In 2010, federal approval of more flexibility for the state’s Medicaid program significantly expanded who is eligible for federally funded health care coverage in California and how that care is financed in the near term. In the longer term, an optional Medicaid eligibility expansion that is part of the ACA could further expand who is eligible for federally funded health care coverage and increase the federal share of costs for some individuals. As we discuss below, these changes have created new opportunities to use federal funds for certain medical services provided to some state prison inmates.
Medicaid is an optional joint federal–state program that provides health insurance coverage to certain low–income populations. In California, the Medicaid program is administered by DHCS and is known as Medi–Cal. Below, we provide an overview of how Medi–Cal is financed, who is eligible for the program, what benefits they receive, and how the program is administered.
Medi–Cal Costs Split Between the State and Federal Government. In choosing to operate a Medicaid program, states receive federal funding for a significant share of the program costs. The percentage of program costs funded with federal funds varies by state and is known as the federal medical assistance percentage, (FMAP or “federal match”). In most cases, the federal match is determined annually by comparing the state’s per capita income to the national average. The Medi–Cal Program currently receives a 50 percent federal match for most services provided to beneficiaries, as well as for state and county costs to administer the program. In other words, the program generally receives one dollar of federal funds for each state dollar spent on Medi–Cal beneficiaries and administration. The federal government also provides an enhanced federal match for certain program costs, such as services for groups with particular medical needs or the implementation of technology systems.
Medi–Cal Provides a Wide Array of Health Care Services to Eligible Individuals. Federal law establishes some minimum requirements for state Medicaid programs regarding the types of services offered and who is eligible to receive them. Required services include hospital inpatient and outpatient care, nursing home stays, and doctor visits. California also offers an array of medical services considered optional under federal law, such as coverage of prescription drugs and durable medical equipment. Medi–Cal services are provided through two main systems: fee–for–service (FFS) and managed care. In a FFS system, a health care provider receives an individual payment for each medical service provided. In a managed care system, managed care plans receive a set fee per patient in exchange for providing health care coverage to enrollees.
Currently, Medi–Cal eligibility requires individuals to have a low income and to be in certain categories, such as being in a family with children, being blind or pregnant, being over 65 or under 19 years of age, or having a disability. Individuals who are not lawfully residing in the United States are generally ineligible for Medi–Cal. Low–income, childless adults are also generally ineligible for Medi–Cal. (However, as we discuss below, such individuals may be eligible for county–operated LIHPs.) The income threshold used to determine Medi–Cal eligibility varies, but for some groups (such as parents) the income threshold is about 100 percent of the Federal Poverty Level (FPL). (The FPL is the income level at which the federal government considers individuals of families to be impoverished.) In 2012, the FPL was $11,170 per year for an individual and $23,050 for a family of four.
State and Counties Administer Medi–Cal. Most Medi–Cal benefits are administered at the state level by DHCS, although some benefits are administered by other state departments. The counties administer some Medi–Cal benefits at the local level and also determine the eligibility for most persons applying to enroll in Medi–Cal. The DHCS contracts with a private sector vendor to act as a fiscal intermediary for Medi–Cal. The fiscal intermediary processes claims submitted by Medi–Cal providers for services rendered to beneficiaries.
In 2010, Congress passed and President Obama signed the ACA, which includes a provision allowing states to expand the Medicaid program beginning in 2014. In June 2010, DHCS obtained a 1115 Bridge to Reform Waiver (hereinafter referred to as the “waiver”) from the federal government that includes components intended to facilitate the state’s progress towards implementing federal health care reform, such as the establishment of LIHPs. (The Centers for Medicare and Medicaid Services [CMS] sometimes approves waivers to allow states to waive federal Medicaid requirements in order to have the flexibility to modify their programs in ways that promote Medicaid program objectives.) Figure 1 summarizes some key aspects of Medi–Cal and county LIHPs, as well as what Medi–Cal might look like in 2014 if the state exercises its option under ACA to expand the program.
Figure 1
A Comparison of Selected Health Care Programs for Low–Income Californians
|
Program Element
|
Medi–Cal
|
Low–Income Health Program (LIHP)
|
Medi–Cal in 2014a
|
|
Eligible Population
|
Certain parents and children, seniors (aged 65 or older), persons with disabilities, and pregnant women—meeting varying income thresholds.
|
Certain low–income individuals who do not qualify for Medi–Cal—income thresholds vary by county.
|
Certain individuals with income up to 133 percent of FPL.
|
|
Federal Match
|
50%
|
50%
|
50% or 100%b
|
|
Eligibility Determination
|
Mostly counties
|
Counties
|
Mostly counties
|
|
Enrollment
|
Counties or DHCS
|
Counties
|
Counties or DHCS
|
|
Submission of Claims to DHCS
|
Providers
|
Countiesc
|
Providers
|
New LIHP Initiative Creates Bridge to Expansion. Among other things, the waiver approved for California in 2010 allows counties to leverage federal funds to create LIHPs to provide health care for indigents who do not qualify for Medi–Cal—a population consisting largely of childless adults. Funding for LIHPs is generally split between counties and the federal government with each covering half of the costs for services and administration. Counties are responsible for determining eligibility, enrolling individuals, paying providers for health care provided to beneficiaries, and submitting cost reports or invoices that reflect these expenditures to DHCS. The DHCS is responsible for reviewing these reports and invoices to determine the allowable amount of federal reimbursement to county LIHPs and ensuring that county LIHPs are adhering to the terms of the waiver and operating consistent with federal law. The services provided to LIHP beneficiaries are generally similar to those provided to Medi–Cal beneficiaries.
As of February 2013, 55 of the state’s 58 counties are operating or plan to operate LIHPs. (This includes three counties that currently have not implemented LIHPs but plan to do so.) Certain aspects of LIHPs (such as the maximum income threshold for eligibility) vary from county to county. Under the terms of the waiver, counties may at any time “cap” enrollment, or exclude any additional beneficiaries from enrolling into the program. Currently only one county, Santa Cruz, has done so. In order to be eligible for a county’s LIHP, individuals must have established legal residency in that county. In addition, individuals who are eligible for Medi–Cal cannot be enrolled into a LIHP. Federal funding for LIHPs will expire in January 2014. While the state has not yet finalized a plan for providing coverage to the indigent population covered by LIHPs in 2014 and beyond, such individuals would be transitioned into Medi–Cal if the state exercises its option to expand Medi–Cal under the ACA, as we describe below.
Under ACA, State Can Expand Medi–Cal With Increased Federal Match in 2014. The ACA gives states the option to significantly expand their Medicaid programs, with the federal government paying for a large majority of the additional costs. Beginning January 1, 2014, federal law gives state Medicaid programs the option to cover most individuals under age 65—including childless adults—with incomes at or below 133 percent of the FPL. As shown in Figure 2, the federal matching rate for coverage of this expansion population will be 100 percent for the first three years, but will decline between 2017 and 2020, with states eventually bearing 10 percent of the additional cost of health care services for the expansion population. The Governor’s 2013–14 Budget Summary includes a commitment to expanding Medi–Cal but presents two possible options for doing so, which we describe in the nearby box. We note, however, that the Legislature has not yet taken action at the time of this analysis to expand the Medi–Cal Program. While policymakers are also still determining how to implement certain changes to Medi–Cal that are required by the ACA in 2014, certain fundamental aspects of the existing program (such as the provision of federally required benefits) will not change.
The administration has stated its commitment to adopting the optional Medicaid expansion authorized under the Patient Protection and Affordable Care Act. The Governor’s 2013–14 Budget Summary presents two distinct approaches—a state–based expansion and a county–based expansion—but does not propose a specific approach. Nor has the Governor provided much detail on how these two approaches would be operated, instead leaving those details to be worked out through the legislative process.
State–Based Expansion Approach. Under the state–based expansion approach, administration of the program would likely be done similarly to the existing Medi–Cal Program and managed care delivery system. Generally, covered benefits for the expansion population would be similar to benefits available to the currently eligible population.
County–Based Expansion Approach. Under this alternative approach, the counties would have operational and fiscal responsibility for implementing the Medi–Cal expansion, more similar to how the Low–Income Health Programs (LIHPs) operate. Operational responsibilities include some administrative functions (such as processing claims billed by providers) that are currently performed by the state and Medi–Cal managed care plans for the currently eligible population. Counties could build upon their existing medical programs for indigents and LIHPs to operate the expansion. The county–based expansion would be required to meet statewide eligibility standards and cover a minimum benefits package. Counties would also have the option of covering additional benefits (other than long–term care) for the expansion population. The administration indicates that this approach would likely require federal approval.
Figure 2
Federal Matching Rate for Health Care Services
Provided to Medicaid Expansion Population
|
Calendar Year
|
Federal Match
|
|
2014
|
100%
|
|
2015
|
100
|
|
2016
|
100
|
|
2017
|
95
|
|
2018
|
94
|
|
2019
|
93
|
|
2020 and thereafter
|
90
|
The state is responsible for providing comprehensive medical care, including primary and specialty care, to each of the roughly 124,000 inmates incarcerated in its 33 prisons. Spending on these services in 2011–12 totaled $1.8 billion. While inmate medical services have historically been funded exclusively from the state General Fund, the recent changes in federal health care policy have expanded the potential to receive federal funding for off–site inpatient medical care delivered to certain inmates.
Inmate Medical Program. In April 2001, a class–action lawsuit, known as Plata v. Brown, was filed in federal court contending that the state violated the Eighth Amendment of the U.S. Constitution by providing inadequate medical care to prison inmates. The court found that the state’s inmate medical care program was “broken beyond repair” and was so deficient that it resulted in the unnecessary suffering and death of inmates. In February 2006, after finding that the state had failed to comply with numerous court–ordered remedial actions, the Plata court appointed a Receiver to take over the direct management and operation of the state’s inmate medical care program from the California Department of Corrections and Rehabilitation (CDCR).
While most inmate medical services are delivered within prison by state–employed primary care physicians and nurses under the management of the Receiver, there are certain circumstances that require inmates to be referred off–site to hospitals and clinics in the community. This mainly occurs when inmates require certain specialty care services (such as complicated surgical operations) that are often unavailable at the state’s own prison hospitals and clinics. According to the Receiver, prison health care administrators generally attempt to contract with specialty care providers to come to prisons to provide specialty care services. However, they are not always able to do so typically because (1) of the inadequacy of the prison’s health care facilities and equipment or (2) there are no specialty care physicians willing and able to come into the prison to deliver the care. In addition, inmates are referred off–site when they require emergency or urgent care and the prison’s primary care physicians are unavailable or lack the expertise or equipment necessary to treat the problem. In 2011–12, the Receiver spent $263 million for off–site services. Of this amount, $109 million was for inpatient care—that is hospital stays lasting 24 hours or more. Most of these services are provided by a network of providers based on a fixed FFS rate negotiated by a Preferred Provider Organization (Health Net) on behalf of the Receiver.
LIHPs and ACA Expand Number of Inmates Eligible for Federal Match. Federal law generally excludes individuals who are inmates being held involuntarily in an institutional setting (such as in county jails, state and private prisons, juvenile detention centers, or state mental health hospitals) from the Medicaid program. There is, however, an important exception to this rule that was clarified by CMS in 1997. Specifically, inmates who are referred off–site for inpatient care lasting at least 24 hours are not excluded from participation in the Medicaid program if they otherwise meet the program’s eligibility requirements. In other words, when inmates receive such care at a hospital, nursing facility, or other facility that is outside of the correctional system, they can be enrolled into Medi–Cal or a LIHP and a federal match can be applied to the state’s cost of the entire duration of their inpatient stay. (The federal match amount is based on the Medi–Cal rate for the provided services, not the actual amount paid by the state.) As we discuss later, the state did not begin implementing a system to obtain federal funds until April 2011. Federal funds can also be used for inpatient care for individuals in other state and local custodial facilities, as we describe in the nearby box.
In addition to state prison inmates, other populations in institutional settings are potentially eligible for participation in Medi–Cal and Low–Income Health Programs when receiving off–site inpatient care. These populations include the roughly 77,000 inmates being held in county jails in California, most of the 5,500 patients being held in state mental health hospitals operated by the Department of State Hospitals, the 800 juvenile wards being held in state custody by the Division of Juvenile Justice, and 8,500 juveniles incarcerated in detention facilities operated by county probation departments. As with state inmates, these other populations have to meet the program’s eligibility requirements, and the care has to be provided in an off–site facility for at least 24 hours. Based on our conversations with state and local officials, very few of these agencies are currently taking advantage of the opportunity to seek federal reimbursement for these populations.
According to data provided by the Receiver, 72 percent of inmates currently receiving off–site inpatient services meet the eligibility requirements of either a LIHP or Medi–Cal. Most of the remaining 28 percent are ineligible because they are not lawfully residing in the United States or lack a valid social security number. Of those who are eligible, roughly 20 percent qualify for Medi–Cal while the remaining 80 percent qualify for county LIHPs. If California exercises its option to expand Medi–Cal to include low–income childless adults in 2014, the inmates who currently qualify for LIHPs would be transitioned into Medi–Cal. Because these inmates would be part of the Medi–Cal expansion population, the federal match for their eligible off–site inpatient care would initially be 100 percent.
Recognizing the opportunity to achieve General Fund savings by obtaining federal funds for inmate medical care, the Legislature passed Chapter 729, Statutes of 2010 (AB 1628, Blumenfield), which directed CDCR to seek federal reimbursement for off–site inpatient services delivered to inmates eligible for Medi–Cal and LIHPs. Specifically, Chapter 729 directed the Receiver—in collaboration with DHCS—to pursue these savings by developing a process for enrolling eligible inmates into Medi–Cal and LIHPs and claiming federal reimbursement for eligible services delivered to these inmates. The legislation also gave DHCS the discretion to require counties to enroll eligible inmates into their LIHP as a precondition for operating a LIHP.
The state has developed a process, consistent with Chapter 729, for obtaining federal funds for certain inmate health care services. However, due to a couple of procedural problems, which we describe in detail below, the state has not been able to maximize the available federal funding. In addition, it appears that DHCS staffing levels for the program may be higher than necessary, particularly in future years.
In order to meet the requirements of Chapter 729, the Receiver has developed, in collaboration with DHCS and county LIHP administrators, a process for enrolling eligible inmates into Medi–Cal and LIHPs and for claiming federal reimbursement for eligible services. The new process, which differs substantially from the typical Medi–Cal and LIHP administrative processes, was first implemented in April 2011. The process is illustrated in Figure 3 and described in more detail below.
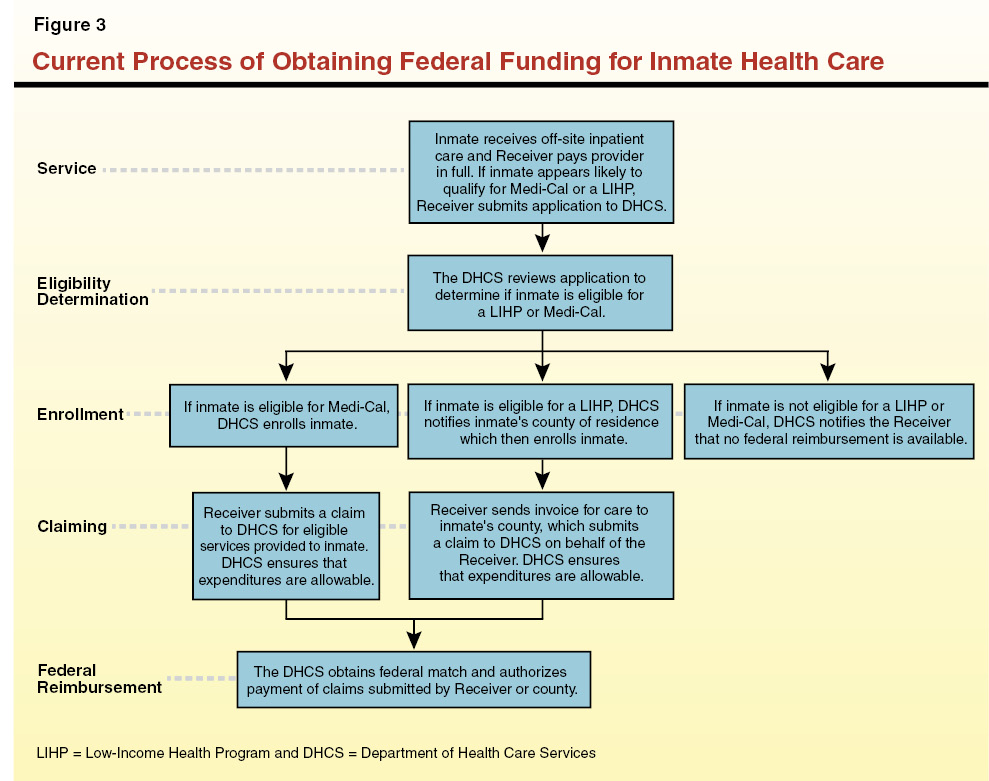
Receiver Identifies Potentially Eligible Inmates. When inmates are referred to off–site providers for inpatient care, the Receiver pays the full cost of the medical services at whatever rate has been negotiated with the provider. The rates paid by the Receiver vary across the state but they are generally higher than the reimbursement rates set by Medi–Cal for similar services. The Receiver’s staff reviews the files of inmates receiving inpatient care and identifies those who may meet the eligibility requirements for participation in Medi–Cal or a LIHP. The staff then completes and submits an application for each potentially eligible inmate to DHCS.
DHCS Determines Inmate Eligibility for Medi–Cal and LIHPs. When DHCS receives an application from the Receiver, they first make a determination of whether the inmate meets the eligibility requirements for Medi–Cal. Specifically, they determine whether the inmate’s income is below 133 percent of FPL, whether they have legal residency in California, and whether they fall into one of the categories required for eligibility (such as being disabled or elderly). If so, the department enrolls the inmate into Medi–Cal (as described below); if not, the department determines if the inmate is eligible for a LIHP (specifically that the inmate has low income and legal residency in a LIHP county). Because LIHPs differ by county, DHCS must determine whether the inmate meets the LIHP requirements of the county in which they legally resided before being sentenced to prison. If so, DHCS notifies the department in that county responsible for LIHP administration. (Several counties are part of a consortium—the County Medical Services Program [CMSP]—that does LIHP enrollment for those counties. For inmates from these counties, the DHCS notifies the CMSP governing board rather than the individual county.)
For Medi–Cal Eligible Inmates, DHCS Responsible for Enrollment and Claiming. If DHCS determines that an inmate is eligible for Medi–Cal, it will then enroll that inmate into the program. This involves entering the inmate’s information into the Medi–Cal Eligibility Data System. Once the inmate has been enrolled, the Receiver will then submit claims for expenses for off–site inpatient care for that inmate to DHCS. The department certifies that the expenditures are allowable under Medi–Cal and then works with a fiscal intermediary to claim the federal match of 50 percent of the cost of the Medi–Cal rate for the services. Finally, DHCS receives the match from the federal government and transfers the funds to the Receiver.
For LIHP Eligible Inmates, Counties Responsible for Enrollment and Claiming. Because the waiver authorizing county LIHPs specifies that only counties can enroll inmates, the Receiver cannot obtain a federal match under these programs without cooperation from counties. Specifically, the Receiver must enter into MOUs with counties that formalize such details as how applications for enrollment will be processed and at what rate the Receiver will reimburse counties for their administrative costs. In order to encourage county cooperation, state law gives DHCS the discretion to require counties to enroll eligible inmates into their LIHP as a precondition for operating a LIHP. In other words, if a county refuses to enroll inmates into their LIHP, DHCS can preclude that county from operating a LIHP and therefore restrict its access to federal funding.
For inmates eligible for a LIHP but not for Medi–Cal, DHCS notifies the county in which the inmate resided prior to being sentenced to prison. In cases where counties have an MOU in place with the Receiver, the counties are then responsible for enrolling inmates into their LIHP. (Currently, not all counties have MOUs in place with the Receiver, for reasons we discuss below.) The Receiver sends the invoices for off–site inpatient care for that inmate to the county, which is then responsible for submitting a claim for federal reimbursement on behalf of the Receiver to DHCS. Finally, DHCS reviews the claim, obtains the federal match if the claim is allowable, and authorizes reimbursement to the Receiver. Under state law, the Receiver is responsible for reimbursing counties for their administrative costs associated with enrolling inmates and claiming federal reimbursement so that they incur no additional costs under the arrangement. As mentioned earlier, the administration has presented two possible options for expanding Medi–Cal in 2014. If the Legislature chooses to implement the county–based approach, that may require modifications to the above process, which we describe in the nearby box.
The Governor’s budget proposes to expand Medi–Cal in 2014 as allowed under the Patient Protection and Affordable Care Act but does not specify whether to take a state– or county–based approach. If the Legislature chooses to implement a state–based Medi–Cal expansion, all new enrollments for the purposes of obtaining federal funding for off–site inpatient care for inmates are likely to be done following the current process used to enroll inmates into Medi–Cal. If, however, the Legislature opts for a county–based Medi–Cal expansion, a new state waiver as well as certain modifications to the inmate enrollment process may be required. For example, depending on how the county–based approach is implemented, the Receiver may have to sign new memoranda of understanding with counties to enroll inmates who are part of the Medi–Cal expansion population into the their programs and to certify expenditures for services delivered to those inmates, similar to the current process used for enrolling and claiming for Low–Income Health Program eligible inmates. Whichever Medi–Cal expansion approach the Legislature selects, it shall want to ensure that there is an efficient inmate enrollment and claiming process that conforms in order to maximize available federal funding.
Although the state has implemented a process for obtaining federal funding for certain inmate health care services, there are a couple of procedural problems that are preventing the state from maximizing potential federal funding.
Some LIHP Counties Have Not Signed MOUs With the Receiver. The Receiver began negotiations with counties on the terms of the enrollment and claiming process for LIHP eligible inmates in 2011. As shown in Figure 4, the Receiver has secured MOUs with 12 counties. About 71 percent of state inmates receiving off–site inpatient services (excluding inmates eligible for Medi–Cal or who lack legal residency) are from these counties. These counties have agreed to an administrative reimbursement rate of $10 per inmate enrolled into their LIHPs. Three counties (Merced, Fresno, and San Luis Obispo) have declined to operate a LIHP. One county, Santa Cruz, did not sign a MOU with the Receiver before imposing an enrollment cap and thus cannot enroll any inmates into its LIHP even if it signed an MOU with the Receiver. The remaining 42 counties are either currently operating or plan to implement a LIHP but have not signed MOUs with the Receiver on the terms of enrolling eligible inmates into their LIHPs. The DHCS has not exercised its authority to bar a county from operating a LIHP, if it refused to enroll inmates in its program.
Figure 4
Status of MOUs Between Counties and
Receiver to Enroll Inmates in LIHP
|
|
|
LIHP Counties With MOUs With Receiver
|
|
Alameda
|
|
Kern
|
|
Los Angeles
|
|
Orange
|
|
Placer
|
|
Sacramento
|
|
San Bernardino
|
|
San Diego
|
|
San Francisco
|
|
San Joaquin
|
|
San Mateo
|
|
Ventura
|
|
LIHP Counties Without MOUs
|
|
Counties that are part of CMSPa
|
|
Contra Costa
|
|
Monterey
|
|
Riverside
|
|
Santa Clara
|
|
Counties Planning to Implement LIHP
|
|
Santa Barbara
|
|
Stanislaus
|
|
Tulare
|
|
LIHP Counties With Enrollment Caps
|
|
Santa Cruz
|
|
Non–LIHP Counties
|
|
Fresno
|
|
Merced
|
|
San Luis Obispo
|
According to the Receiver, the primary obstacle to securing MOUs with the remaining counties has been disagreement over an appropriate reimbursement rate. Specifically, some counties feel that the $10 per enrollee reimbursement proposed by the Receiver—which is based on a study of costs in Orange County—is insufficient to cover their costs. While we have not undertaken an analysis of county by county administrative costs, it is likely that costs do vary somewhat by county. For example, smaller counties may require a slightly higher reimbursement rate because they have fewer enrollees and thus a smaller volume of cases over which to spread their fixed costs of implementing a system to enroll inmates. However, we note that, according to the Receiver, none of the counties requesting a larger reimbursement fee have been able to produce any analysis indicating that $10 is insufficient.
If and when the Receiver is able to secure MOUs with the remaining counties, it is possible to retroactively claim federal reimbursement for services that have already been delivered to inmates who are subsequently enrolled in those counties’ LIHPs. For example, Los Angeles County implemented a LIHP in October 2011 but did not sign an MOU with the Receiver until October 2012. Upon signing the MOU, Los Angeles County began enrolling LIHP eligible inmates who have received off–site inpatient care since October 2011, and the Receiver has submitted a claim for federal matching funds for those services. We note, however, this process of retroactively claiming reimbursement for services previously delivered may not be possible in all cases. That is because some counties may choose to cap their LIHP enrollment before signing MOUs with the Receiver. For example, because Santa Cruz has already capped enrollment, the Receiver will be unable to access federal funds for any services that have been or will be provided to LIHP–eligible inmates from Santa Cruz County. Based on data provided by the Receiver, the share of federal funding potentially available to LIHP–eligible inmates from the 39 counties that are currently operating LIHPs (without enrollment caps) and do not have MOUs with the Receiver is $13 million over the 2011–12, 2012–13, and 2013–14 fiscal years. In other words, if the Receiver is unable to secure MOUs with these counties or is unable to do so before they impose enrollment caps, the state would lose the opportunity to receive these federal funds.
DHCS Unable to Process Certain Medi–Cal Claims Due to Data Exchange Problems. Between May and December 2012, the Receiver submitted about 900 claims for federal reimbursement for off–site inpatient services delivered to Medi–Cal eligible inmates to DHCS. However, DHCS has been unable to process two–thirds of these claims. The DHCS informs us that staff are still in the process of identifying why these claims have not been processed. Based on some preliminary data provided by the department, it appears that some claims were rejected because they are invalid (such as claims for services that are ineligible for Medi–Cal reimbursement). In other cases, however, it appears that valid claims have been rejected because of problems in the claiming process. In particular, many of the claims cannot be processed due to a technical problem in the software used by the fiscal intermediary. According to DHCS, the software has erroneously rejected over 250 claims for certain inmates who meet the eligibility requirements for both Medi–Cal and Medicare, commonly referred to as “dual eligibles.” (Inmates are ineligible to receive Medicare.) Other claims have been rejected because individuals involved in developing and processing the claims (such as DHCS and the Receiver’s staff and medical providers) have entered inaccurate data.
According to DHCS, staff are working with the fiscal intermediary and expect to resolve the software issue affecting dual–eligible inmates by March 2013. We note, however, that staff have been aware of this problem for several months and have evidently been unable to find a solution. If and when this issue is resolved, DHCS has indicated that they will be able to retroactively claim federal reimbursement for outstanding claims that have been affected. In the interim, DHCS has agreed to provide an advance payment to the Receiver for 80 percent of the total claims affected. The department is also working to correct data entry issues that have prevented certain valid claims from being processed. The state can also retroactively collect federal reimbursement on these claims if and when the errors are corrected, so long as the underlying claims are valid. In addition, DHCS has indicated that it is developing processes to improve quality control (such as developing regular reports on the reasons for rejected claims) and expects to reduce the number of rejected claims in the future.
Problems Result in Greater General Fund Costs. Based on data provided by the Receiver, we estimate that a total of about $21 million in federal matching funds could be obtained for expenditures incurred in 2011–12. As shown in Figure 5, that figure grows to almost $70 million in 2014–15. Our estimates assume that (1) the Receiver is able to secure MOUs with all counties to enroll inmates into their LIHPs, (2) the 2011–12 spending level of $109 million for off–site inpatient services remains relatively stable, and (3) California expands Medi–Cal in 2014, as authorized by the ACA. The growth in potentially available federal funds reflects that (1) many county LIHPs did not take effect (and thus could not enroll inmates) until late in the 2011–12 budget year and (2) the federal match for certain inmates will increase from 50 percent to 100 percent if the state expands Medi–Cal in 2014.
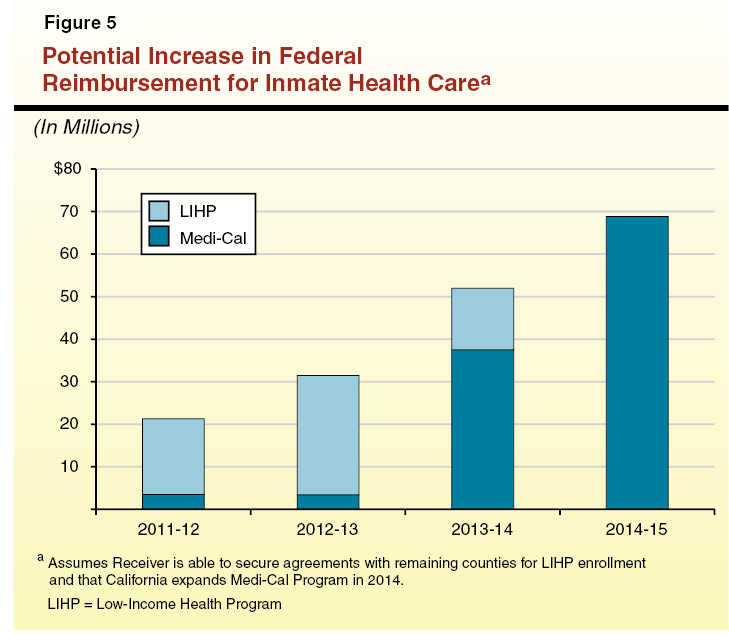
Given that many LIHP counties have not yet entered into MOUs with the Receiver, as well as the data exchange problems with DHCS, only a small portion of the total federal funding that is potentially available has actually been obtained to date. As of December 2012, the Receiver has received a total of $5.1 million in federal reimbursement, including $3.3 million for LIHP eligible inmates and $1.8 million for Medi–Cal eligible inmates. We note that this amount does not include claims that have been submitted and are in the process of being processed. The total thus far received represents less than one–fifth of what we estimate could have been obtained to date without the above problems. Unless these problems are addressed and federal reimbursements are obtained, the General Fund will have to continue to bear these inmate health care costs.
We note that the 2012–13 budget assumed that $45 million in annual savings would be achieved from obtaining federal funds for inmate care in 2012–13 and future years. However, based on recent data provided by the Receiver, it appears that only $30 million will be achievable in 2012–13, and perhaps several millions of dollars less than that if the Receiver is unable to address the issues described above. This means that in order to adhere to the amount budgeted for the inmate medical care program in 2012–13, the Receiver will have to submit a request for additional funding or make some other operational changes in order to achieve savings in some other area of the inmate medical program. In future years, however, if the state is able to address those issues which are currently limiting access to federal funds and the Legislature acts to expand Medi–Cal in 2014, it is likely that annual General Fund savings will exceed $45 million. We estimate that if those issues are satisfactorily resolved, the Legislature could potentially reduce the Receiver’s base budget for the inmate medical care program by an additional $5 million in 2013–14 and almost $25 million in 2014–15.
In 2010–11, DHCS requested, and the Legislature approved, 19 positions for the purposes of processing LIHP and Medi–Cal applications for inmates. Due to subsequent budget reductions, the program was reduced to 17 staff. The Receiver uses the General Fund appropriation provided to his office in the budget to reimburse DHCS for 50 percent of the department’s costs associated with the staff, with the remaining 50 percent of the costs paid by the federal government. The Receiver is estimated to provide DHCS with $650,000 for those positions in the current year. However, recent data on the number of applications received and processed by DHCS, as well as expected changes in the department’s future workload, suggest that the current staffing level is unnecessarily high.
The budget request submitted by DHCS in 2010 overestimated the number of applications the department would receive from the Receiver. Specifically, the budget request estimated that DHCS would receive and be capable of processing approximately 600 applications per month. However, as of September 2012, DHCS has received an average of only about 340 applications per month during the 2012 calendar year and staff are processing applications within an average of 45 days. According to the department, the eligibility determination process has proved to be more time consuming than initially estimated due to complications such as difficulties in verifying the legal residency status for applicants.
There are also a couple of factors that are likely to reduce the department’s future workload. For example, in 2014 the eligibility determination process will be simplified because the department will no longer have to assess eligibility for dozens of county LIHPs with varying eligibility requirements. Instead DHCS will only have to determine eligibility for Medi–Cal, which has uniform statewide eligibility requirements. In addition, there is a provision of the ACA requiring states to use a simplified process for determining Medi–Cal eligibility beginning in 2014. While the state is not expected to finalize its future eligibility determination process until sometime in 2013, it is likely that the new process will further reduce the department’s workload.
In order to ensure that Chapter 729 is fully implemented consistent with legislative intent and that the program is administered as efficiently as possible, we recommend that the Legislature (1) hold budget hearings on status of MOUs between the Receiver and counties to identify and resolve any remaining obstacles preventing the Receiver from securing MOUs with counties to enroll inmates in LIHPs, (2) require DHCS to report on its efforts to address problems that are preventing certain claims for federal reimbursement from being processed, and (3) review DHCS staffing levels and make reductions consistent with their reduced workloads. If the issues preventing the state from maximizing its use of federal funds for inmate health care are resolved, it may also be possible to reduce the Receiver’s budget by $5 million in 2013–14 and more in out years.
Hold Hearings on Status of MOUs Between Receiver and Counties. In passing Chapter 729, the Legislature made clear its intent that counties operating LIHPs enroll state inmates. Given that the majority of counties have thus far not signed MOUs with the Receiver to do so—despite, in some cases, more than one year of negotiations with the Receiver—we recommend that the Legislature provide greater oversight to ensure that its intentions are fulfilled and the state is able to maximize General Fund savings. As mentioned previously, the state risks foregoing a total of $13 million in potential savings over the 2011–12, 2012–13, and 2013–14 fiscal years if the Receiver is unable to secure MOUs with the remaining counties. Specifically, the Legislature could have the Receiver, DHCS, and representatives from counties that have not signed MOUs, report at budget hearings on the status of negotiations.
Depending on the outcome of those hearings, the Legislature has several options to expedite the resolution of outstanding issues that are preventing MOUs from being signed. For example, if the Legislature finds that some counties have legitimate concerns that the reimbursement rate of $10 as adopted in other counties is insufficient to cover their costs, it could direct the Receiver to pay higher rates to those counties. The costs of increasing the reimbursement rate would be relatively insignificant relative to the potential savings. For example, if the rate was doubled to $20 in all of the counties which have not signed MOUs, the total increased cost to the state would be several tens of thousands of dollars, or less than half of 1 percent of the $13 million in savings that are potentially available. On the other hand, raising the rates for the remaining counties might be viewed as unfair by the counties who have already agreed to the $10 reimbursement rate.
Alternatively, if the Legislature finds $10 to be reasonable, it could direct DHCS to exercise its authority under Chapter 729 to prohibit counties from operating LIHPs until they have signed an MOU with the Receiver. This would create a very strong incentive for counties to sign MOUs because failure to do so would result in the loss of federal funds. The amount of lost federal funding would vary depending on the size of the county but could amount to tens of millions of dollars annually in some counties. The Legislature could also amend state law to specify that counties are required to enroll inmates into their LIHPs, if they have one, and that the reimbursement rate shall be $10, or whatever level is deemed appropriate. Such statutory changes would effectively force county cooperation and would expedite the collection of the available federal funding. There is a risk, however, that some counties may claim that the reimbursement rate is insufficient and thus amounts to a state reimbursable mandate that is not fully funded. If they are able to successfully bring a claim to the Commission on State Mandates, the state would have to pay any additional costs that the commission finds are not funded.
Require DHCS to Report on Efforts to Resolve Claiming Issues. According to DHCS, staff are currently working to correct the software and data entry issues that have prevented the state from receiving federal reimbursement for services delivered to Medi–Cal eligible inmates. We recognize that resolving these issues are among many competing priorities that the department currently faces as it attempts to prepare for the full implementation of ACA in 2014. However, failure to remedy this issue is preventing the state from accessing millions of dollars in federal funding. Moreover, if the state chooses to expand Medi–Cal in 2014, the number of Medi–Cal claims, and thus the number of potentially affected claims, will increase dramatically. As such, it is critical that DHCS remedy these issues prior to 2014, and preferably as soon as possible. In order to ensure that the department is on track to resolve these issues, we recommend that the Legislature require DHCS to report at budget hearings on trends in the number of rejected claims, as well as its efforts to prevent the rejection of valid claims.
Review DHCS Staffing Levels. In light of recent data revealing a discrepancy between the number of inmate applications projected to be received and actually received by DHCS to date, as well as expected reductions in the department’s future workload, it is likely that current staffing levels could be reduced. We recommend that the department report at upcoming budget hearings on: (1) recent trends in the number of applications received and processed and (2) the establishment of new rules that will be used for Medi–Cal eligibility determination in 2014 and its assessment of how these rule changes will impact workload. If the department is continuing to receive fewer applications than initially estimated and will likely realize a decrease in workload as a result of changes in the eligibility determination process in 2014, then the Legislature could reduce staffing levels accordingly. Staffing reductions could result in General Fund savings of a couple hundred thousand dollars annually. Our office will assist the Legislature in analyzing materials provided by the department and determining what specific reductions could be made.