guide which policy–driven budget augmentations that it wishes to approve. (The proposed augmentation for employment services stands out as one of a handful of policy–driven augmentations proposed in the Governor’s budget.) In the context of the CalWORKs program, the Legislature could choose to redirect some or all of the funding proposed for the employment services augmentation to support other CalWORKs program goals. For example, some of the funding for the employment services augmentation could be used instead to increase maximum grant levels. Increasing maximum grant levels by 1 percent would result in increased grant costs of approximately $38 million. The earned–income disregard could also be increased, which would have the effect of increasing grants for CalWORKs cases with income and creating an increased work incentive.
Recommend That Legislature Approve TANF–CSAC Funding Swap. The TANF–CSAC funding swap has no net impact on total CalWORKs funding levels and General Fund spending overall, but does result in increased General Fund spending in CalWORKs. This additional General Fund spending provides flexibility in the CalWORKs program that is beneficial to the state by helping to avoid federal penalties and achieve state objectives. In view of this benefit, we recommend that the Legislature approve the TANF–CSAC funding swap as proposed in the Governor’s budget.
Recommend That Legislature Augment Employment Services Funding. We find that the policy changes implemented in the 2012–13 budget imply an increased focus on assisting work–eligible cases to identify and address barriers to employment. The Governor’s proposal to increase funding for employment services is consistent with that policy and the approach used by administration in calculating the amount of the augmentation is reasonable. While we recommend that the Legislature adopt in concept the Governor’s proposal to augment employment services funding, we also recommend that the Legislature determine the amount of such augmentation by considering the level of service it expects given its recent policy actions and the level of funding it deems appropriate in light of its priorities for the CalWORKs program.
Recommend That DSS Report on County Use of Augmented Employment Services Funds. Particularly given the flexibility with which single allocation funds can be used, we recommend that the Legislature direct DSS to report to the Legislature by March 1, 2014, on the counties’ use of funds provided by the augmentation, including a discussion on changes made in the provision of employment services as a result of the augmentation and a preliminary take on outcomes achieved. Such a report could help facilitate the identification of promising ways to better engage WTW participants and help gauge the adequacy of funding provided.
Overview of IHSS. The IHSS program—administered at the state level by DSS—provides in–home care for persons who cannot safely remain in their own homes without such assistance. In order to qualify for IHSS, a recipient must be aged, blind, or disabled and in most cases have income below the level necessary to qualify for SSI/SSP cash assistance. County social workers perform an assessment to determine the number of hours and type of services to authorize an IHSS recipient to receive each month. Recipients are eligible to receive up to 283 hours per month of assistance with tasks such as bathing, housework, meal preparation, and dressing. In most cases, the recipient is responsible for hiring and supervising a provider.
IHSS Is a Medi–Cal Benefit. Close to 99 percent of IHSS recipients receive program services as beneficiaries of the state’s Medicaid health services program (known as Medi–Cal in California) for low–income families with children, seniors, and persons with disabilities. Individuals with disabilities who do not qualify for Medi–Cal—primarily because of their immigration status—comprise about 1 percent of the IHSS caseload. The program is subject to federal Medicaid rules, including the FMAP reimbursement rate for California of 50 percent for most program costs. Historically, for almost all IHSS recipients, 50 percent of program costs were paid for by the federal government, with about 32.5 percent paid for by the state, and 17.5 percent by the counties. Chapter 45, Statutes of 2012 (SB 1036, Committee on Budget and Fiscal Review), altered the historical county contribution by enacting a county IHSS MOE. The MOE requirement replaced the county contribution of 17.5 percent with a requirement that counties generally maintain their 2011–12 expenditure level for IHSS beginning in 2012–13, to be adjusted annually for inflation beginning in 2014–15. Furthermore, the historical cost–sharing arrangements have been altered by ACA, which provides for an enhanced FMAP (56 percent)—known as the Community First Choice Option—for certain services for certain beneficiaries, including IHSS recipients who meet the state’s nursing facility clinical eligibility standards.
The CCI. The CCI is a policy initiative enacted in the 2012–13 budget intended to improve the coordination of care for SPDs. As part of CCI, the IHSS program will shift from a Medi–Cal FFS benefit to a Medi–Cal managed care plan benefit in eight demonstration counties, pending federal approval from CMS. The Governor’s 2013–14 budget proposes to begin this CCI–related shift to managed care on September 1, 2013.
Year–to–Year Expenditure Comparison. The budget proposes $6.2 billion (all funds) for IHSS expenditures in 2013–14, which is a 5.9 percent net increase over estimated revised expenditures in 2012–13. General Fund expenditures for 2013–14 are proposed at $1.8 billion, a net increase of $85 million, or 4.9 percent, above the revised estimate of 2012–13 expenditures. This net increase in total expenditures reflects several factors.
- Sunset of 3.6 Percent Across–the–Board Reduction. Increase of $185 million ($60 million General Fund) because of the sunset of the 3.6 percent across–the–board reduction in IHSS hours that was implemented in 2012–13 and two prior years.
- Increase in IHSS Basic Services Costs. Increase of $152 million ($49 million General Fund) because of (1) a larger caseload, (2) greater hours per case, and (3) higher costs per hour because of an increase in the cost of providing workers’ compensation insurance to IHSS providers.
- Erosion of Savings From Community First Choice Option. Increase of $94 million (General Fund) above estimated 2012–13 expenditures because of stricter federal requirements for IHSS recipients to qualify for the enhanced FMAP associated with the Community First Choice Option beginning July 7, 2013.
- New Services Costs Related to CCI. Increase of $35 million ($11 million as reimbursement from DHCS originating from the General Fund) for (1) increased IHSS hours for existing recipients as a result of CCI and (2) new IHSS recipients who will have transitioned out of institutional care settings into IHSS because of CCI.
- MOE Shift to General Fund. Increase of $30 million General Fund above estimated 2012–13 expenditures because all increases in the non–federal share of IHSS costs above the IHSS county MOE are borne by the state’s General Fund.
- 20 Percent Across–the–Board Reduction. Decrease of $395 million ($113 million General Fund) because the budget assumes the state will prevail in ongoing litigation to allow it to begin implementing a 20 percent reduction in service hours that was a 2011–12 budget solution. We discuss this budget reduction in further detail below.
- Elimination of Services for Recipients Without a Health Care Certificate. Decrease of $80 million ($26 million General Fund) below estimated 2012–13 expenditures because of an increase in the estimated number of IHSS recipients and applicants who are not expected to submit the health care certificate required to receive IHSS.
Caseload Growth. The Governor’s budget assumes the average monthly caseload for IHSS in 2013–14 will be 418,890, a decrease of about 1 percent compared to the most recent estimate of the 2012–13 average monthly caseload. This 2013–14 caseload estimate does not take into account a relatively small but likely increase in IHSS recipients as a result of CCI. Under Chapter 33, Statutes of 2012 (SB 1008, Committee on Budget and Fiscal Review), managed care plans in the eight demonstration counties would have the discretion to transition dual eligibles (SPDs eligible for both Medi–Cal and Medicare) from institutional care settings to home– and community–based services (HCBS), such as IHSS.
Budget Change Proposals. The budget is requesting additional staff resources for the following budget change proposals.
- CCI. The budget requests seven limited–term positions through 2014–15 to address workload associated with shifting IHSS to a managed care plan benefit in eight demonstration counties under CCI. We find that this budget proposal is justified on a workload basis.
- Case Management Information and Payrolling System (CMIPS) II. The budget proposes $510,000 ($255,000 General Fund) to extend four limited–term positions for the CMIPS II IT project. We provide a status update of this project under the County Welfare Automation write–up in this report.
Analyst’s Comments on Overall Budget Proposal. Overall, we find the Governor’s 2013–14 budget proposal for IHSS reasonable. We have reviewed the caseload projections for IHSS and do not recommend any adjustments at this time. If we receive additional information that causes us to change our overall assessment, we will provide the Legislature with an updated analysis. In the section that follows, we discuss the budgetary risk inherent in the budget’s assumption that the 20 percent across–the–board reduction to IHSS hours will begin to be implemented during the course of 2013–14. We offer the Legislature an alternative budget savings solution that could be implemented from the beginning of 2013–14.
The 20 Percent Across–the–Board Reduction
Origin of Reduction. The 2011–12 budget package contained a statutory mechanism, or “trigger,” for further reducing General Fund program expenditures if General Fund revenues were reestimated to fall short of the amount assumed in the 2011–12 Budget Act. One of these reductions was a 20 percent across–the–board reduction in IHSS hours (estimated to save $100 million General Fund in 2011–12). Ultimately, the trigger was pulled. However, in early 2012, a federal judge issued a preliminary injunction preventing the state from implementing this IHSS–related reduction. The Governor’s 2013–14 budget plan assumes the state will ultimately prevail in the ongoing litigation and be able to implement the 20 percent reduction beginning on November 1, 2013, for an estimated partial–year savings of $113 million General Fund.
Legal Risk. The preliminary injunction order issued by a federal judge raised concerns about the reduction’s potential violation of federal Medicaid law, the federal Americans with Disabilities Act (ADA), and due process requirements under the 14th Amendment of the United States Constitution. The judge acknowledged that the state may reduce IHSS hours under certain circumstances, but found that the plaintiffs are likely to succeed in their claims as described below.
- Medicaid Law. At issue was whether the reduction violated federal Medicaid requirements, including: (1) the reasonable standards requirement that eligibility determination and the extent of assistance are consistent with program objectives; (2) the comparability mandate that individuals of comparable need receive comparable services; and (3) the sufficiency requirement mandating that each service must be sufficient in amount, duration, and scope to achieve its purpose.
- ADA. At issue was whether the reduction of IHSS hours would put recipients at serious risk of institutionalization, in violation of the ADA that requires states to provide services in the most integrated setting appropriate to the needs of persons with disabilities.
- Due Process. At issue was whether the state’s notice to IHSS recipients and the supplemental care application to seek a restoration of lost hours would meet the requirements of due process, whereby the state must provide IHSS recipients with “timely and adequate notice” of the reduction and “an effective opportunity to defend” themselves.
Litigation Update. As of the date of this analysis, an appeal of the preliminary injunction is scheduled to be heard in March 2013. If the state prevails, then it may be able to begin implementing the 20 percent reduction in IHSS hours by the November 1, 2013 date assumed in the budget. However, below we raise fiscal and policy concerns with the 20 percent reduction.
Fiscal and Policy Concerns With 20 Percent Reduction. When the state enters into litigation on an enacted budget solution, some measure of uncertainty exists about whether the budget solution will ultimately be implemented. For the 20 percent reduction in particular, the federal judge has raised legal concerns that call into question the state’s ability to ultimately implement the reduction and achieve the budget’s assumed partial–year savings of $113 million in 2013–14. This assumption of savings is also susceptible to erosion should a greater–than–anticipated number of IHSS recipients apply for and receive a full or partial restoration of lost hours through the supplemental care application process.
Regardless of the outcome of the litigation concerning the 20 percent reduction, we think that the Legislature should consider whether a reduction of this magnitude is the appropriate policy to pursue at this time. Subsequent to the 20 percent reduction’s enactment in 2011–12, the Legislature enacted CCI (Chapters 33 and 45), with a stated policy objective to align financial incentives so as to shift utilization away from institutional care settings and toward HCBS, such as IHSS. The IHSS program is the most commonly utilized form of HCBS among SPDs, and therefore critical to maintaining SPDs in their homes and communities. A reduction in IHSS hours of this magnitude may put some recipients at risk of institutionalization, which works against one of the stated policy goals of CCI.
3.6 Percent Across–the–Board Reduction Has Been Successful in Achieving Savings. The 3.6 percent across–the–board reduction due to sunset on June 30, 2013, has been successfully implemented without legal challenge in three fiscal years—2010–11 through 2012–13. In 2012–13, the reduction is effective for 11 months, with estimated savings of $60 million General Fund, or about $5.5 million per month. If the Legislature continued the 3.6 percent reduction through 2013–14, the full–year savings from the reduction would be approximately $66 million General Fund.
In light of the fiscal and policy concerns with the 20 percent reduction discussed above, we recommend that the Legislature take the following two actions.
- Repeal the 20 Percent Across–the–Board Reduction. We recommend that the Legislature repeal the 20 percent reduction because of the uncertainty of achieving the estimated savings and the potential for adverse policy consequences. Fiscally, the 20 percent reduction is subject to a particularly high level of uncertainty due to the ongoing litigation and potential savings erosion even if implementation were to occur. If the reduction were ultimately implemented, the magnitude of the reduction may cause some recipients to be at risk of avoidable institutionalization—an outcome inconsistent with the Legislature’s policy goals in implementing CCI.
- Continue the 3.6 Percent Across–the–Board Reduction. In lieu of the 20 percent reduction, we recommend that the Legislature continue the 3.6 percent reduction on an ongoing basis because it would result in a relatively certain amount of General Fund savings while diminishing the risk of avoidable institutionalization. Unlike the 20 percent reduction, the 3.6 percent reduction has not been subject to legal challenge and has been successfully implemented in 2012–13 and two prior years. In other words, given the risk that the 20 percent reduction may not be implemented, we think that the state would be fiscally better off by continuing the 3.6 percent reduction to achieve relatively certain savings. From a policy perspective, the continuation of an existing 3.6 percent reduction is less likely than the 20 percent reduction to lead to unnecessary out–of–home placement among recipients, which aligns with the goals of CCI.
The Governor’s budget includes funding proposals for two county welfare automation projects—CMIPS II and the Child Welfare System–New System (CWS–NS) project. We discuss each of these budget proposals below.
The Project. The DSS is in the process of replacing the CMIPS (commonly referred to as Legacy CMIPS) with CMIPS II. Legacy CMIPS is the existing automated statewide system that performs payroll and case management functions for all IHSS providers and recipients. (For more information on the IHSS program, please see the IHSS write–up earlier in this report.) The 30–plus–year–old Legacy CMIPS has become outdated and is unable to support many of the major technical or functional modifications necessary to support legislatively enacted program changes as well as caseload management needs. The CMIPS II will update timesheet processing for providers, implement an enhanced user–friendly system, and hold approximately 30 percent more data. The CMIPS II project entered into the maintenance and operation (M&O) phase with the conversion of Yolo, Merced, and DSS as “the 59th county” in July 2012 from Legacy CMIPS to CMIPS II. The remaining 56 counties will transition incrementally with full statewide operation in 2013–14.
Recommend Approval of Governor’s Budget Proposal. The Governor’s budget proposes an increase of $510,000 ($255,000 General Fund; $255,000 federal reimbursements) for a two–year extension of four limited–term positions to transition from Legacy CMIPS to CMIPS II and for ongoing CMIPS II M&O activities. We recommend approval of the Governor’s proposal as it ensures the appropriate resources are maintained to continue to move the CMIPS II project forward towards full statewide operation as planned for 2013–14.
The DSS proposes to replace the existing Child Welfare Services/Case Management System (CWS/CMS) with CWS–NS. Here we provide background regarding the CWS/CMS, describe the CWS–NS project, discuss the Governor’s proposal to authorize funding for the planning and procurement phase of the CWS–NS project, and recommend approval of the Governor’s proposal.
The CWS/CMS. The CWS/CMS is the statewide case management system currently supporting the state’s CWS program. The CWS workers throughout the state rely on CWS/CMS for access to child, family, and other case–related information to make timely decisions, perform effective case management, and ultimately keep children safe and families intact. The system has been operational since 1997 and is maintained and operated by an independent contractor for $78.9 million ($39.9 million General Fund) annually.
Federal Government Provides Enhanced Funding. In 1993, the federal government offered enhanced funding to states that agreed to develop a Statewide Automated Child Welfare Information System (SACWIS). A SACWIS performs specified functions, including processing child abuse investigations and preparing foster care case plans. If a state chose to develop such a system, then the federal government provided “incentive funding” at 75 percent of total costs for the first three years of the project’s development and then 50 percent for the subsequent years. In 1994, California received federal approval to develop CWS/CMS as SACWIS–compliant. In 1997, the state announced the completion of the CWS/CMS system when it became operational in all counties.
Federal Government Expresses Concerns About CWS/CMS. The federal government, however, did not consider CWS/CMS complete in 1997 because the system did not meet all the SACWIS requirements. Starting in 1999, the federal government raised concerns about the inability of the CWS/CMS system to meet SACWIS requirements. In June 2003, the federal government officially notified the state that it did not consider CWS/CMS to meet SACWIS requirements. As a result, the federal government reduced its share of funding for CWS/CMS from roughly 50 percent to 30 percent. In addition, the federal government notified the state that it would not provide any federal funding for the project after August 2005.
Go–Forward Plan Is State’s Strategy to Address Federal Concerns. In October 2004, SACWIS funding was conditionally restored retroactively after the federal government approved the state’s strategy to address the federal government’s concerns about achieving SACWIS compliance, known as the Go–Forward Plan. As a result of the federal agreement, the Legislature mandated the development of a Technical Architecture Alternatives Analysis (TAAA) Study to evaluate a number of approaches to redesigning CWS/CMS to better meet the needs of CWS workers and the SACWIS requirements. Based on the TAAA recommendation in 2005, a decision was made to continue to operate CWS/CMS while simultaneously building a new SACWIS using a web–based architecture. The plan for the new system became the CWS/Web project. The 2011–12 Budget Act indefinitely suspended the CWS/Web project because of resources challenges (the project was suspended while in the procurement phase).
The CWS Automation Study Recommends the Buy/Build Option. Additionally, as a result of its deliberations on the 2011–12 budget, the Legislature directed DSS (in Chapter 32, Statutes of 2011 [AB 106, Committee on Budget]) to partner with the Office of Systems Integration (OSI) in HHSA to assess (1) the business needs associated with CWS, (2) the current case management system, and (3) the viable automated system options to meet the requirements of CWS. In April 2012, after a review of several alternatives, the CWS automation study found it was neither feasible nor cost–effective to maintain the CWS/CMS and recommended its replacement. The report recommended a buy/build approach involving the purchase of an application (or a suite of applications) that is already available and used as is, with any additional functionally built over time, so as to customize the system for California’s program needs. The replacement system project is referred to as CWS–NS.
The CWS–NS. The CWS–NS will use the CWS automation study recommended buy/build approach to replace the existing CWS/CMS. The successful implementation of the CWS–NS is intended to meet the business needs of CWS, comply with state and federal laws and regulations, result in enhanced data reliability and availability, allow user mobility, and allow for automated system interfaces with other state partners for data sharing. The CWS–NS buy/build approach is expected to allow the state to qualify for continued SACWIS federal financial participation (FFP) for M&O costs associated with the CWS/CMS while also claiming FFP for implementing the new automated system. The CWS–NS is estimated to cost $392.7 million, including one full year of M&O, and planned to be fully implemented by September 2017.
The Governor makes two proposals regarding the CWS–NS.
- Funding for OSI to Support the CWS–NS Project. The Governor proposes $2.7 million in special funds (funded by $1.35 million General Fund $1.35 million and federal funds) for eight positions (all two–year limited–term positions) in OSI to support the CWS–NS project during the planning and procurement phase.
- Funding for DSS to Support the CWS–NS Project. The Governor proposes $1 million ($482,000 General Fund, $506,000 federal funds, and $39,000 reimbursements) for nine positions (all two–year limited–term positions) in DSS to support the CWS–NS project during the planning and procurement phase.
The resources will provide the necessary project management, fiscal, procurement and contracting, business analysis, and technical expertise to support the development of CWS–NS project during the planning and procurement phase.
CWS/CMS Continues to Be Noncompliant. The CWS/CMS continues to be noncompliant with federal SACWIS requirements even though the Administration of Children and Families continues to provide the state with FFP at the enhanced level of 50 percent. Continued failure to comply, however, could jeopardize future FFP funding and require a payback of SACWIS FFP claimed since the beginning of the CWS/CMS project in the 1990s.
Processes Used to Achieve Program Compliance Inefficient. Although the CWS/CMS system is noncompliant with state and federal regulations, the CWS program itself is compliant with state and federal regulations. The program uses a series of manual processes and external technologies to fully comply with state and federal requirements even as the CWS/CMS system remains noncompliant. The manual and technical processes used to ensure program compliance are costly and divert CWS workers from their program services delivery work.
Lower Ongoing Costs Projected for CWS–NS Relative to Current System. The cost of maintaining CWS–NS is estimated to be $23.9 million in 2018–19, when the system is fully implemented. With the approved SACWIS FFP of 50 percent, the approximate annual General Fund contribution for system maintenance is estimated to be about $12 million. This equates to annual General Fund savings of $27.9 million compared to the cost of maintaining the existing system ($78.9 million total, $39.9 million General Fund).
Current System Offers Limited Functionality. The current automated system does not fully support critical child welfare operations and CWS workers do not have the tools or access to all the information needed and available to do their jobs. The new system will automate existing manual tasks, provide CWS workers the capability and flexibility needed to effectively perform their duties, and provide improved service delivery to the program’s beneficiaries.
We recommend approval of the Governor’s proposal for $2.7 million for OSI and $1 million for DSS to support the CWS–NS project during the planning and procurement phase. The CWS–NS is designed to comply with state and federal law and incorporate critical business functionality to provide effective and efficient child welfare services. The approval of this request will provide the necessary resources for the planning and procurement phase of the CWS–NS project.
Return to LAO 2013-14 Budget: Social Services Table of Contents
Return to LAO 2013-14 Budget: Health Table of Contents
Return to LAO 2013-14 Budget: Full Table of Contents